 |
|
Back to: Walter Day Conversations
British Journal of Sports Medicine
The "piriformis syndrome"- myth or reality? Link
M T F Read
7 Waterden Road, Guildford, Surrey GU24 0LX, UK
Keywords: piriformis syndrome; sciatic nerve; buttock; hamstring
NOTE: I am not a Doctor, Please speak to your doctor regarding any nerve condition.
In the above editorial,1 I noted the desire to package these rather indeterminate
pains in the buttock, around the trochanter, and which can radiate to the groin
or knee, as a deep gluteal syndrome. The piriformis syndrome and the hamstring
syndrome, I believe exist, but in my admittedly very small experience, as they
are rare, they do have a major clinical finding that differs from pain induced by
the hip stabilizers. Because the sciatic nerve is involved, the straight leg raises,
Laseque and Bowstring signs, which produce neural stress peripheral to the lesion,
are positive, but the slump test, which moves the dura and is proximal to the lesion,
is negative. Most patients diagnosed as having "piriformis syndrome" do not have
these clinical findings, and their problem better fits the classification of deep
gluteal syndrome. Perhaps, in fact, the deep gluteal syndrome diagnosis should be
used as well as, and not inclusive of, the piriformis and hamstring syndromes. I
feel the gluteals are often not involved and perhaps an even broader term such as
hip stabilizer syndrome should be considered.
February 3, 2005 -- New News: In, "The Journal of Neurosurgery Spine", from
studies of UCLA and Cedars Sinai Medical Center in Los Angeles, CA. --
Dr. Aaron Filler, M.D.
Study of Piriformis Syndrome -- Proper Diagnosis now Available:
Institute for Nerve Medicine
Internet:
sjackson@nervemed.com
http://www.nervemed.com
Company Information:
Institute for Nerve Medicine
2716 Ocean Park Blvd.
Suite 3082
Santa Monica, CA 90405
USA
Ph. 310-314-6410
Fx. 310-314-2414
Media Contacts:
Shirlee B. Jackson
Executive Director
310.314.6410
VIDEO AND PHOTOS AVAILABLE: Cedars Sinai Medical Center, UCLA and the Institute for
Nerve Medicine: Breakthrough Medical Findings Provide Answers To Back Pain Sufferers
Revolutionary Medical Report published in the February issue of The Journal of
Neurosurgery: Spine - Findings In A Revolutionary Medical Report From Doctors At UCLA,
Cedars-Sinai Medical Center And The Institute For Nerve Medicine Reveal That New
Technology Better Diagnoses And Treats Back Pain Sufferers With Sciatica
For Immediate Release
LOS ANGELES, Calif./EWORLDWIRE/Feb. 3, 2005 --- In a report that may revolutionize
the treatment of more than a million cases of sciatica (radiating leg pain) each year,
investigators from Cedars Sinai Medical Center, UCLA and the Institute for Nerve Medicine
in Los Angeles, California report today in the Journal of Neurosurgery - Spine that new
technology can accomplish the reliable effective diagnosis and treatment of piriformis
syndrome and other causes of sciatica that do not involve a herniated lumbar disc.
The paper, entitled: "Sciatica of Non-Disc Origin & Piriformis Syndrome: Diagnosis by MR
Neurography and Interventional MRI with Outcome Study of Resulting Treatment" addresses
the current problem of a nearly 80% failure rate for diagnosis using standard methods.
The study involved 240 patients followed for up to seven years.
The most common cause for sciatica in the study proved to be a diagnosis called "piriformis
syndrome" - one of several disorders the investigators report on that arise due to entrapment
of the sciatic nerve in the area of the hip. Currently, the report says, when a patient
experiences painful persistent sciatica - pain radiating down the leg - physicians often
look only for a herniated lumbar disk relying upon lumbar MRI scanning. Surgery for the
disk herniation is often carried out to treat the sciatica.
Most spine specialist consider piriformis syndrome to be extremely rare. However, the
authors conclude that although it is rarely diagnosed, it is actually a common cause of
sciatica - possibly as common as the well known herniated disk syndromes.
Although 1.5 million lumbar MRI scans are carried out each year for sciatica (at a cost of
about $1.5 billion), only about 300,000 (20%) reveal a herniated disk amenable to surgery.
About 1/3rd of the surgeries fail to relieve the sciatica. As a consequence, about 1.2
million (80%) receive no clear diagnosis and 100,000 have spine surgery that fails.
The new report includes a diagnostic efficacy study showing that MR Neurography (a new
method for imaging the sciatic nerve) has a 93% specificity for identifying piriformis
syndrome. Treatments involved new technology employing Open MRI real time image guidance
for injection therapy as well as a new minimal access outpatient surgery technique. Good
and excellent outcomes were over 80% in a group of patients that typically have extremely
poor outcomes.
For a copy of this breakthrough report, media can e-mail afiller@nervemed.com.
Media interested in interviewing Dr. Aaron Filler, M.D. can call Charles Barrett, The
Barrett Company Communications, in Los Angeles at 310-471-5764 or by cell at 323-595-5941.
HTML: http://newsroom.eworldwire.com/wr/020305/11339.htm
PDF: http://newsroom.eworldwire.com/pdf/020305/11339.pdf
ONLINE NEWSROOM: http://newsroom.eworldwire.com/2290.htm
LOGO: http://newsroom.eworldwire.com/2290.htm
CONTACT:
Charles Barrett
The Barrett Company
12021 Wilshire Blvd. #600
Los Angeles, CA 90025
PHONE. 310-471-5764
FAX. 310-471-5215
EMAIL: barcorpr@earthlink.net
http://www.barrettco.com
Kelli Hanley
Cedars-Sinai Medical Center
8700 Beverly Blvd.
Room 2429A
Los Angeles, CA 90048-1865
PHONE. 310-423-4767
FAX. 310-423-0435
EMAIL: kelli.hanley@cshs.org
http://www.csmc.edu
KEYWORDS: Medicine, Technology, Patents, Neurosurgery, Imaging, Sciatica, Back Pain,
UCLA, Medical Advance
SOURCE: Publicist, Cedars Sinai Medical Center
AVAILABLE MEDIA:
Photo: Sciatica Neurography (size: 271.9 k)
Sciatica Neurography
http://newsroom.eworldwire.com/media_uploads/2290_998081_1107384865.jpg
Click for full-size
Photo: Piriformis Injection (size: 295.6 k)
Open MR Guided Injection
http://newsroom.eworldwire.com/media_uploads/2290_649103_1107384903.jpg
Click for full-size
Video Clip: Press Release Highlights (size: 3.0 k)
Report Findings Published
http://newsroom.eworldwire.com/media_uploads/institute4nervemed_020205.wmv
This is the personal web page of Paul Dean, Piriformis Syndrome Sufferer:
disclaimer: I am not a doctor and do not claim anything except that there
are many problems people have in getting the proper treatment for Piriformis
Syndrome.
The below information to bring about more awareness of Piriformis Syndrome
with description and links as well as Paul Dean's diagnosis and treatment in
trying to recover from this rare condition which many doctors have overlooked
in Paul Dean's recovery process. You will find many conflicting Doctors
recovery plans because every Doctor has their own research and their own
ideas on what Piriformis Syndrome is and how to treat it.
Terms:
The Disk: Dense tissue between the vertebrae that acts as a shock absorber
and prevents damage to nerves and blood vessels along the spine.
Electromyography: A medical test in which a nerve's ability to conduct
an impulse is measured.
Lumbosacral: Referring to the lower part of the backbone or spine.
Myelography: A medical test in which a special dye is injected into a nerve
to make it visible on an x ray.
Piriformis: A muscle in the pelvic girdle that is closely associated with
the sciatic nerve.
Radiculopathy: A condition in which the spinal nerve root of a nerve has been
injured or damaged.
Spasm: Involuntary contraction of a muscle.
Vertebrae: The component bones of the spine.
Where is the Piriformis Muscle?
In non medical terms, it would be the middle of the buttocks cheek, and very deep.
Piriformis Syndrome: Sciatica, and Back Pain.
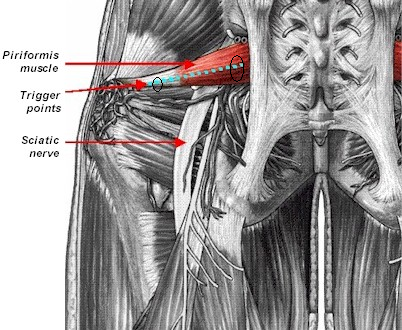
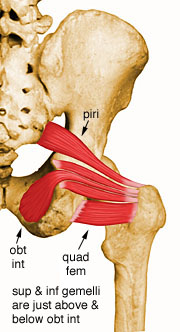
Located deep in the hip underneath the Glutes are the 'Deep Six' lateral rotators
of the leg; Gemellus Superior and Inferior, Obturator Internus and Externus, Quadratus
Femoris, and last but not least, the (Piriformis). The Deep Six not only rotate and
stabilize the legs, they also play an important role in pelvic balance. If one hip
is tight then the pelvis will be pulled to the side and rotated causing an imbalance
in the lower back. If both hips are tight then pelvic movement becomes restricted and
the lower back has to contend with the torsion created. Trigger points in the Deep Six
can refer pain into the legs and pelvis and can contribute to other dysfunction such
as 'Restless Leg Syndrome'. One leg or both will usually be rotated outwards and the
joint compressed contributing significantly to arthritic hip joints as well as problems
with the knees and ankles.
There are many medical ideas on what Piriformis Syndrome is and how to fix it,
and it is an ongoing problem in diagnosis and agreement of treatment as you
will see below. Every body is different and there can be many different
variations of the problem in piriformis syndrome so treatment will have to
vary per the individual case by case study.
Where is the pain?
If it lies deep in the buttock and follows down the leg then you may have
sciatica, from a Piriformis Syndrome Condition. Link
Sciatica
The largest nerve in your body has a very devious twist--and when you have a pain
in that nerve, it can really get around.
Sciatica, pain in the sciatic nerve, can radiate from the buttocks down the back
of the leg to the knee, even as far as the big toe. "People with sciatica often say
their back pain is bad but their leg pain is worse," says Loren M. Fishman, M.D., a
physiatrist and rehabilitation medicine specialist at Flushing Hospital Medical Center
in New York City. Often the hip pain is far more severe on one side than the other.
When you've got pain like that, you'll need a hands-on diagnosis before anything else,
Dr. Fishman says. Once the doctor has ruled out a disk problem or fracture, he may be
able to find out whether tight buttocks muscles are causing your pain by compressing
the sciatic nerve.
If you do have sciatica, the doctor will probably recommend a program of supervised
exercises.
Rashad Net University
Post traumatic piriformis syndrome Link
It is postulated by several investigators that sciatica may be secondary to an
aberrant relationship between the piriformis muscle and the sciatic nerve. Pace
and Nagle describe a diagnostic maneuver that is now referred to as Pace's sign-pain
and weakness in association with resisted abduction and external rotation of the
affected thigh.
gluteal atrophy, depending on the duration of the condition. The piriformis syndrome
is thought to occur after blunt trauma to the buttocks. A hematoma forms and scarring
occurs between the sciatic nerve and the short external rotators. Patients who have a
history of this type of trauma and typical findings on physical examination, and
intractable pain after conservative treatment will benefit from release of the piriformis
tendon and sciatic neurolysis.
The authors report the operative treatment and outcome in fifteen cases of piriformis
syndrome (in 14 patients) all patients had blunt trauma to the buttocks. They all
underwent operative release of the piriformis tendon and sciatic neurolysis. The
patients had an average delay of 32 months from the time of injury to the surgery.
Intraoperative findings revealed adhesions between the piriformis muscle, the sciatic
nerve, and the roof of the greater sciatic notch. At twenty-four months all patients
had excellent and four good results from the surgery. All had returned to work.
If conservative treatment has failed a nerve conduction test and referral to an
experience hip surgeon who is familiar with the syndrome is necessary. Note: In the
case of myself, and my occurrence of piriformis syndrome I sought the help of a
Neurosurgeon.
============================================================================
Piriformis Muscle and Blunt Injury Adhesions Link
============================================================================
As mentioned earlier, the sciatic is not the only nerve that may get compressed
in this region. Pressure may be placed on the superior gluteal nerve between
the piriformis muscle and the greater sciatic notch. The piriformis muscle
may also compress the inferior gluteal nerve, either with fibrous bands in
the muscle or with pressure against the sacrospinous ligament.
The pressure on nerves in piriformis syndrome is usually from a hypertonic
piriformis muscle, but it may also occur from external pressure, such as sitting
on a wallet. There are also reports of piriformis syndrome occurring from a
direct blow to the buttock area, (fall injury trauma). As a result of
the blunt trauma, adhesions may develop between the piriformis muscle, the
sciatic nerve and the roof of the greater sciatic notch.
Myofascial trigger points in the piriformis or other gluteal muscles may play
an important role in piriformis syndrome. Piriformis trigger points will often
perpetuate muscle tightness, leading directly to nerve compression. Trigger
points in the gluteus minimus are known to reproduce "sciatica-like pain.
Furthermore, sacroiliac joint dysfunction may perpetuate trigger pointymptoms
and may easily be confused with nerve entrapment by the piriformis muss in
the piriformis muscle and increase the likelihood of nerve compression. A
sudden load placed on the sacroiliac region or the piriformis muscle - from
a fall on the stairs, for example - is often the initial cause of perpetual
trigger-point problems. The constant hypertonicity may then lead to nerve
compression.
"trigger points perpetuate muscle tightness, forcing nerve compression"
============================================================================
The Journal of Bone & Joint Surgery
Excellence Through Peer Review
Sciatica
Sciatica is a condition involving impaired movement and/or sensation in the leg,
caused by damage to the sciatic nerve.
Piriformis syndrome is estimated to cause 6-8% of sciatica, but is more common
in the general population because it has been under diagnosed and under treated.
Information about Sciatica
Sciatica is a form of peripheral neuropathy. It occurs when there is damage to
the sciatic nerve, located in the back of the leg. This nerve controls the muscles
of the back of the knee and lower leg and provides sensation to the back of the
thigh, part of the lower leg and the sole of the foot. Incomplete damage to the
sciatic nerve may appear identical to damage to one of the branches of the sciatic
nerve (tibial nerve dysfunction or common peroneal nerve dysfunction).
A problem in a single nerve group, such as the sciatic nerve, is classified as a
mononeuropathy. The usual causes are direct trauma (often due to an injection into
the buttocks), prolonged external pressure on the nerve, and pressure on the nerve
from nearby body structures. It can also be caused by entrapment -- pressure on the
nerve where it passes through a narrow structure. The damage slows or prevents
conduction of impulses through the nerve.
The sciatic nerve is commonly injured by fractures of the pelvis, gunshot wounds,
or other trauma to the buttocks or thigh. Prolonged sitting or lying with pressure
on the buttocks may also injure it. Systemic diseases, such as diabetes, can
typically damage many different nerves, including the sciatic nerve. The sciatic
nerve may also be harmed by pressure from masses such as a tumor or abscess, or
by bleeding in the pelvis.
In many cases, no cause can be identified.
Note: A ruptured lumbar disk in the spine may cause symptoms that simulate the
symptoms of sciatic nerve dysfunction.
Symptoms
Chronic pain may arise from more than just compression on the nerve. According
to some pain researchers, physical damage to a nerve is only half of the equation.
A developing theory proposes that some nerve injuries result in a release of
neurotransmitters and immune system chemicals that enhance and sustain a pain
message. Even after the injury has healed, or the damage has been repaired, the
pain continues. Control of this abnormal type of pain is difficult. Link
Diagnosis of Sciatica
Before treating sciatic pain, as much information as possible is collected. The
individual is asked to recount the location and nature of the pain, how long it
has continued, and any accidents or unusual activities prior to its onset. This
information provides clues that may point to back strain or injury to a specific
location. Back pain from disk disease, piriformis syndrome, and back strain must
be differentiated from more serious conditions such as cancer or infection. Lumbar
stenosis, an overgrowth of the covering layers of the vertebrae that narrows the
spinal canal, must also be considered. The possibility that a difference in leg
lengths is causing the pain should be evaluated; the problem can be easily be
treated with a foot orthotic or built-up shoe.
Often, a straight-leg-raising test is done, in which the person lies face upward
and the health- care provider raises the affected leg to various heights. This
test pinpoints the location of the pain and may reveal whether it is caused by
a disk problem. Other tests, such as having the individual rotate the hip joint,
assess the hip muscles. Any pain caused by these movements may provide information
about involvement of the piriformis muscle, and piriformis weakness is tested with
additional leg-strength maneuvers.
Further tests may be done depending on the results of the physical examination
and initial pain treatment. Such tests might include magnetic resonance imaging
(MRI) and computed tomography scans (CT scans). Other tests examine the conduction
of electricity through nerve tissues, and include studies of the electrical activity
generated as muscles contract (electromyography), nerve conduction velocity, and
evoked potential testing. A more invasive test involves injecting a contrast substance
into the space between the vertebrae and making x-ray images of the spinal cord
(myelography), but this procedure is usually done only if surgery is being considered.
All of these tests can reveal problems with the vertebrae, the disk, or the nerve
itself.
If the pain is chronic and conservative treatment fails, surgery to repair a herniated
disk or cut out part or all of the piriformis muscle may be suggested, particularly
if there is neurological evidence of nerve or nerve-root damage.
Sciatica Following a Fall 1
continued Link
It is thought that acute or chronic injury causes swelling of the piriformis
muscle and irritates the sciatic nerve, resulting in sciatica. Patients with
an aberrant course of the nerve through the muscle are particularly predisposed
to this condition.
Answer: Piriformis syndrome secondary to myositis ossificans of the
piriformis muscle.
Discussion
Piriformis syndrome is usually a diagnosis of exclusion once the more common
causes of sciatica have been ruled out2. Yoeman3 is credited as being the first
author to have described entrapment of the sciatic nerve by the piriformis muscle.
Freiberg and Vinke4,5 further defined the condition and described what is known
as the Freiberg sign (pain caused by passive internal rotation of the extended
thigh). Beaton and Anson6 described four anatomical variations in the relationship
between the piriformis muscle and the sciatic nerve and implicated these variations
as a cause of compression and inflammation of the sciatic nerve.
The diagnosis often can be made on the basis of a careful clinical evaluation2,
7-10. Physical findings that suggest compression of the sciatic nerve by the
piriformis muscle include tenderness over the sciatic notch, isolated atrophy
of the gluteus maximus, dysesthesia of the posterior aspect of the thigh, and
tenderness of the rectal wall with or without a sausage-shaped mass that is
felt laterally during a rectal examination11. Additional findings that are
indicative of such compression include the Freiberg sign4,5
============================================================================
The Piriformis Syndrome Link
By September Nelson
--------------------------------------------------------------------------------
Introduction. Not all low back, hip, and gluteal (buttock) pain are manifestations
of back injury. Pain in any of these areas may indicate injury or irritation of
any one of a number of muscles and nerves surrounding the low back and hip. Injury
to any of these structures can result in pain and loss of function. A specific
muscle that is susceptible to injury and inflammation is the piriformis muscle.
Due to the location of this muscle, the sciatic nerve is often involved with
piriformis problems. Pain and dysfunction resulting from piriformis injury is
referred to as piriformis syndrome. The symptoms of this disorder sometimes mimic
those of a bulging lumbar disc, or similar low back injury. Therefore, diagnosis
of pain in the low back, gluteal, or hip region should include an evaluation of
the piriformis muscle (PM), other hip musculature, and surrounding nerves.
Anatomy and Function. The piriformis muscle is located deep in the gluteal region.
This muscle attaches to the sacrum and the lateral portion of the upper part of the
femur. It is one part of a group of muscles whose actions include abduction (moving
the thigh away from the midline) and external rotation of the thigh (turning the
knee and toes outward). These muscles are important in maintaining stability of
the hip in all weight bearing activities.
References.
(1) Julsrud, M. E. (1989). Piriformis syndrome. Journal of the American
Podiatric Medical Association, 79, 128-131.
(2) Chen, W. S. (1992). Sciatica due to piriformis pyomyositis. The Journal
of Bone and Joint Surgery, 74-A, 1546-1548.
(3) Vandertop, W. P., and Bosma, N. J. (1991). The piriformis syndrome. The
Journal of Bone and Joint Surgery, 73-A, 1095-1097.
(4) Keskula, D. R. and Tamburello, M. (1992). Conservative management of
piriformis syndrome. Journal of Athletic Training, 27, 102-108.
(5) Barton, P. (1991). Piriformis syndrome: a rational approach to management.
Pain, 47, 345-352.
============================================================================
Acupuncture Today
May, 2002, Volume 03, Issue 05
Treatment of Piriformis Syndrome Pain: Acupuncture Link
=============================================================================
Dr. Katz's Corner
Alejandro J. Katz, MD, OMD, LAC, QME
Treatment of Piriformis Syndrome Pain
Some of the cases termed "lower back pain" are in reality piriformis syndrome.
In piriformis syndrome, the piriformis muscle gets tight (due to overstretching,
trauma, prolonged bad posture, etc.) and compresses the sciatic nerve, producing
numbness and pain going down the thigh and calf (UB channel). If the compression
is on the inferior gluteal nerve (a branch of the sciatic nerve), the pain will
be in the buttock (local symptoms).
Piriformis Trigger Points /Acupuncture
 When the initial examination takes place, it is very common to see the patient
leaning toward the other side (when sitting or standing) in order to reduce the
compression of the sciatic nerve. The great majority of these patients are taking
medications - for example, 800 milligrams of ibuprofen (Motrin) three times a
day, or 500 milligrams of naproxen two times a day - with little or no improvement.
The examination of the affected area begins with moderate digital palpation of
GB 30 and moves toward the midline. A series of trigger points will be discovered
that, when palpated, will produce local and/or referred pain (referred pain/
tingling toward the buttock and/or leg [UB channel]).
Technique used: Chinese acupuncture needles (gauge #36), 1.5-2 inches long.
Micro-current device: Acutron Mentor, biphasic milliamp pads, with milliamp
stimulation for 20 minutes (milliamp stimulation is maintained as a noticeable,
mild tingling sensation). A second stage follows: a cooling period of five minutes
(micro amp stimulation, biphasic, 75-100 micro-amps).
Treatment points: GB 30 is connected to 2-4 trigger areas on top of the piriformis
muscle.
The treatment frequency is 1-3 times a week (depending on the pain level) for 4-6
weeks. The acupuncture needles are inserted with the stimulation pads on top of
the needles (the pads used are Zimmer, single use).
Within 6-8 treatments, the patient is able to feel improvement: pain/burning and
tingling is reduced; the range of motion of the hip is increased; and pain medication
reduced or discontinued.
As in almost all muscle disorders, the indication of the appropriate stretching
exercises for the muscles involved will assist in a speedy recovery. A course
of daily stretching exercises is recommended (part of the protocol) to patients
to assist in recovery of the muscles and tendons. Targeting the piriformis is
done with a single knee to the chest with painful side cross-over. The stretching
exercises are performed three times a day, five times each time, maintaining the
stretch between 5-10 seconds. It is convenient to apply heat for 15 to 20 minutes
before the stretching exercises are done in order to increase the elasticity of
the muscle, and ice for five minutes afterward in order to reduce the inflammation
produced by the stretching exercises.
Other treatments: Posture training is another pillar of patient rehabilitation.
In some cases, a cortisone injection is administered locally to reduce the inflammation
and edema of the muscle. Surgery is another resource (although rarely used): it
"cleans up" the fibrotic muscle.
If you have any questions about the treatment described in this article, please
contact me at the address below.
Alejandro J. Katz, MD, OMD, LAc, QME
Los Angeles, California
tvstardr@aol.com
www.drkatz.org
============================================================================
When the initial examination takes place, it is very common to see the patient
leaning toward the other side (when sitting or standing) in order to reduce the
compression of the sciatic nerve. The great majority of these patients are taking
medications - for example, 800 milligrams of ibuprofen (Motrin) three times a
day, or 500 milligrams of naproxen two times a day - with little or no improvement.
The examination of the affected area begins with moderate digital palpation of
GB 30 and moves toward the midline. A series of trigger points will be discovered
that, when palpated, will produce local and/or referred pain (referred pain/
tingling toward the buttock and/or leg [UB channel]).
Technique used: Chinese acupuncture needles (gauge #36), 1.5-2 inches long.
Micro-current device: Acutron Mentor, biphasic milliamp pads, with milliamp
stimulation for 20 minutes (milliamp stimulation is maintained as a noticeable,
mild tingling sensation). A second stage follows: a cooling period of five minutes
(micro amp stimulation, biphasic, 75-100 micro-amps).
Treatment points: GB 30 is connected to 2-4 trigger areas on top of the piriformis
muscle.
The treatment frequency is 1-3 times a week (depending on the pain level) for 4-6
weeks. The acupuncture needles are inserted with the stimulation pads on top of
the needles (the pads used are Zimmer, single use).
Within 6-8 treatments, the patient is able to feel improvement: pain/burning and
tingling is reduced; the range of motion of the hip is increased; and pain medication
reduced or discontinued.
As in almost all muscle disorders, the indication of the appropriate stretching
exercises for the muscles involved will assist in a speedy recovery. A course
of daily stretching exercises is recommended (part of the protocol) to patients
to assist in recovery of the muscles and tendons. Targeting the piriformis is
done with a single knee to the chest with painful side cross-over. The stretching
exercises are performed three times a day, five times each time, maintaining the
stretch between 5-10 seconds. It is convenient to apply heat for 15 to 20 minutes
before the stretching exercises are done in order to increase the elasticity of
the muscle, and ice for five minutes afterward in order to reduce the inflammation
produced by the stretching exercises.
Other treatments: Posture training is another pillar of patient rehabilitation.
In some cases, a cortisone injection is administered locally to reduce the inflammation
and edema of the muscle. Surgery is another resource (although rarely used): it
"cleans up" the fibrotic muscle.
If you have any questions about the treatment described in this article, please
contact me at the address below.
Alejandro J. Katz, MD, OMD, LAc, QME
Los Angeles, California
tvstardr@aol.com
www.drkatz.org
============================================================================
Description of Problem:
----------
1: Pain. 1991 Dec;47(3):345-52. Related Articles, Link
Piriformis syndrome: a rational approach to management.
 Barton PM.
Department of Physical Medicine and Rehabilitation, University of Western Ontario,
London, Canada.
Although rarely recognized, the piriformis syndrome appears to be a common cause of
buttock and leg pain as a result of injury to the piriformis muscle. Four cases
representing a broad spectrum of presentations are described here. The major findings
include buttock tenderness extending from the sacrum to the greater trochanter and
piriformis tenderness on rectal or pelvic examination. Symptoms are aggravated by
prolonged hip flexion, adduction, and internal rotation, in the absence of low back
or hip findings. Minor findings may include leg length discrepancy, weak hip abductors,
and pain on resisted hip abduction in the sitting position. Myofascial involvement of
related muscles and lumbar facet syndromes may occur concurrently. The diagnosis is
primarily clinical as no investigations have proved definitive. The role of MRI of the
piriformis muscle is assessed and other investigative tools are discussed. A rational
management schema is demonstrated: (1) underlying biomechanical factors and associated
conditions should be corrected; (2) the patient is instructed in a home program of
prolonged piriformis muscle stretching which may be augmented in physical therapy by
preceding ultrasound or Fluori-Methane (dichlorodifluoromethane and trichloromono
fluoromethane spray); (3) a trial of up to three steroid injections is attempted;
and (4) if all these measures fail, consideration should be given to surgical sciatic
nerve exploration and piriformis release.
Piriformis Muscle Injection: LinkLidocaine is usually used
The piriformis muscle is a relatively small structure located as far as eight
inches below the surface of the buttock. If a blind injection misses the muscle,
the injection test is meaningless. Immediately deep to the piriformis muscle is
the sciatic nerve and the colon so misplacement of the needle may lead to significant
complications. The use of Open MRI image guidance makes this a safe reliable and
accurate procedure. In these images, the physician's finger is seen indicating
the angle of approach in the first image. In subsequent views, local anaesthetic
is injected in the skin and then a titanium Lufkin needle is introduced and
advanced into the piriformis muscle. An injection of Marcaine (10 cc of 0.5%
solution of this long acting local anesthetic) and Celestone (1cc of this
steroid medication) is then seen darkening the interior of the muscle in the
last two image frames. These flash MRI images each take about 12 seconds to
complete. In about 20% of cases the injection is therapeutic and the piriformis
syndrome resolves completely and permanently. In others, the injection needs to
repeated in a few months, and in still others, it last only a few days. In this
category, surgery may be required to maintain the pain relief. Piriformis surgery
is now a small procedure which can be carried out under local anesthetic as an
outpatient.
----------
What is Piriformis Syndrome?
Piriformis syndrome is a rare neuromuscular disorder that occurs when the piriformis
muscle compresses or irritates the sciatic nerve-the largest nerve in the body. The
piriformis muscle is a narrow muscle located in the buttocks. Compression of the
sciatic nerve causes pain-frequently described as tingling or numbness-in the buttocks
and along the nerve, often down to the leg. The pain may worsen as a result of sitting
for a long period of time, climbing stairs, walking, or running.
Piriformis syndrome can develop when the piriformis muscle becomes tight or spasms
and places pressure on the sciatic nerve that runs beneath it. The pressure on the
sciatic nerve can cause low back pain and/or pain that radiates to the rear and
down the leg (similar to sciatica pain). From a technical standpoint, piriformis
syndrome does not cause true sciatica (as sciatica is usually defined as a
radiculopathy, or compression of a nerve root as it exits the spine). However, just
like sciatica, piriformis syndrome can cause pain, numbness and tingling along the
sciatic nerve, which runs down the back of the leg and into the foot.
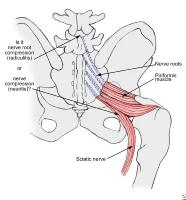
Piriformis Syndrome is caused by an entrapment (pinching)
of the sciatic nerve as
it exits the Greater Sciatic notch in the gluteal region.
History: Piriformis syndrome often is not recognized as a cause of LBP and
associated sciatica. This clinical syndrome is due to a compression of the
sciatic nerve by the piriformis muscle. The patient with an unrelenting
sciatica may be suffering with a piriformis syndrome.
This syndrome is considered an entrapment
neuropathy caused by pressure on
the sciatic nerve by an enlarged or inflamed piriformis muscle. The sciatic
nerve can be compressed between the swollen muscle fibers and the bony pelvis.
Causes: Approximately 50%
of patients with piriformis syndrome have a history
of trauma, with either a direct buttock contusion or hip/lower back torsional
injury. The remaining 50% of cases are of spontaneous onset, so the treating
physician must have a high index of suspicion for this problem, lest it be overlooked.
Dr. Stephen M. Pribut's Sport Pages
Sports Medicine
December 11, 2004
Piriformis Syndrome: The Big Mystery or A Pain In The Behind
by Stephen M. Pribut, DPM and Amelia Perri-Pribut, B.S., R.N., M.B.A.
Superior and Inferior Gluteal Region
Barton PM.
Department of Physical Medicine and Rehabilitation, University of Western Ontario,
London, Canada.
Although rarely recognized, the piriformis syndrome appears to be a common cause of
buttock and leg pain as a result of injury to the piriformis muscle. Four cases
representing a broad spectrum of presentations are described here. The major findings
include buttock tenderness extending from the sacrum to the greater trochanter and
piriformis tenderness on rectal or pelvic examination. Symptoms are aggravated by
prolonged hip flexion, adduction, and internal rotation, in the absence of low back
or hip findings. Minor findings may include leg length discrepancy, weak hip abductors,
and pain on resisted hip abduction in the sitting position. Myofascial involvement of
related muscles and lumbar facet syndromes may occur concurrently. The diagnosis is
primarily clinical as no investigations have proved definitive. The role of MRI of the
piriformis muscle is assessed and other investigative tools are discussed. A rational
management schema is demonstrated: (1) underlying biomechanical factors and associated
conditions should be corrected; (2) the patient is instructed in a home program of
prolonged piriformis muscle stretching which may be augmented in physical therapy by
preceding ultrasound or Fluori-Methane (dichlorodifluoromethane and trichloromono
fluoromethane spray); (3) a trial of up to three steroid injections is attempted;
and (4) if all these measures fail, consideration should be given to surgical sciatic
nerve exploration and piriformis release.
Piriformis Muscle Injection: LinkLidocaine is usually used
The piriformis muscle is a relatively small structure located as far as eight
inches below the surface of the buttock. If a blind injection misses the muscle,
the injection test is meaningless. Immediately deep to the piriformis muscle is
the sciatic nerve and the colon so misplacement of the needle may lead to significant
complications. The use of Open MRI image guidance makes this a safe reliable and
accurate procedure. In these images, the physician's finger is seen indicating
the angle of approach in the first image. In subsequent views, local anaesthetic
is injected in the skin and then a titanium Lufkin needle is introduced and
advanced into the piriformis muscle. An injection of Marcaine (10 cc of 0.5%
solution of this long acting local anesthetic) and Celestone (1cc of this
steroid medication) is then seen darkening the interior of the muscle in the
last two image frames. These flash MRI images each take about 12 seconds to
complete. In about 20% of cases the injection is therapeutic and the piriformis
syndrome resolves completely and permanently. In others, the injection needs to
repeated in a few months, and in still others, it last only a few days. In this
category, surgery may be required to maintain the pain relief. Piriformis surgery
is now a small procedure which can be carried out under local anesthetic as an
outpatient.
----------
What is Piriformis Syndrome?
Piriformis syndrome is a rare neuromuscular disorder that occurs when the piriformis
muscle compresses or irritates the sciatic nerve-the largest nerve in the body. The
piriformis muscle is a narrow muscle located in the buttocks. Compression of the
sciatic nerve causes pain-frequently described as tingling or numbness-in the buttocks
and along the nerve, often down to the leg. The pain may worsen as a result of sitting
for a long period of time, climbing stairs, walking, or running.
Piriformis syndrome can develop when the piriformis muscle becomes tight or spasms
and places pressure on the sciatic nerve that runs beneath it. The pressure on the
sciatic nerve can cause low back pain and/or pain that radiates to the rear and
down the leg (similar to sciatica pain). From a technical standpoint, piriformis
syndrome does not cause true sciatica (as sciatica is usually defined as a
radiculopathy, or compression of a nerve root as it exits the spine). However, just
like sciatica, piriformis syndrome can cause pain, numbness and tingling along the
sciatic nerve, which runs down the back of the leg and into the foot.
Piriformis Syndrome is caused by an entrapment (pinching)
of the sciatic nerve as
it exits the Greater Sciatic notch in the gluteal region.
History: Piriformis syndrome often is not recognized as a cause of LBP and
associated sciatica. This clinical syndrome is due to a compression of the
sciatic nerve by the piriformis muscle. The patient with an unrelenting
sciatica may be suffering with a piriformis syndrome.
This syndrome is considered an entrapment
neuropathy caused by pressure on
the sciatic nerve by an enlarged or inflamed piriformis muscle. The sciatic
nerve can be compressed between the swollen muscle fibers and the bony pelvis.
Causes: Approximately 50%
of patients with piriformis syndrome have a history
of trauma, with either a direct buttock contusion or hip/lower back torsional
injury. The remaining 50% of cases are of spontaneous onset, so the treating
physician must have a high index of suspicion for this problem, lest it be overlooked.
Dr. Stephen M. Pribut's Sport Pages
Sports Medicine
December 11, 2004
Piriformis Syndrome: The Big Mystery or A Pain In The Behind
by Stephen M. Pribut, DPM and Amelia Perri-Pribut, B.S., R.N., M.B.A.
Superior and Inferior Gluteal Region
 "...The existence of piriformis syndrome has been doubted for years."
Piriformis syndrome may overlap with a variety of other problems including what
McCrory et. al. have called a "deep buttock" syndrome. This includes pain in the
buttock region, possibly pain in the hamstrings, occasionally pain in the back
of the leg that is difficult to locate. Link
These symptoms of the piriformis muscle dysfunction may be caused by other
clinical entities that include gluteus medius dysfunction, herniated or bulging
disks, "sciatica" and other musculoskeletal problems in this area. Scant information
is available on the piriformis syndrome in lay publications, and only a little
more in scientific publications. The functioning of the muscle has not been clearly
defined and examined in the literature. The location of the muscle does not allow
for surface EMG (electromyographical) study. It is quite difficult, if not impossible
to place a deep electrode in the muscle for study purposes also.
Anatomically, the piriformis muscle lies deep to the gluteal muscles. It originates
from the sacral spine and attaches to the greater trochanter of the femur, which is
the big, bony "bump" on the outside top of the thigh. The sciatic nerve usually passes
underneath the piriformis muscle, but in approximately 15% of the population, it
travels through the muscle. It is thought that acute or chronic injury causes swelling
of the muscle and irritates the sciatic nerve, resulting in sciatica. Patients with
an aberrant course of the nerve through the muscle are particularly predisposed to
this condition.
The piriformis syndrome is diagnosed primarily on the basis of symptoms and on the
physical exam. There are no tests that accurately confirm the diagnosis, but X-rays,
MRI, and nerve conduction tests may be necessary to exclude other diseases. Some of
the other causes of sciatica include disease in the lumbar spine (e.g. disc herniation)
chronic hamstring tendonitis, and fibrous adhesions of other muscles around the
sciatic nerve.
Once properly diagnosed, treatment is undertaken in a stepwise approach. Initially,
progressive piriformis stretching is employed, starting with 5 seconds of sustained
stretch and gradually working up to 60 seconds. This is repeated several times
throughout the day. It is important that any abnormal biomechanical problems, such
as overpronation of the foot or other coexisting conditions, are treated. This
stretching can be combined with physical therapy modalities such as ultrasound.
If these fail, then injections of a corticosteroid into the piriformis muscle may
be tried. Finally, surgical exploration may be undertaken as a last resort.
-----------------------------------------------------------------------------------
"...The existence of piriformis syndrome has been doubted for years."
Piriformis syndrome may overlap with a variety of other problems including what
McCrory et. al. have called a "deep buttock" syndrome. This includes pain in the
buttock region, possibly pain in the hamstrings, occasionally pain in the back
of the leg that is difficult to locate. Link
These symptoms of the piriformis muscle dysfunction may be caused by other
clinical entities that include gluteus medius dysfunction, herniated or bulging
disks, "sciatica" and other musculoskeletal problems in this area. Scant information
is available on the piriformis syndrome in lay publications, and only a little
more in scientific publications. The functioning of the muscle has not been clearly
defined and examined in the literature. The location of the muscle does not allow
for surface EMG (electromyographical) study. It is quite difficult, if not impossible
to place a deep electrode in the muscle for study purposes also.
Anatomically, the piriformis muscle lies deep to the gluteal muscles. It originates
from the sacral spine and attaches to the greater trochanter of the femur, which is
the big, bony "bump" on the outside top of the thigh. The sciatic nerve usually passes
underneath the piriformis muscle, but in approximately 15% of the population, it
travels through the muscle. It is thought that acute or chronic injury causes swelling
of the muscle and irritates the sciatic nerve, resulting in sciatica. Patients with
an aberrant course of the nerve through the muscle are particularly predisposed to
this condition.
The piriformis syndrome is diagnosed primarily on the basis of symptoms and on the
physical exam. There are no tests that accurately confirm the diagnosis, but X-rays,
MRI, and nerve conduction tests may be necessary to exclude other diseases. Some of
the other causes of sciatica include disease in the lumbar spine (e.g. disc herniation)
chronic hamstring tendonitis, and fibrous adhesions of other muscles around the
sciatic nerve.
Once properly diagnosed, treatment is undertaken in a stepwise approach. Initially,
progressive piriformis stretching is employed, starting with 5 seconds of sustained
stretch and gradually working up to 60 seconds. This is repeated several times
throughout the day. It is important that any abnormal biomechanical problems, such
as overpronation of the foot or other coexisting conditions, are treated. This
stretching can be combined with physical therapy modalities such as ultrasound.
If these fail, then injections of a corticosteroid into the piriformis muscle may
be tried. Finally, surgical exploration may be undertaken as a last resort.
-----------------------------------------------------------------------------------
 Piriformis Stretch
The gentle Piriformis Stretch:
Place the right knee on the ground roughly in line with your
left shoulder The right foot should be just in front of the
left knee Press your hips towards the ground so that your
bodyweight is on your right leg. As you move down the right
knee comes closer to the left shoulder.
You should feel a gentle pull deep in the right hip / buttocks.
-----------------------------------------------------------------------------------
A good sports medicine physician with experience in caring for athletes with the
piriformis syndrome can help direct appropriate management. With proper diagnosis
and treatment, there is no reason for this syndrome to be dreaded. Good luck and
good training.
last update - 2/97
Diagnosis:
The symptoms most often reported are pain when running or walking in the gluteal
region. Pain may go down the back of the leg. Dyspareunia is sometimes noted.
Having the patient lie down, flex the knee to 10 - 20 degrees and then have the
patient attempt to externally rotate the leg against resistance. Pain may occur
with piriformis tendonitis. Direct tenderness will be found in the region of the
piriformis tendon over the buttock region.
If there is a positive test to the straight leg lift (causing sciatica like pain),
externally rotate the leg to see if this lessens the pain. This could indicate
compression of the sciatic nerve by the piriformis.
Be certain to examine the sacroiliac joint also.
Treatment:
Rest is usually recommended. A two to three week break from the sports and activities
that cause pain can be very helpful. Relative rest, meaning less intense workouts,
and fewer miles is also helpful, and should be used during your return to activity.
Like Achilles tendonitis and iliopsoas tendonitis this is a very difficult problem
to eliminate.
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the course
of the sciatic nerve. This referred pain, called "sciatica", often goes down the
back of the thigh and/or into the lower back. Patients generally complain of pain
deep in the buttocks, which is made worse by sitting, climbing stairs, or performing
squats.
The anatomical position of the muscle leads one to conclude that it functions in
some ways similar to that of the gluteus medius. The major portion of origin of the
piriformis is the anterior lateral portion of the sacrum and the insertion is on the
upper portion of the femur.
It can be seen that the sciatic nerve passes immediately below the piriformis muscle.
The first places the sciatic nerve inferior (below) to the Piriformis muscle and
superior (above) the gemellus muscle. Entrapment in this area is likely due to a
myospasm or contracture (tightening or shortening respectively) of either of these
two muscles. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
This particular syndrome can often mimic its more notorious counterpart known as
sciatica, and that being the case, it is often misdiagnosed as sciatica. The main
difference between sciatica and piriformis syndrome is in the cause. Sciatica is
directly due to a lumbar disc pressing on the sciatic nerve as it exits the intervertebral
foramen in the lumbar spine. What both of these complaints have in common is that
both can produce pain, numbness and tingling below the knee and into the foot.
Link to below article:
In the United States each year, 1.5 million people have lumbar MRI scans to look
for the cause of the buttock and leg pain called 'sciatica'. More than 1.2 million
of those scans fail to find the cause in the spine. Three hundred thousand of the
scans are sufficiently positive that the patient has lumbar spine surgery. Of the
300,000 surgeries, as many as 25% fail to relieve the pain - in many cases this
is because the diagnosis of a spinal cause for the sciatica was incorrect.
October 13, 2004
Piriformis Syndrome: The Big Mystery or A Pain In The Behind
by Stephen M. Pribut, DPM and
Amelia Perri-Pribut, B.S., R.N., M.B.A.
Piriformis syndrome is difficult to diagnose and resistant to therapy. The existence
of piriformis syndrome has been doubted for years. In many instances it is not even
considered as a diagnosis, in others it is ruled out, and in others yet the symptoms
are ascribed to "sciatica" or some other cause, even if the piriformis is considered
as a possible cause. Often the patient has considered the possibility before the
physicians, trainers, therapists and others have.
"...The existence of piriformis syndrome has been doubted for years."
Piriformis syndrome may overlap with a variety of other problems including what McCrory
et. al. has called a "deep buttock" syndrome. This includes pain in the buttock region,
possibly pain in the hamstrings, occasionally pain in the back of the leg that is
difficult to locate.
These symptoms of the piriformis muscle dysfunction may be caused by other clinical
entities that include gluteus medius dysfunction, herniated or bulging disks, "sciatica"
and other musculoskeletal problems in this area. Scant information is available on the
piriformis syndrome in lay publications
The piriformis syndrome
------
Balanced Concepts
in Health
Piriformis Syndrome
by Christine M. Booras, B.A., LMT, CPFT
"What a pain in the _ _ _ _ !
No, I'm not talking about a fellow co-worker. What I am talking about is Piriformis
syndrome...
How can one muscle cause so much discomfort? Link The problem is its
relation to the sciatic nerve (shown below in yellow, running just under the
piriformis muscle), the largest nerve in the body. As the sciatic nerve runs from
the lower back and down the body to supply all of the nervous functions to the leg,
it just happens to pass underneath the piriformis muscle. Both the piriformis
muscle and sciatic nerve pass together through a small hole, or foramen, of the
pelvis.
If the piriformis muscle gets irritated due to excessive sitting, walking or
squatting it will be come inflamed and compress the sciatic nerve against the
bone. The result: radiating, excruciating pain. Because the gluteal muscles
are tight and contracted, "trigger points" and spasms may also develop due
to the lack of adequate blood and oxygen reaching the tissues. Now you have
a true "pain in the butt!"
Before the serious decision of a surgery you have the following options:
So, now what? There is hope and it doesn't have to involve surgery. Research
has proven that a combination of stretching, massage therapy, proper posture
and utilizing anti-inflammatory can produce a significant reduction or
elimination of pain.
Seeing as how it can possibly be a purely muscular condition, stretching should
be your first approach. Several stretches specifically designed to treat
piriformis conditions are described in a companion article. They should be
performed daily.
STRETCHING:
STRETCHES FOR THE PIRIFORMIS AND RELATED MUSCLES
It is always best to warm-up the muscles for about 3-4 minutes before stretching.
You can do this by jogging in place, jumping jacks, etc. Just to get the body
warmed up.
These stretches should be performed on both sides of the body one to two times
daily for treatment and then once each day after you have started getting some
relief.
Hold the stretch for 2-3 seconds and repeat a second time on the same side. Go
to other side and repeat what you did on the first side. Repeat whole sequence
3-5 times. Remember: NEVER BOUNCE!
We are stretching not only the piriformis but also other muscles that it affects
or is affected by. This will enhance the lengthening and softening of all
muscles involved.
MASSAGE THERAPY:
Massage Therapy can be very effective in re-nourishing the muscles with blood
and oxygen, thus helping to eliminate the spasms and "trigger points" that may
be present. On your own, you can do "self massage", use a tennis ball or
Lacrosse Ball for deeper penetration and have a partner help you out, which
can be fun.
You can also make an appointment with a Licensed Massage Therapist (LMT) who
knows how to treat "all the right spots" in order to expedite the healing process.
As always, follow the recommendations of your physician. In closing, utilizing
proper biomechanics, stretching, massage and anti-inflammatory can bring you
back to your normal self in no time, though you may have to deal with the other
"pains" at work with some other creative alternative!
Christine M. Booras, B.A., LMT, CPFT
================================================================================
Assess & Address
Piriformis Syndrome
by Whitney Lowe
Link
Radiating neurological pain that goes down the back of the leg is often diagnosed
as originating from disc hernias in the lumbar spine; however, there are numerous
sites where nerve irritation may produce similar symptoms. One of the most common
is in the gluteal region, where the sciatic nerve may get compressed by the
piriformis muscle, creating a condition known as piriformis syndrome.
Neurological pain may also be produced in this region by entrapment of other nerves,
such as the superior and inferior gluteal nerves. This entrapment is sometimes
referred to as piriformis syndrome, as well.
--------------------------------------------------------------------------------
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the course
of the sciatic nerve. This referred pain, called "sciatica", often goes down the
back of the thigh and/or into the lower back. Patients generally complain of pain
deep in the buttocks, which is made worse by sitting, climbing stairs, or performing
squats. The piriformis muscle assists in abducting and laterally rotating the thigh.
In other words, while balancing on the left foot, move the right leg directly sideways
away from the body and rotate the right leg so that the toes point towards the ceiling.
This is the action of the right piriformis muscle.
It is thought that acute or chronic injury causes swelling of the muscle and irritates
the sciatic nerve, resulting in sciatica. Patients with an aberrant course of the nerve
through the muscle are particularly predisposed to this condition.
The piriformis syndrome is diagnosed primarily on the basis of symptoms and on the
physical exam. There are no tests that accurately confirm the diagnosis, but X-rays,
MRI, and nerve conduction tests may be necessary to exclude other diseases. Some of the
other causes of sciatica include disease in the lumbar spine (e.g. disc herniation),
chronic hamstring tendonitis, and fibrous adhesions of other muscles around the sciatic
nerve.
Piriformis syndrome also causes sciatica. Its treatment is much less invasive and
severe than the treatment of herniated lumbar disks. However, many doctors never
consider piriformis syndrome as a possible diagnosis. Many physicians who are
aware of it are uncertain how to properly diagnose and treat it. A course of
daily stretching exercises is recommended (part of the protocol) to patients
to assist in recovery of the muscles and tendons.
Stretching can be combined with physical therapy modalities such as ultrasound.
If these fail, then injections of a corticosteroid into the piriformis muscle
may be tried. Finally, surgical exploration may be undertaken as a last resort.
The advent of MR Neurography and Open MR injection techniques together with new
large scale outcome studies are now leading to the successful diagnosis and treatment
of many more sciatica sufferers. Surgery is another resource for pain reduction
(although rarely used): it "cleans up" the fibrotic muscle scar tissue.
====================================================================================
This Publication Is Searchable
The Merck Manual of Diagnosis and Therapy
Section 5. Musculoskeletal And Connective Tissue Disorders Link
Chapter 62. Common Sports Injuries
Piriformis Syndrome
Sciatic pain can be caused by compression of the sciatic nerve by the piriformis
muscle. The piriformis muscle extends from the pelvic surface of the sacrum to the
upper border of the greater trochanter of the femur and, during running or sitting,
can squeeze the sciatic nerve at the site where the nerve emerges from under the
piriformis to over the gemellus and obturator internus muscles.
Symptoms and Signs
A chronic nagging ache, pain, tingling, or numbness starts in the buttocks but
can extend along the course of the sciatic nerve, down the entire back of the
femur and tibia, and in front of the tibia. Pain is usually chronic and worsens
when the piriformis is pressed against the sciatic nerve (eg, while sitting on
a toilet, a car seat, or a narrow bicycle seat or while running). Unlike piriformis
pain, disk compression of the sciatic nerve is usually associated with lumbar pain,
particularly during lumbar extension.
Diagnosis
Thorough physical examination is essential for diagnosis: Freiberg's maneuver
(forceful internal rotation of the extended thigh) stretches the piriformis muscle,
causing pain. Pace's maneuver (abducting the affected leg) elicits pain in a sitting
patient. For Beatty's maneuver, the patient lies on a table on the side of the
no affected leg. The affected leg is placed behind the non affected leg with the
bent knee on the table. Raising the knee several inches off the table causes pain
in the buttocks. For the Mirkin test, the patient should stand, keeping the knees
straight, and slowly bend toward the floor. The examiner should press into the
buttocks where the sciatic nerve crosses the piriformis muscle, causing pain that
starts at the point of contact and that extends down the back of the leg. Pain can
also occur with pelvic or rectal examination.
Treatment
The patient should stop running, bicycling, or performing any activity that elicits
pain. A patient whose pain is aggravated by sitting should stand up immediately or,
if unable to do so, change positions to raise the painful area from the seat.
Stretching exercises, although often recommended, are rarely beneficial, and any
movement that raises the knee forcibly often aggravates symptoms. A corticosteroid
injection into the site near where the piriformis muscle crosses the sciatic nerve
often helps, presumably by reducing fat around the muscle, making it less likely
to press on the nerve.
====================================================================================
Piriformis Stretch
The gentle Piriformis Stretch:
Place the right knee on the ground roughly in line with your
left shoulder The right foot should be just in front of the
left knee Press your hips towards the ground so that your
bodyweight is on your right leg. As you move down the right
knee comes closer to the left shoulder.
You should feel a gentle pull deep in the right hip / buttocks.
-----------------------------------------------------------------------------------
A good sports medicine physician with experience in caring for athletes with the
piriformis syndrome can help direct appropriate management. With proper diagnosis
and treatment, there is no reason for this syndrome to be dreaded. Good luck and
good training.
last update - 2/97
Diagnosis:
The symptoms most often reported are pain when running or walking in the gluteal
region. Pain may go down the back of the leg. Dyspareunia is sometimes noted.
Having the patient lie down, flex the knee to 10 - 20 degrees and then have the
patient attempt to externally rotate the leg against resistance. Pain may occur
with piriformis tendonitis. Direct tenderness will be found in the region of the
piriformis tendon over the buttock region.
If there is a positive test to the straight leg lift (causing sciatica like pain),
externally rotate the leg to see if this lessens the pain. This could indicate
compression of the sciatic nerve by the piriformis.
Be certain to examine the sacroiliac joint also.
Treatment:
Rest is usually recommended. A two to three week break from the sports and activities
that cause pain can be very helpful. Relative rest, meaning less intense workouts,
and fewer miles is also helpful, and should be used during your return to activity.
Like Achilles tendonitis and iliopsoas tendonitis this is a very difficult problem
to eliminate.
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the course
of the sciatic nerve. This referred pain, called "sciatica", often goes down the
back of the thigh and/or into the lower back. Patients generally complain of pain
deep in the buttocks, which is made worse by sitting, climbing stairs, or performing
squats.
The anatomical position of the muscle leads one to conclude that it functions in
some ways similar to that of the gluteus medius. The major portion of origin of the
piriformis is the anterior lateral portion of the sacrum and the insertion is on the
upper portion of the femur.
It can be seen that the sciatic nerve passes immediately below the piriformis muscle.
The first places the sciatic nerve inferior (below) to the Piriformis muscle and
superior (above) the gemellus muscle. Entrapment in this area is likely due to a
myospasm or contracture (tightening or shortening respectively) of either of these
two muscles. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
This particular syndrome can often mimic its more notorious counterpart known as
sciatica, and that being the case, it is often misdiagnosed as sciatica. The main
difference between sciatica and piriformis syndrome is in the cause. Sciatica is
directly due to a lumbar disc pressing on the sciatic nerve as it exits the intervertebral
foramen in the lumbar spine. What both of these complaints have in common is that
both can produce pain, numbness and tingling below the knee and into the foot.
Link to below article:
In the United States each year, 1.5 million people have lumbar MRI scans to look
for the cause of the buttock and leg pain called 'sciatica'. More than 1.2 million
of those scans fail to find the cause in the spine. Three hundred thousand of the
scans are sufficiently positive that the patient has lumbar spine surgery. Of the
300,000 surgeries, as many as 25% fail to relieve the pain - in many cases this
is because the diagnosis of a spinal cause for the sciatica was incorrect.
October 13, 2004
Piriformis Syndrome: The Big Mystery or A Pain In The Behind
by Stephen M. Pribut, DPM and
Amelia Perri-Pribut, B.S., R.N., M.B.A.
Piriformis syndrome is difficult to diagnose and resistant to therapy. The existence
of piriformis syndrome has been doubted for years. In many instances it is not even
considered as a diagnosis, in others it is ruled out, and in others yet the symptoms
are ascribed to "sciatica" or some other cause, even if the piriformis is considered
as a possible cause. Often the patient has considered the possibility before the
physicians, trainers, therapists and others have.
"...The existence of piriformis syndrome has been doubted for years."
Piriformis syndrome may overlap with a variety of other problems including what McCrory
et. al. has called a "deep buttock" syndrome. This includes pain in the buttock region,
possibly pain in the hamstrings, occasionally pain in the back of the leg that is
difficult to locate.
These symptoms of the piriformis muscle dysfunction may be caused by other clinical
entities that include gluteus medius dysfunction, herniated or bulging disks, "sciatica"
and other musculoskeletal problems in this area. Scant information is available on the
piriformis syndrome in lay publications
The piriformis syndrome
------
Balanced Concepts
in Health
Piriformis Syndrome
by Christine M. Booras, B.A., LMT, CPFT
"What a pain in the _ _ _ _ !
No, I'm not talking about a fellow co-worker. What I am talking about is Piriformis
syndrome...
How can one muscle cause so much discomfort? Link The problem is its
relation to the sciatic nerve (shown below in yellow, running just under the
piriformis muscle), the largest nerve in the body. As the sciatic nerve runs from
the lower back and down the body to supply all of the nervous functions to the leg,
it just happens to pass underneath the piriformis muscle. Both the piriformis
muscle and sciatic nerve pass together through a small hole, or foramen, of the
pelvis.
If the piriformis muscle gets irritated due to excessive sitting, walking or
squatting it will be come inflamed and compress the sciatic nerve against the
bone. The result: radiating, excruciating pain. Because the gluteal muscles
are tight and contracted, "trigger points" and spasms may also develop due
to the lack of adequate blood and oxygen reaching the tissues. Now you have
a true "pain in the butt!"
Before the serious decision of a surgery you have the following options:
So, now what? There is hope and it doesn't have to involve surgery. Research
has proven that a combination of stretching, massage therapy, proper posture
and utilizing anti-inflammatory can produce a significant reduction or
elimination of pain.
Seeing as how it can possibly be a purely muscular condition, stretching should
be your first approach. Several stretches specifically designed to treat
piriformis conditions are described in a companion article. They should be
performed daily.
STRETCHING:
STRETCHES FOR THE PIRIFORMIS AND RELATED MUSCLES
It is always best to warm-up the muscles for about 3-4 minutes before stretching.
You can do this by jogging in place, jumping jacks, etc. Just to get the body
warmed up.
These stretches should be performed on both sides of the body one to two times
daily for treatment and then once each day after you have started getting some
relief.
Hold the stretch for 2-3 seconds and repeat a second time on the same side. Go
to other side and repeat what you did on the first side. Repeat whole sequence
3-5 times. Remember: NEVER BOUNCE!
We are stretching not only the piriformis but also other muscles that it affects
or is affected by. This will enhance the lengthening and softening of all
muscles involved.
MASSAGE THERAPY:
Massage Therapy can be very effective in re-nourishing the muscles with blood
and oxygen, thus helping to eliminate the spasms and "trigger points" that may
be present. On your own, you can do "self massage", use a tennis ball or
Lacrosse Ball for deeper penetration and have a partner help you out, which
can be fun.
You can also make an appointment with a Licensed Massage Therapist (LMT) who
knows how to treat "all the right spots" in order to expedite the healing process.
As always, follow the recommendations of your physician. In closing, utilizing
proper biomechanics, stretching, massage and anti-inflammatory can bring you
back to your normal self in no time, though you may have to deal with the other
"pains" at work with some other creative alternative!
Christine M. Booras, B.A., LMT, CPFT
================================================================================
Assess & Address
Piriformis Syndrome
by Whitney Lowe
Link
Radiating neurological pain that goes down the back of the leg is often diagnosed
as originating from disc hernias in the lumbar spine; however, there are numerous
sites where nerve irritation may produce similar symptoms. One of the most common
is in the gluteal region, where the sciatic nerve may get compressed by the
piriformis muscle, creating a condition known as piriformis syndrome.
Neurological pain may also be produced in this region by entrapment of other nerves,
such as the superior and inferior gluteal nerves. This entrapment is sometimes
referred to as piriformis syndrome, as well.
--------------------------------------------------------------------------------
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the course
of the sciatic nerve. This referred pain, called "sciatica", often goes down the
back of the thigh and/or into the lower back. Patients generally complain of pain
deep in the buttocks, which is made worse by sitting, climbing stairs, or performing
squats. The piriformis muscle assists in abducting and laterally rotating the thigh.
In other words, while balancing on the left foot, move the right leg directly sideways
away from the body and rotate the right leg so that the toes point towards the ceiling.
This is the action of the right piriformis muscle.
It is thought that acute or chronic injury causes swelling of the muscle and irritates
the sciatic nerve, resulting in sciatica. Patients with an aberrant course of the nerve
through the muscle are particularly predisposed to this condition.
The piriformis syndrome is diagnosed primarily on the basis of symptoms and on the
physical exam. There are no tests that accurately confirm the diagnosis, but X-rays,
MRI, and nerve conduction tests may be necessary to exclude other diseases. Some of the
other causes of sciatica include disease in the lumbar spine (e.g. disc herniation),
chronic hamstring tendonitis, and fibrous adhesions of other muscles around the sciatic
nerve.
Piriformis syndrome also causes sciatica. Its treatment is much less invasive and
severe than the treatment of herniated lumbar disks. However, many doctors never
consider piriformis syndrome as a possible diagnosis. Many physicians who are
aware of it are uncertain how to properly diagnose and treat it. A course of
daily stretching exercises is recommended (part of the protocol) to patients
to assist in recovery of the muscles and tendons.
Stretching can be combined with physical therapy modalities such as ultrasound.
If these fail, then injections of a corticosteroid into the piriformis muscle
may be tried. Finally, surgical exploration may be undertaken as a last resort.
The advent of MR Neurography and Open MR injection techniques together with new
large scale outcome studies are now leading to the successful diagnosis and treatment
of many more sciatica sufferers. Surgery is another resource for pain reduction
(although rarely used): it "cleans up" the fibrotic muscle scar tissue.
====================================================================================
This Publication Is Searchable
The Merck Manual of Diagnosis and Therapy
Section 5. Musculoskeletal And Connective Tissue Disorders Link
Chapter 62. Common Sports Injuries
Piriformis Syndrome
Sciatic pain can be caused by compression of the sciatic nerve by the piriformis
muscle. The piriformis muscle extends from the pelvic surface of the sacrum to the
upper border of the greater trochanter of the femur and, during running or sitting,
can squeeze the sciatic nerve at the site where the nerve emerges from under the
piriformis to over the gemellus and obturator internus muscles.
Symptoms and Signs
A chronic nagging ache, pain, tingling, or numbness starts in the buttocks but
can extend along the course of the sciatic nerve, down the entire back of the
femur and tibia, and in front of the tibia. Pain is usually chronic and worsens
when the piriformis is pressed against the sciatic nerve (eg, while sitting on
a toilet, a car seat, or a narrow bicycle seat or while running). Unlike piriformis
pain, disk compression of the sciatic nerve is usually associated with lumbar pain,
particularly during lumbar extension.
Diagnosis
Thorough physical examination is essential for diagnosis: Freiberg's maneuver
(forceful internal rotation of the extended thigh) stretches the piriformis muscle,
causing pain. Pace's maneuver (abducting the affected leg) elicits pain in a sitting
patient. For Beatty's maneuver, the patient lies on a table on the side of the
no affected leg. The affected leg is placed behind the non affected leg with the
bent knee on the table. Raising the knee several inches off the table causes pain
in the buttocks. For the Mirkin test, the patient should stand, keeping the knees
straight, and slowly bend toward the floor. The examiner should press into the
buttocks where the sciatic nerve crosses the piriformis muscle, causing pain that
starts at the point of contact and that extends down the back of the leg. Pain can
also occur with pelvic or rectal examination.
Treatment
The patient should stop running, bicycling, or performing any activity that elicits
pain. A patient whose pain is aggravated by sitting should stand up immediately or,
if unable to do so, change positions to raise the painful area from the seat.
Stretching exercises, although often recommended, are rarely beneficial, and any
movement that raises the knee forcibly often aggravates symptoms. A corticosteroid
injection into the site near where the piriformis muscle crosses the sciatic nerve
often helps, presumably by reducing fat around the muscle, making it less likely
to press on the nerve.
====================================================================================
Medical Operative Report For Paul Dean
Sciatica, Piriformis Syndrome, Piriformis Release, Piriformis Surgery for
buttock injury occurring on April 4, 2001 from a fall injury at construction
site at job.
Doctors Report Provided Below.
TUSTIN HOSPITAL AND MEDICAL CENTER
14662 Newport Avenue, Tustin, California 92780
SURGEON: Israel P. Chambi, M.D.
ASSISTANT SURGEON: Edward Boseker, M.D.
DATE OF SERVICE: 06/09/04
DIAGNOSIS
1. Piriformis syndrome.
2. Residual sciatic nerve root irritation, status post lumbar
laminectomy/discectomy.
3. Lumber discogenic disease, L5-S1.
OPERATION:
1. Decompression of the right sciatic, posterior cutaneous, and inferior
gluteal nerves, and the operative microscope was used.
2. Mapping of the nerves in the gluteal area using electrical stimulation.
ESTIMATED BLOOD LOSS: 10 cc.
INDICATIONS: The patient is a 39-year-old, right-handed male who comes
with a history being involved in an industrial injury on 04/02/2001. The
patient presents with intense pain in the right buttocks with radiation to
the right leg. The patient also has experienced weakness in the hamstring
muscles with sensory deficit in the right S1 and L5 nerve root distribution.
The patient has a positive Tinel sign in the region of the right sciatic
notch as well as pain in the distribution of the piriformis muscle. The
patient had received extensive medical treatment. Initially, the patient
improved with piriformis injections. However, over last recent months, the
patient has substantial recurrence of the pain that clearly increases with
sitting and is relieved by rest. Pain medications have provided minimal
relief of the patient's pain. Based on the lack of improvement with
intensive medical treatment, the patient was recommended to have an operation
to decompress mainly the sciatic nerve as well as the inferior gluteal and
the posterior cutaneous nerve. The patient understands the risks of
operation including infection, bleeding, the possibly of nerve damage,
as well as the potential possibility that the operation may not improve,
and after the implications of operation, the patient signed the consent.
PROCEDURE IN DETAIL: After obtaining general endotracheal anesthesia, the
patient was placed in the prone position on a Wilson frame. The right buttock
was prepped and draped in the sterile fashion. A small curvilinear incision
was made. The incision was carried down through the subcutaneous tissue. The
gluteus maximus muscle was split parallel to its fibers. We took an oblique
approach to direct our view to the piriformis muscle. The gluteus maximus
was extremely taken; we have problems in applying the appropriate retraction.
Immediately, we were able to identify the inferior gluteal nerve, which was
substantially displaced medially and the inferior gluteal nerve was displaced
inferiorly. We came to find a very prominent fibrosis involving --
Page 1
OPERATIVE REPORT
Patient Name: PAUL DEAN
MR NO:
Physician: ISRAEL P. Chambi, M.D.
----------------------------------------------------------------------------------
Page 2
OPERATIVE REPORT
TUSTIN HOSPITAL AND MEDICAL CENTER
14662 Newport Avenue, Tustin, California 92780
-- almost the entire piriformis muscle and this was causing the substantial
displacement of the sciatic nerve as well as the posterior cutaneous and inferior
displacement of the inferior gluteal nerves. Using the microscope, a portion of
the muscle that is still attached to this fibrous tissue that looks like very
thick fibrous bands were cauterized with bipolar electrocoagulaton and then
sectioned with Metzenbaum scissors. Once this was sectioned, there was a
substantial decompression of the sciatic nerve and we were able to place a #3
Penfield into the pelvis through the sciatic notch. Further stimulation of the
inferior gluteal nerve demonstrated that the nerve was working well and this
was not affected during our dissection. The fatty tissue that was there
in the vessel was replaced to cover the sciatic nerve. Then fibrin glue
was applied. After obtaining excellent hemostatis, the fascia of the gluteus
maximus muscle was approximated with interrupted 2-0 Vicryl sutures as well as
the subcutaneous tissue and the skin with 5-0% to reduce the incision pain.
The patient tolerated the procedure well.
ESTIMATED BLOOD LOSS: 10 cc.
NEEDLE AND SPONGE COUNT: Correct.
FINDINGS: We found a very thick fibrosis involving most of the piriformis
muscle replacing and displacing the sciatic nerve medially. Following the
operation, there was substantial relaxation of the sciatic nerve. There were
no complications:
___________________________
ISRAEL P. Chambi, M.D.
IMC/MWSM
D: 06/09/2004 09:41
T: 06/09/2004 22:44
JOB: 161795
Page 2
OPERATIVE REPORT
Patient Name: PAUL DEAN
MR NO:
Physician: ISRAEL P. Chambi, M.D.
--------------------------------------------------------------------------------
DISABILITY STATUS
This patient will continue on temporary total disability. Good or bad,
to be declared permanent and stationary after sufficiently recovered.
DISCLOSURE STATMENT
I declare under penalty of perjury that I, the signing physician, have
actually performed this examination and the time spent in performing this
evaluation is in compliance with the IMC Guidelines
(Section 5307.1 and 4507.6).
I declare under perjury that I have devoted at least 1/3 of my total
practice to providing medical treatment.
ISRAEL P. Chambi, M.D.
----------------------------------------------------------------------------
 Stock Photo
Israel P. Chambi-Venero, MD
Neurosurgeons
Israel P. Chambi, M.D., FACS
801 N. Tustin Ave., Suite 406
Santa Ana, CA 92705
714 973 0810
FAX 714 973 0840
drisraelchambi@yahoo.com
Diplomat American Board of Neurological Surgery Brachial-Plexus & Peripheral
Nerve Institute
micro neural surgeon
- Santa Ana, California (CA) 92705
PRESCRIPTION
Stock Photo
Israel P. Chambi-Venero, MD
Neurosurgeons
Israel P. Chambi, M.D., FACS
801 N. Tustin Ave., Suite 406
Santa Ana, CA 92705
714 973 0810
FAX 714 973 0840
drisraelchambi@yahoo.com
Diplomat American Board of Neurological Surgery Brachial-Plexus & Peripheral
Nerve Institute
micro neural surgeon
- Santa Ana, California (CA) 92705
PRESCRIPTION
ISRAEL P. CHAMBI, M.D., FACS
Diplomat American Board of Neurological Surgery
Adult & Pediatric Neurosurgery
Brachial Plexus & Peripheral Nerve Surgery
Address:
XXX XXXXX
XXX XXXXX Santa ANA, CA 92705
Paul Dean 39
_______________________________________________
Name (Print) Age
XXXX Riverside, CA 6/29/2004
_______________________________________________
Address City Date
Rx
Hydrocodone/Apap 5/500 - Tab Every 4 hours
Mobic #15 - Once A Day
Post Piriformis Syndrome
Right - Center
Physical Therapy 3 times a week for 6 weeks
Ultrasound
Right Massage
Heat
No Weights
No Stretching
Thank you.
_______________________________________________
Israel P. Chambi, M.D. Calif. Lic. # XXXXXXXXXX
------------------------------------------------------------------------
My questions to Dr. Chambi at first post surgery visit. I already
had a back surgery (L5 S1 Discectomy) a year and a half earlier.
POST-OP RT. PIRIFORMIS RELEASE FIRST VISIT TO DR. CHAMBI AFTER SURGERY
WHY DO I STILL HAVE PAIN AFTER THE SURGERY...
June 29, 2004
QUESTIONS FOR DR. CHAMBI FROM PAUL DEAN, PATIENT:
1. Why do I still have intense pain when sitting, lifting,
standing long periods, or moving around after the Piriformis
Surgery?
DR CHAMBI: You are having pain because your sciatic nerve
in the Piriformis Region has shrunk and lost elasticity.
Over the next 6 months the body will bring some of that
elasticity back and then the nerve will be able take stretching
and lifting which take a longer length of elasticity than
you have at this time.
DR CHAMBI:
You have been scarred down completely by your Piriformis Muscle
and your nerve has been impinged for so long that it will take
some time for the sciatic nerve to heal.
2. What can I do in the meantime to help the healing, so that
I can get back to lifting and sitting and doing what I was
able to do in the past?
DR. CHAMBI: Do not stretch the sciatic nerve and do not lift
any weights. This damages the sciatic nerve. You can do light
walking and massage as well as ultra sound and heat can be
applied to the region affected region. Use Vicodin for pain,
and Mobic to help circulation and nerve healing.
3. What exactly was done in the surgery?
DR. CHAMBI: The Piriformis muscle was separated
and several inches of scarring that
was attached to the sciatic nerve was
removed.
4. Did you remove any of my Piriformis Muscle?
DR. CHAMBI: It was cut, but none was removed.
5. How much Piriformis Muscle did you cut through?
DR. CHAMBI: About two-thirds of the Piriformis
was cut through.
6. How much scarring did you remove?
DR. CHAMBI: Several inches of scar tissue was
removed because it had adhered to
the sciatic nerve making it impossible
for the nerve to move, giving you pain.
7. Will the scarring come back and a later time?
DR. CHAMBI: No it will not. We use a Fibrin Glue
which stops scar tissue.
8. Will my pain get better?
DR. CHAMBI: Some elasticity in the sciatic nerve
will come back, reducing your pain.
9. Will I be 100%?
DR. CHAMBI: You should get quite a bit better now
that your sciatic nerve is no longer
trapped. However, the nerve has been
entrapped for three years and has been
compressed extremely and will need to
heal. All sciatic nerve healing is slow
and we will have to wait and see what
the final outcome of healing will be.
You will be in physical therapy for quite
some time before we know how well you
have healed up.
10. Does waiting a long time before the surgery become a
problem for the healing of a sciatic nerve?, in my case
it has been three years since my injury first occurred.
DR. CHAMBI: Yes, when the sciatic nerve is compressed for a
very long time, it is less likely that it will regain its
elasticity and full functioning.
11. If I exercise my muscles or body will that help the healing
process of my sciatic nerve?
DR. CHAMBI: No. The sciatic nerve does not do well when stretched
or exercised a lot. Soft message and gentle walking and are recommended,
but do not stretch the sciatic nerve and do not lift weights as this
hurts the injured sciatic nerve. You do not have a muscle problem,
but a nerve problem which needs very gentle care. Stretching and
strengthening does not help a damaged nerve, and you do not want to
inflame the area.
12. I know that 8 out of 10 patients were helped by the Piriformis
Release and I am glad I did the operation because the intensity of
my pain has been reduced from it maximum pain levels, and I was
wondering why 2 patients had a failure of an outcome?
DR. CHAMBI: Both patients waited to long before having the piriformis
release surgery. The first patient waited 8 years and the second
patient waited 10 years, and they never regained elasticity of their
nerve and there was permanent damage because the sciatic nerve was
compressed for two long.
13. Have you treated any Professional Sports Figures lately, and
how is there recovery?
DR. CHAMBI: We just did a Piriformis Release on a Professional
Baseball player who hurt his sciatic nerve in the Piriformis Region
a year ago while pitching a fastball. We gave him the release and
he is still recovering at this time.
14. Why did I have to see four Doctors before you and none knew
that I had piriformis syndrome, but you figured it out right away.
These other doctors were well known in their Orthopedic field and
Neurological fields. It was quite upsetting that nobody could tell
me the real reason I was in pain. I feel like this is the most
misunderstood injury there could possibly be. It has the sciatic
pain that goes down to the foot and every doctor assumes that you
have a bad disc, or a failed back surgery. Why is there such a
misunderstanding about this injury?
DR. CHAMBI: Most Doctors never see this type of injury in their practice
because it is quite rare in most practices, however, I see this type
of injury quite often because I deal so much with professional
athletes. You have to fall in an unusual manner to get this type
of trauma. The fall must be sideways and backwards which occurs often
in football lineman and other high contact type of sports.
DR. CHAMBI:
The Doctor must rule out disk problems in the back by looking at the
MRI and determining that the disk in the back is not affecting the pain
after a back surgery because the nerve in the back is freed up from that
surgery. Also the symptoms are different for Piriformis Syndrome than
in the back patient. There is buttock pain in the Piriformis region
that is quite specific and the piriformis muscle is in spasm in many
cases. The pain is mostly in the outlaying areas and not in the
lower back region specifically. Lidocaine Injections usually help
calm down the Piriformis Muscle which helps the pain go away and this
is a positive sign that you have Piriformis Syndrome. However, if
your sciatic nerve has been scarred down, that scarring needs to
be removed so that you can have full range of motion without pain.
The sciatic nerve needs to have full elasticity and movement and cannot
be compressed by the spasm or displaced Piriformis Muscle.
15. I still cannot sit, lift or stretch or be active without a lot
of pain. Do you think this will all change for the better?
DR. CHAMBI: Yes, but it will take some time for the sciatic nerve to heal,
and it cannot be rushed. You will be doing a lot better in time but
you need to take it easy for right now.
Thank you Dr. Chambi, I will be going into physical therapy three times
a week for six weeks and am looking forward to my next visit with you.
I am glad I did the surgery and feel I now have an opportunity to heal,
and I was not able to heal before now because my nerve was way to impacted
and scarred down in the past to heal on my own. At least now I have a
chance to get better. It is a shame that no other Doctor could diagnose
this problem, and that I had to wait so long. Every day my nerve
is impacted the chances of full recovery are that much worse as permanent
damage can be caused.
Click below for the photos of the operation for the following:
Piriformis Release Surgery
Dr. Israel Chambi, Neurosurgeon: Training and Civil life:
Dr. Israel Chambi finished his undergraduate training at the National University
of Arequipa, Peru, and his medical training at the University of Mexico in 1974.
He came to California for his internship at the University of California at both
the Irvine and Los Angeles campuses, and later moved to Toronto, Canada, where
he obtained a fellowship in stereotactic neurosurgery. He held a teaching and
research post at the University of California at Irvine and founded the Brachial
Plexus and Peripheral Nerve Institute in Santa Ana. At the present time he is chair
of the division of neurosurgery at Western Medical Center in Santa Ana.
Besides his contribution to the scientific world, Dr. Israel Chambi is an exemplary
contributor to civic and church life. He excels in the field of neurosurgery, not
only in his clinical skills, but also as a teacher, mentor, publisher, and national
and international speaker. He has been a supporter of La Sierra University's Stahl
Center for World Service. His ethnic roots motivated him to participate in various
projects, which bring north and south together. His cross-cultural vision motivated
him to pioneer "Radio Adventista" in the Peruvian Andes and to promote medical
conferences in Arequipa, Peru.
The Chambi Venero brothers are part of the history of rural education in Peru.
Evenezer Chambi owns a clinic in Beverly Hills, California and his brother
Dr. Israel Chambi is a renowned neurologist who also lives in the United States
of America.
Chambi Father and head of Family:
The head of the family is Pastor Pedro Chambi, learned to read at age 22.
As a leader in his local congregation, Dr. Chambi has a lasting impact in fostering
inclusiveness and interdependence in the multi-ethnic Santa Ana Seventh-day Adventist
Church. He is married to Rosalba Chambi, who is a nurse, and has three children:
Ruth, Moses, and Israel Jr.
NEWS: La Sierra University
Donors: Dr. Israel and Mrs. Rosalba Chambi - half million-dollar gift for the Science
Complex at Los Sierra University, 4700 PIERCE ST , RIVERSIDE , CA - 92515
Dr. Israel Chambi, Neuro-Surgeon
Wife: Rosalba Chambi - Nurse
Dr. Israel Chambi is a neurosurgeon in Orange County. He and his wife, Rosalba Chambi
are exemplary contributors to civic and church life. Born and raised in Peru and Mexico,
the Chambi's international roots and cross-cultural vision motivate participation in
projects that foster inclusiveness in both North and South America such as the founding
of Radio Adventist in the Peruvian Andes and this their most recent gift to La Sierra
University for the new Science Complex.
Professional Reports:
Chambi, Israel P. "The Piriformis Syndrome Manifesting As Lumbar Disc Syndrome: Report
of 19 Cases" The Western Neurosurgical Society, Annual Meeting, Boson, MA., August 18, 1994
Chambi, Israel P. "The Piriformis Syndrome Manifesting As Lumbar Disc Syndrome: Report
of 19 Cases" The Western Neurosurgical Society, Annual Meeting, Gleneden Beach, Oregon.
September 9-12, 1995.
Neuroscience Conference
02.20.92 Annual Scientific Program
UCI Neurosurgery and SNSOC
"Does Piriformis Syndrome Exist?"
State-Of-The-Art Microscope Provides Incredible Precision In
Neurosurgery
"The diameter of a human hair, is how Israel P. Chambi, M.D., FACS, a Diplomat of the
American Board of Neurological Surgery and a distinguished Fellow of the American College
of Surgeons, describes the size of a blood vessel in the brain. "A small peripheral nerve
is no larger than a toothpick." This obstacle of scale, present in even the simplest surgeries,
is the reason the sue of a high-powered microscope is an essential part of his neurosurgical
practice at Tustin Medical Center.
Most people understand that high blood pressure can disrupt blood flow to the brain,
causing a stroke. Dr. Chambi explains that, like the brain, the peripheral nervous
system is also vulnerable to pressure. "Many of my patients are athletes who experience
pain from pressure on the peripheral nerves in their arms or legs. The pressure may
be caused by an actual injury or be secondary to inflammation of the nerves caused by
overuse." Dr. Chambi's goal is to correct or minimize the neurological disability
that results from disruption in blood flow caused by pressure from swelling or
bleeding within the nervous system.
Unique in the diversity of his practice, Dr. Chambi is noted for his expertise in
neurovascular surgery. Also, he is one of only a handful of surgeons in the region who
perform specialized surgery to treat disorders of the peripheral nerves, including
nerve gafting procedures. In addition to maintaining his private practice, Dr. Chambi
has been instrumental in the development of the Neurovascular and Peripheral Nerve
service at Western Medical Center, where he is part of a team of qualified neurosurgeons.
NOTE: He is not at Western Medical Center but is instead at Tustin Medical Center at this
time.
Additional information regarding the use of microsurgery for the treatment of
neurovascular or peripheral nerve disorders, such as those listed below, may be
obtained by requesting a referral from your physician or by contacting Dr.
Chambi's staff at 714-973-0810.
* Aneurysm and Arteriovenous Malformation
* Spinal Disorders -- Ruptured Disc, Stenosis
* Traumatic Brain and Spinal Cord Injuries
* Brain Tumors *hydrocephalus
* Breathing Disorders -- Phrenic Nerve Pacemaker
* Peripheral Nerve Disorder Affecting the Arms and Legs
CURRICULUM VITAE
Isreal P. Chambi, M.D.
PERSONAL DATA:
Date of Birth: January 25, 1949 - Chile
Home Address: 112 South M***** ********** ***
Anaheim, CA.
Business Data: Brachial Plexus and Peripheral Nerve Institute
801 N. Tustin Ave Suite 406
Santa Ana, CA 92705
(714)-973-0810
FAX: (714)-973-0840
Citizenship: United States
EDUCATION
1966-68 National University of Peru B.S.
Arequipa, Peru
1968-74 University of Mexico M.D.
Mexico City, Mexico
POSTGRATUATE TRAINING
1978-79 Martin Luther King Internship
Medical Center
Los Angeles, California
1979-81 University of California, Irvine General Surgery
Medical Center Resident
Orange, California
1981-83 University of California, Irvine Neurosurgery
Medical Center Resident
Orange, California
-------------------------------------------------------------------------------
As a side note... Compassion is in the family.
Israel P. Chambi, M.D. has a brother, Ebenezer Chambi, M.D. Link
Ebenezer Chambi, M.D.
 Family practice Physician
Chapel Medical Clinic
9739 California Avenue
South Gate, CA 90280
Phone: 323-567-1212
-------------------------------------------------------------------------------
Ebenezer Chambi: Dialogue with an Adventist physician, health educator, and
community leader Link
Ebenezer Chambi MD - Chambi Ebenezer MD
9739 California Ave
South Gate, CA 90280
Phones: (323) 564-2228
by Michael Peabody
Born in Peru, Dr. Ebenezer Chambi developed early in his life a sense of community
and an inclination to service. His family was active in the local church. Throughout
his educational experience, he was guided by a commitment to help others. In 1970,
he completed his pre-medical studies at Union College (now Peru Union University)
located near Lima, the capital. Although he wanted to study medicine in his homeland,
the then prevailing political situation made this virtually impossible. His older
brothers had moved to Mexico to pursue their medical training; so did he.
Completing his medical degree from the Autonomous University of Guadalajara, Mexico,
in 1975, he did his residencies in Puerto Rico and Los Angeles, California. After
completing the latter, Dr. Ebenezer Chambi joined a research team to study epilepsy.
Currently, he is practicing general medicine at the Chapel Medical Clinic in South
Gate, California. In addition to ensuring quality care to his patients, Dr. Ebenezer
Chambi brings his Christian commitment to bear on his profession by continually
promoting preventive care and healthful living. He is involved in his community through
a variety of activities ranging from sponsoring folk music concerts to speaking to
high school students on health. In recognition of his community service, he received
in 1994 the La Sierra University Presidential Citation for Humanitarian Service.
Ebenezer Chambi and his wife, Esther, have three children who are pursuing advanced
studies: Esther Janet, Ebenezer Howard, and Eber Caleb.
Dr. Ebenezer Chambi, what influences have shaped your life?
Perhaps the same four major influences that shape all of us: family, education,
community, and religion. The family teaches us how to care for each other. Parents
care for children, children care for each other and their parents. In a good home,
we learn to love people unconditionally. Education is one of the major ways to learn
about ourselves and develop our talents and intellectual skills. It structures our
personality. Community teaches us that we are not alone-no one is an island. We
depend on other people and they depend on us. Christianity gives us inner strength,
especially when we feel discouraged and don't have energy to keep going. There is a
higher power, God, ready to help us. Religion gives us the powerful tool of confidence.
It brings us strength and hope. It keeps us from giving up on life. At the end of
the journey, it gives us the assurance of a better life.
What type of research did you do in epilepsy?
Epilepsy can be a very debilitating disease, and our team wanted to find its cause
and determine whether it could be successfully treated or even cured. We studied a
diverse population in the Los Angeles area, seeking ways of helping epilepsy victims.
The results were rewarding. Some were cured. Many were able to live relatively normal
lives and return to their vocations.
Currently, what does your practice cover?
I am involved in general practice. Beyond the regular treatment of patients, I focus
on preventive medicine. I want to teach people how to live healthier, happier lives.
In my practice, I see a lot of baby boomers. I'm one of them, so I know what they are
like and how they live. Because they work so many hours and have so many activities,
they often wait until the last possible moment to come to see me, knowing that a visit
to the doctor takes time. They usually don't come in when they have a slight cold or
a stomach ache. They visit my office only when they sense that they are in serious
trouble and need help. We do a complete check-up, including blood and urine tests.
Most of the time we find that they have high cholesterol levels; they are not eating
right and not exercising. Most of the common problems can be prevented, and I emphasize
that.
How do you convince busy people to live healthier lives?
The key is behavior modification. We can give objective explanations of why a person
should exercise more or spend some time relaxing rather than overworking, but it is
challenging to convince people that they need to make fundamental changes in how they
live. At times a physician needs to be quite direct, even blunt, to persuade patients
to radically alter their lifestyle.
A while back, a man, suffering from exhaustion, came to my office. He was working at
two jobs so he could buy a new house every year. His wife told me that he worked too
many hours a day and did not take time to relax and enjoy life. She told me that they
already owned three homes and that he wanted to buy another one. I told her, "Don't
worry. The more he works, the more houses he will leave to you when he dies!" He got
the message and changed his habits.
Do you also utilize the media to educate the public?
When I was doing my residence in Puerto Rico, I started a radio program on health
prevention and promotion. Then here, in the Los Angeles area, I hosted for ten years
a weekly radio forum called El Médico Habla (The Physician Speaks) that was quite
popular. We have also prepared several short video programs on health that I make
available to pastors and TV cable stations.
Does the emphasis on exercise and nutrition in the popular media help in having
people change their lifestyle?
Yes. Ten or 15 years ago, it was more difficult to convince people that they needed
to exercise and eat well. But now, the media's coverage of prevention and health has
made my job easier in terms of education. The problem is that many people who understand
the principles of healthful living aren't putting them into practice. They still eat
too much fast food and stay up too late watching the late shows.
Fortunately, people are beginning to see the light. The city where I practice has a
park where you can see more people running, walking, and doing other exercises than
in any other park in the nearby cities. I like to think this has something to do with
our emphasis on exercise.
The hamburger place that is near our office now also sells vegetarian burgers. I think
that shows some of the positive influence we've had on people who are trying to eat
more healthful foods.
How can people who are not involved in the health-care profession effectively spread
the message of healthful living?
All of us exert an influence and convey a silent message wherever we go. People are
searching for a better life, and they look up to good role models. If we spend time
with people, we can influence them positively by your example. I've found it effective
not to preach at people, but rather to lead by example. We can encourage others to see
that there's a better life.
It's easy to become so focused on our own studies or profession that we forget that
we are part of a larger community outside our walls. How can a person who has become
so insulated begin to interact with the larger community beyond their family or church?
Before I became active in the community, it was easy to be critical of those outside
my circle. But after I became involved, I discovered how much good I could do and how
much I enjoyed it.
Get to know other people, especially those with whom we would not normally associate.
It will help with your social and intellectual development. You will also learn how
your community works and how you can help.
Becoming involved begins with something as simple as the way you greet people. Start
with a solid and sincere, "Good morning. How are you?" Speak words of encouragement.
Learn to listen. Meet with the people who are having problems in your area of expertise
who don't know where to look for help. Focus on relieving their suffering.
A few years ago, an earthquake hit the Los Angeles area. When people asked me why I
left my office to volunteer in the relief efforts, I told them that I was just paying
part of my debt to my community. The community has given me a lot and I want to give
back. It's a two-way street.
And don't forget to have fun! One of the things I do is organize folk-music concerts.
And though lots of people enjoy them, I enjoy them the most!
How do you apply this involvement in your church?
I love my church like a family. I do things not to be recognized or rewarded, but
because I want to do something for Christ and my church. If you start a project with
the goal of being recognized for your efforts, you miss the point. Instead, do the
job because it is important and necessary.
As a successful physician, a health educator, and community leader, what would your
counsel be to people who are just entering their careers?
Learn from successful people by watching how they live, how they get along with
others, and how they maintain their emotional balance. Emulate their good traits.
If I retrace my journey, being active in the church and in the community were the
most important factors that kept me on track. Those of us who have been blessed by
talents and education can do much good. Put yourself where God can use your skills.
Take the initiative to help the community and make people's lives better. That is
a worthwhile goal in life.
Interview by Michael Peabody. Michael Peabody is a third year law student at Pepperdine
University in Malibu, California. E-mail: mdpeabod@pepperdine.edu
Dr. Ebenezer Chambi's address: 9739 California Ave.; South Gate, California 90280; U.S.A.
-------------------------------------------------------------------------------
Orthopedics Link
Information about diagnosis and treatment of piriformis syndrome
What is piriformis syndrome?
Good question! No one really knows exactly what causes piriformis syndrome, or
if it really exists. Some physicians believe that piriformis syndrome is the
name given to hip/buttock pain that cannot be otherwise diagnosed. Others believe
that piriformis syndrome is a very real cause of pain and disability.
What is the piriformis muscle?
The piriformis is a muscle that travels behind the hip joint. The piriformis
muscle is small compared to other muscles around the hip and thigh, and it
aids in external rotation (turning out) of the hip joint. The piriformis muscle
and its tendon have an intimate relationship to the sciatic nerve--the largest
nerve in the body--which supplies the lower extremities with motor and sensory
function. The piriformis tendon and sciatic nerve cross each other behind the
hip joint, in the deep buttock. Both structures are about one centimeter in
diameter.
What do people think happens in piriformis syndrome?
It is thought that the piriformis muscle tendon may be tethering the sciatic
nerve, and causing an irritation to the nerve. While it has not be proven,
the theory supported by some physicians is that when the piriformis muscle
and its tendon are too tight, the sciatic nerve is choked. This may decrease
the blood flow to the nerve and irritate the nerve because of pressure.
What else may be causing this pain?
Sometimes referred to as "deep buttock pain," other causes of this type of
pain include spine problems (including herniated discs, spinal stenosis, etc.),
sciatica, and tendonitis. The diagnosis of piriformis syndrome is often given
when all of these diagnoses are eliminated as possible causes of pain. Other
signs of piriformis syndrome include examination maneuvers that attempt to
isolate the function of this muscle, and the finding of pain directly over
the tendon of the piriformis muscle.
Is there any treatment for piriformis syndrome?
Unfortunately, the treatment of piriformis syndrome is quite general, and
often this is a difficult problem to recover from. Some treatment suggestions are:
1. Physical Therapy - Emphasis on stretching and strengthening the hip rotator
muscles
2. Rest - Avoid the activities that cause symptoms for at least a few weeks
3. Anti-Inflammatory Medication - To decrease inflammation around the tendon
4. Deep Massage - Advocated by some physicians
5. On some occasions, when these treatments fail, patients have surgery to
release, or loosen, the piriformis muscle tendon. This surgery is not a
small procedure, and generally considered the last resort if a lengthy
period of conservative treatment does not solve the problem.
=============================================================================
eMedicine Specialties > Physical Medicine and Rehabilitation > Lower Limb Musculoskeletal
Conditions Link
Piriformis Syndrome
Last Updated: June 14, 2004 Rate this Article
Email to a Colleague
Synonyms and related keywords: hip socket neuropathy, pseudosciatica, wallet sciatica,
deep gluteal syndrome, piriformis syndrome
AUTHOR INFORMATION Section 1 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Author: Milton J Klein, DO, Consulting Staff, Department of Physical Medicine and
Rehabilitation, Sewickley Valley Hospital and Ohio Valley General Hospital
Milton J Klein, DO, is a member of the following medical societies: American Academy
of Disability Evaluating Physicians, American Academy of Osteopathy, American Academy
of Physical Medicine and Rehabilitation, American Association of Electrodiagnostic
Medicine, American Medical Association, American Osteopathic Association, and American
Osteopathic College of Physical Medicine and Rehabilitation
Editor(s): Rajesh R Yadav, MD, Assistant Professor, Section of Physical Medicine
and Rehabilitation, MD Anderson Cancer Center, University of Texas at Houston;
Francisco Talavera, PharmD, PhD, Senior Pharmacy Editor, Pharmacy, eMedicine;
Michael T Andary, MD, MS, Residency Program Director, Associate Professor,
Department of Physical Medicine and Rehabilitation, Michigan State University
College of Osteopathic Medicine; Kelly L Allen, MD, Consulting Staff, Department
of Physical Medicine and Rehabilitation, Lourdes Regional Rehabilitation Center,
Our Lady of Lourdes Medical Center; and Consuelo T Lorenzo, MD, Consulting Staff,
Department of Physical Medicine and Rehabilitation, Alegent Health Care, Immanuel
Rehabilitation Center
INTRODUCTION Section 2 of 10
Author Information Introduction Clinical Differentials Workup Treatment
Follow-up Miscellaneous Pictures Bibliography
Background: Piriformis syndrome has remained a controversial diagnosis since
its initial description in 1928. Piriformis syndrome usually is caused by neuritis
of the proximal sciatic nerve. The piriformis muscle can either irritate or compress
the proximal sciatic nerve due to spasm and/or contracture, and this problem can
mimic discogenic sciatica (pseudosciatica).
Pathophysiology: The piriformis muscle is flat, pyramid-shaped, and oblique.
This muscle originates to the anterior of the S2-S4 vertebrae, the sacrotuberous
ligament, and the upper margin of the greater sciatic foramen (see Image 1).
This muscle passes through the greater sciatic notch and inserts on the superior
surface of the greater trochanter of the femur. With the hip extended, the piriformis
muscle is the primary external rotator; however, with the hip flexed, the piriformis
muscle itself becomes a hip abductor. This muscle is innervated by branches from
L5, S1, and S2. A lower lumbar radiculopathy also may cause secondary irritation
of the piriformis muscle, which may complicate the diagnosis and hinder patient
progress.
Many developmental variations of the relationship between the sciatic nerve in
the pelvis and piriformis muscle have been observed. In approximately 20% of the
population, the muscle belly is split with one or more parts of the sciatica
nerve dividing the muscle belly itself. In 10% of the population, the tibial/peroneal
divisions are not enclosed in a common sheath. Usually, the peroneal portion splits the
piriformis muscle belly; the tibial division rarely splits the muscle belly.
Involvement of the superior gluteal nerve usually is not seen in cases of piriformis
syndrome. This nerve leaves the sciatic nerve trunk and passes through the canal
above the piriformis muscle.
Blunt injury may cause hematoma formation and subsequent scarring between the sciatic
nerve and short external rotators. Nerve injury can occur with prolonged pressure on
the nerve or vasa nervorum.
Etiology can be subdivided into a few categories as follows:
Hyperlordosis
Muscle anomalies with hypertrophy
Fibrosis (due to trauma)
Partial or total nerve anatomical abnormalities
Other causes can include the following:
Pseudo aneurysms of the inferior gluteal artery adjacent to the piriformis syndrome
Bilateral piriformis syndrome due to prolonged sitting during an extended
neurosurgical procedure
Cerebral palsy
Total hip arthroplasty
Myositis ossificans
Vigorous physical activity
This syndrome remains controversial because, in most cases, the diagnosis is clinical,
and no confirmatory tests exist to support the clinical findings.
Frequency:
In the US: Given the lack of agreement on exactly how to diagnose this condition,
estimates of frequency of sciatica caused by piriformis syndrome vary from rare to
approximately 6% of sciatica cases seen in a general family practice.
Approximately 90% of adults have had at least one episode of disabling LBP in their
lifetime.
Mortality/Morbidity: Piriformis syndrome is not life-threatening, but it can have
significant associated morbidity. The total cost of low back pain (LBP) and sciatica is
significant, exceeding $16 billion in both direct and indirect costs.
Sex: Some reports suggest a 6:1 female-to-male predominance. CLINICAL Section
3 of 10 Author Information Introduction Clinical Differentials Workup Treatment
Follow-up Miscellaneous Pictures Bibliography
History: Piriformis syndrome often is not recognized as a cause of LBP and associated
sciatica. This clinical syndrome is due to a compression of the sciatic nerve by the
piriformis muscle. This condition is identical in clinical presentation to LBP with
associated L5, S1 radiculopathy due to discogenic and/or lower lumbar facet arthropathy
with foraminal narrowing. Not uncommonly, patients demonstrate both of these clinical
entities simultaneously. This diagnostic dilemma highlights the need for patients with
LBP and associated radicular pain to undergo a complete history and physical examination,
including a digital rectal examination.
Many cases of refractory trochanteric bursitis are observed to have an underlying occult
piriformis syndrome due to the insertion of the piriformis muscle on the greater
trochanter of the hip. If both the trochanteric bursitis and the piriformis syndrome
are treated inadequately, both conditions remain resistant to medical management.
Physical: Examination findings may include the following:
Piriformis muscle spasm often is detected by careful deep palpation.
Digital rectal examination may reveal tenderness on lateral pelvic wall that
reproduces symptoms.
Reproduction of sciatica type pain with weakness is noted by resisted abduction/external
rotation (Pace test).
The Freiberg test is another diagnostic sign that elicits pain upon forced internal
rotation of the extended thigh.
The Beatty maneuver reproduces buttock pain by selectively contracting the piriformis
muscle. The patient lies on the uninvolved side and abducts the involved thigh upward;
this activates the ipsilateral piriformis muscle, which is both a hip external rotator
and abductor with the hip flexed.
A painful point may be present at the lateral margin of the sacrum.
Shortening of the involved lower extremity may be seen.
The patient may have difficulty sitting due to an intolerance of weight bearing on
the buttock.
The patient may have the tendency to demonstrate a splayed foot on the involved side
when in the supine position.
Piriformis syndrome alone is rarely a cause of a focal neuromuscular impairment; either
a sciatic mononeuropathy or an L5-S1 radiculopathy can mimic both of these conditions,
obscuring diagnosis of piriformis syndrome.
A Morton foot may predispose the patient to developing piriformis syndrome. The
prominent second metatarsal head destabilizes the foot during the push-off phase
of the gait cycle, causing foot pronation and internal rotation of the lower limb.
The piriformis muscle (external hip rotator) reactively contracts repetitively during
each push-off phase of the gait cycle as a compensatory mechanism, leading to piriformis
syndrome.
Causes: Approximately 50% of patients with piriformis syndrome have a history of trauma,
with either a direct buttock contusion or hip/lower back torsional injury. The remaining
50% of cases are of spontaneous onset, so the treating physician must have a high index of
suspicion for this problem, lest it be overlooked.
DIFFERENTIALS Section 4 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Lumbar Degenerative Disc Disease
Lumbar Facet Arthropathy
Lumbar Spondylolysis and Spondylolisthesis
Myofascial Pain
Trochanteric Bursitis
Other Problems to be Considered:
Lumbosacral radiculopathy
Buttock pain
Ischial tuberosity bursitis
Sciatica
Check the Internet for Related Articles:
Lumbar Degenerative Disc Disease
Lumbar Facet Arthropathy
Lumbar Spondylolysis and Spondylolisthesis
Myofascial Pain
Trochanteric Bursitis
Continuing Education
CME available for this topic. Click here to take this CME.
WORKUP Section 5 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Lab Studies:
Laboratory studies generally are not indicated in diagnosing piriformis syndrome.
Imaging Studies:
Diagnostic imaging of the lumbar spine is mandatory to exclude associated discogenic
and/or osteoarthritic contributing pathology.
Reports in the literature on piriformis muscle describe imaging by nuclear
diagnostic studies and MRI of the pelvis, but these tests are neither practical
nor reliable diagnostic approaches to this problem. The history and clinical
diagnostic examination provide the greatest and most specific diagnostic yield
for this problem.
Other Tests:
Results of electrodiagnostic testing for piriformis syndrome usually are normal.
Reports of positional H-reflex abnormalities can be found in the literature;
however, such findings have not been widely accepted or reproduced.
TREATMENT Section 6 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Rehabilitation Program:
Physical Therapy: Because a definitive method to accurately diagnose this problem
is not available, treatment regimens are controversial and have not been subjected
to randomized blind clinical trials. Despite this fact, numerous treatment strategies
exist for patients with piriformis syndrome.
Functional biomechanical deficits may include the following:
Tight piriformis muscle
Tight hip external rotators and adductors
Hip abductor weakness
Lower lumbar spine dysfunction
Sacroiliac joint hypomobility
Functional adaptations to these deficits include the following:
Ambulation with thigh in external rotation
Functional limb length shortening
Shortened stride length
Once the diagnosis has been made, these underlying perpetuating biomechanical factors
must be corrected.
Consider the use of ultrasound and other heat modalities prior to physical therapy
sessions. Prior to performing piriformis stretches, the hip joint capsule should be
mobilized anteriorly and posteriorly to allow for more effective stretching. Soft
tissue therapies of the piriformis muscle can be helpful, including longitudinal
gliding with passive internal hip rotation, as well as transverse gliding and sustained
longitudinal release with the patient lying on his/her side. Addressing sacroiliac
joint and low back dysfunction also is important.
A home stretching program should be provided to the patient. These stretches are an
essential component of the treatment program. During the acute phase of treatment,
stretching every 2-3 hours (while awake) is a key to the success of non operative
treatment. Prolonged stretching of the piriformis muscle is accomplished in either
a supine or orthostatic position with the involved hip flexed and passively adducted/
internally rotated.
Medical Issues/Complications: No consensus exists on overall treatment of piriformis
syndrome due to lack of objective clinical trials. Conservative treatment (eg,
stretching, manual techniques, injections, activity modifications, modalities like
heat or ultrasound, natural healing) is successful in most cases.
Injection therapy can be incorporated if the situation is refractory to the
aforementioned treatment program. For effective injection, the piriformis muscle
must be localized manually by digital rectal examination. Then the piriformis muscle
is injected using a 3.5-inch (8.9-cm) spinal needle. Care must be taken to avoid
direct injection of the sciatic nerve.
Surgical Intervention: Surgical management is the treatment of last resort. Surgery
for this condition involves resection of the muscle itself or the muscle tendon
near its insertion at the superior aspect of the greater trochanter of the femur
(as described by Mizuguchi). These surgical procedures are described as effective,
and they do not cause any associated superimposed postoperative disability.
Consultations:
Because of the enigmatic nature of piriformis syndrome, initial consultation obtained
from an orthopedic surgeon or similar specialist usually is nonspecific. This disorder
is considered to be a soft tissue problem that presents as low back or buttock pain
with sciatica. After all differential diagnoses have been excluded, consider piriformis
syndrome. Due to the traumatic etiology of most cases, piriformis syndrome usually is
associated with other more proximal causes of LBP, sciatica, and buttock pain (thereby
further clouding the diagnosis).
Other Treatment (injection, manipulation, etc.):
The Spray N' Stretch myofascial treatment and ultrasound modality preceding physical
therapy sessions are useful.
Manual muscle medicine, including facilitated positional release, may be helpful.
Injections with steroids, local anesthetics, and botulinum toxin have been reported
in the literature for this condition. No single technique is universally accepted.
Localization techniques include manual localization of muscle with fluoroscopic and
electromyographic guidance. The piriformis muscle, after localization with a digital
rectal examination, can be injected with a 3.5-inch (8.9-cm) spinal needle. Care should
be taken to avoid direct injection of the sciatic nerve.
FOLLOW-UP Section 7 of 10
Author Information Introduction Clinical Differentials Workup Treatment
Follow-up Miscellaneous
Further Inpatient Care:
Inpatient care would be necessary only if surgical intervention is warranted.
Surgery is the last resort treatment for severe cases of piriformis syndrome.
Further Outpatient Care:
Piriformis syndrome usually is treated effectively with conservative measures.
Please refer to the Treatment section for a discussion of treatment recommendations.
Deterrence/Prevention:
No method has been demonstrated to prevent piriformis syndrome. The best prevention
is to maintain biomechanical balance by restoration of a more physiologic weight
bearing distribution with a level pelvis/sacral base and equal leg lengths, achieved
by heel lift therapy if necessary. This treatment approach also prevents recurrences
of piriformis syndrome, especially if the underlying etiology is a leg-length discrepancy.
The patient also must engage in a general stretching program that includes bilateral
piriformis muscles.
Complications:
The most significant complication is failure to recognize, diagnose, and treat this
disabling condition. If left untreated, a patient may undergo unsuccessful back
surgery for a disc herniation; however, a coexisting occult piriformis syndrome
can result in a failed back syndrome.
Another complication is inadvertent direct injection of the sciatic nerve, which
usually results in a non disabling and temporary sciatic mononeuropathy.
Prognosis:
The prognosis depends upon early recognition and treatment. As this is a soft
tissue syndrome, it has a tendency to be chronic, usually due to late diagnosis
and treatment and has a less favorable prognosis.
Patient Education:
For conservative measures to be effective, the patient must be educated with an
aggressive home-based stretching program to maintain piriformis muscle flexibility.
He or she must comply with the program even beyond the point of discontinuation of
formal medical treatment.
MISCELLANEOUS Section 8 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Medical/Legal Pitfalls:
The greatest medical/legal concern is either misdiagnosis or failure to diagnose
piriformis syndrome. In most cases, the diagnosis is one of exclusion. Therefore,
if piriformis syndrome is not in the differential diagnosis list, it may be overlooked.
The patient becomes a chronic pain patient doomed to a lifetime of disability and
chronic management with medication. Because the diagnosis usually is elusive, missing
the diagnosis does not constitute malicious negligence and, therefore, rarely would
be sufficient grounds alone for a medical malpractice lawsuit.
Piriformis syndrome may be a secondary perpetuating factor underlying chronic
posttraumatic intractable LBP. Negligent misdiagnosis or delayed diagnosis of
this condition has caused a significant degree of unnecessary disability and
financial loss.
Special Concerns:
In female patients, piriformis syndrome may be a cause of dyspareunia, but, again,
this connection becomes impossible to prove. Diagnosis of piriformis syndrome requires
a high index of suspicion by either the primary care physician or the obstetric/
gynecologic specialist/surgeon. A bimanual simultaneous vaginal-rectal examination
of female patients to determine this soft tissue diagnosis helps the physician to
prescribe appropriate treatment.
Although it is a misdiagnosed etiology of LBP/sciatica, piriformis syndrome can
be a significant cause of soft tissue pain and disability. This problem requires
a skillful, attentive physician to conduct a thorough history/physical examination
that provides an accurate diagnosis. Once the clinical diagnosis has been made, a
specific treatment can be formulated to provide the best outcome with a minimal degree
of long-term disability.
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis).
In the piriformis syndrome, the irritation extends to the full thickness
of the nerve (sciatic neuritis).
BIBLIOGRAPHY Section 10 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Barton PM: Piriformis syndrome: a rational approach to management. Pain 1991 Dec; 47(3):
345-52[Medline].
Beatty RA: The piriformis muscle syndrome: a simple diagnostic maneuver. Neurosurgery
1994; 34: 512-514[Medline].
Beauchesne RP, Schutzer SF: Myositis ossificans of the piriformis muscle: an unusual
cause of piriformis syndrome. A case report. J Bone Joint Surg Am 1997 Jun; 79(6):
906-10[Medline].
Brown JA, Braun MA, Namey TC: Piriformis syndrome in a 10-year-old boy as a complication
of operation with the patient in the sitting position. Neurosurgery 1988 Jul; 23(1):
117-9[Medline].
Durrani Z, Winnie AP: Piriformis muscle syndrome: an under diagnosed cause of sciatica.
J Pain Symptom Manage 1991 Aug; 6(6): 374-9[Medline].
Fishman LM, Zybert PA: Electrophysiologic evidence of piriformis syndrome. Arch Phys
Med Rehabil 1992 Apr; 73(4): 359-64[Medline].
Freidberg AH: Sciatic pain and its relief by operation on muscle and fascia. Arch
Surg 1937; 34: 337-349.
Frymoyer JW: Back pain and sciatica. N Engl J Med 1988 Feb 4; 318(5): 291-300[Medline].
Jankiewicz JJ, Hennrikus WL, Houkom JA: The appearance of the piriformis muscle
syndrome in computed tomography and magnetic resonance imaging. A case report and
review of the literature. Clin Orthop 1991 Jan; (262): 205-9[Medline].
Karl RD Jr, Yedinak MA, Hartshorne MF: Scintigraphic appearance of the piriformis
muscle syndrome. Clin Nucl Med 1985 May; 10(5): 361-3[Medline].
Mizuguchi T: Division of the piriformis muscle for the treatment of sciatica.
Postlaminectomy syndrome and osteoarthritis of the spine. Arch Surg 1976 Jun; 111(6):
719-22[Medline].
Noftal F: The Piriformis Syndrome. Can J Surg 1988 Jul; 31(4): 210[Medline].
Pace JB, Nagle D: Piriformis syndrome. West J Med 1976 Jun; 124(6): 435-9[Medline].
Papadopoulos SM, McGillicuddy JE, Albers JW: Unusual cause of "piriformis muscle
syndrome". Arch Neurol 1990 Oct; 47(10): 1144-6[Medline].
Parziale JR, Hudgins TH, Fishman LM: The piriformis syndrome. Am J Orthop 1996
Dec; 25(12): 819-23[Medline].
Rask MR: Superior gluteal nerve entrapment syndrome. Muscle Nerve 1980 Jul-Aug;
3(4): 304-7[Medline].
Retzlaff EW, Berry AH, Haight AS: The piriformis muscle syndrome. J Am Osteopath
Assoc 1974 Jun; 73(10): 799-807[Medline].
Robinson D: Piriformis syndrome in relation to sciatic pain. Am J Surg 1947;
73: 355-358.
Schiowitz S: Facilitated positional release. J Am Osteopath Assoc 1990 Feb;
90(2): 145-6, 151-5[Medline].
Steiner C, Staubs C, Ganon M: Piriformis syndrome: pathogenesis, diagnosis,
and treatment. J Am Osteopath Assoc 1987 Apr; 87(4): 318-23[Medline].
TePoorten BA: The piriformis muscle. J Am Osteopath Assoc 1969 Oct; 69(2):
150-60[Medline].
Thiele GH: Tonic spasm of the levator ani, coccygeus and piriformis muscles.
Trans Am Proct Soc 1936; 37: 145-155.
Uchio Y, Nishikawa U, Ochi M: Bilateral Piriformis Syndrome after Total Hip
Arthroplasty. Arch Orthop Trauma Surg 1988; 117: 177-179.
Yeoman W: The relation of arthritis of the sacroiliac joint to sciatica.
Lancet 1928; ii: 1119-1122.
NOTE:
Medicine is a constantly changing science and not all therapies are clearly
established. New research changes drug and treatment therapies daily. The authors,
editors, and publisher of this journal have used their best efforts to provide
information that is up-to-date and accurate and is generally accepted within medical
standards at the time of publication. However, as medical science is constantly
changing and human error is always possible, the authors, editors, and publisher
or any other party involved with the publication of this article do not warrant
the information in this article is accurate or complete, nor are they responsible
for omissions or errors in the article or for the results of using this information.
The reader should confirm the information in this article from other sources prior
to use. In particular, all drug doses, indications, and contraindications should
be confirmed in the package insert.
FULL DISCLAIMER
Medicine is a constantly changing science and not all therapies are clearly established.
New research changes drug and treatment therapies daily. The authors, editors, and
publisher of this journal have used their best efforts to provide information that
is up-to-date and accurate and is generally accepted within medical standards at the
time of publication. However, as medical science is constantly changing and human
error is always possible, the authors, editors, and publisher or any other party
involved with the publication of this article do not warrant the information in this
article is accurate or complete, nor are they responsible for omissions or errors
in the article or for the results of using this information. The reader should
confirm the information in this article from other sources prior to use. In particular,
all drug doses, indications, and contraindications should be confirmed in the package
insert.
----
: Arch Surg. 1976 Jun;111(6):719-22. Related Articles, Link
Division of the piriformis muscle for the treatment of sciatica. Postlaminectomy
syndrome and osteoarthritis of the spine.
Mizuguchi T.
Division of the piriformis muscle at its tendinous insertion was employed for the
treatment of sciatica in 14 patients with post laminectomy syndrome and osteoarthritis
of the spine. Of these patients, 85% had satisfactory results. It is logical that the
piriformis muscle can play an important role in the production of sciatic associated
with intraspinal lesions. Tension on the sciatic nerve, which passes in close approximation
to the piriformis muscle anteriorly, can be relieved by division of the piriformis
muscle.
----
1: Neurosurgery. 1994 Mar;34(3):512-4; discussion 514. Related Articles, Link
Comment in:
Neurosurgery. 1994 Sep;35(3):545.
The piriformis muscle syndrome: a simple diagnostic maneuver.
Beatty RA.
Department of Neurosurgery, University of Illinois, College of Medicine, Chicago.
Current maneuvers to diagnose the piriformis syndrome are less than ideal. Freiberg's
maneuver of forceful internal rotation of the extended thigh elicits buttock pain by
stretching the piriformis muscle, and Pace's maneuver elicits pain by having the patient
abduct the legs in the seated position, which causes a contraction of the piriformis
muscle. This report describes a maneuver performed by the patient lying with the painful
side up, the painful leg flexed, and the knee resting on the table. Buttock pain is
produced when the patient lifts and holds the knee several inches off the table. The
maneuver produced deep buttock pain in three patients with piriformis syndrome. In 100
consecutive patients with surgically documented herniated lumbar discs, the maneuver
often produced lumbar and leg pain but not deep buttock pain. In 27 patients with
primary hip abnormalities, pain was often produced in the trochanteric area but not
in the buttock.
he maneuver described in this report was helpful in diagnosing the piriformis syndrome.
It relies on contraction of the muscle, rather than stretching, which the author believes
better reproduces the actual syndrome.
Publication Types:
Case Reports
PMID: 8190228 [PubMed - indexed for MEDLINE]
----
Muscle Nerve. 1980 Jul-Aug;3(4):304-7. Related Articles, Link
Superior gluteal nerve entrapment syndrome.
Rask MR.
Entrapment of the superior gluteal nerve can occur as a result of compression by
anterior-superior tendinous fibers of the piriformis muscle and cause aching claudication
-type buttock pain, weakness of abduction of the affected hip with a waddling gait, and
tenderness to palpation in the area of the buttock super lateral to the greater sciatic
notch. Instilling anesthetic into the point of entrapment may relieve the pain completely
but superior gluteal neurolysis may be required to effect a permanent cure.
Publication Types:
Case Reports
PMID: 7412775 [PubMed - indexed for MEDLINE]
-------------------------------------------------------------------------------
1: Clin Nucl Med. 1985 May;10(5):361-3. Related Articles, Link
Scintigraphic appearance of the piriformis muscle syndrome.
Karl RD Jr, Yedinak MA, Hartshorne MF, Cawthon MA, Bauman JM, Howard WH, Bunker SR.
This is the first report in the nuclear medicine literature of the scintigraphic
appearance of the piriformis muscle syndrome. This syndrome previously has been
thought to be a purely clinical diagnosis and imaging modalities have been ignored.
However, its confusing clinical presentation can lead to unnecessary surgical exploration
This case is presented to illustrate the characteristic scintigraphic pattern and
suggest the role of nuclear medicine scanning in establishing the diagnosis.
Publication Types:
Case Reports
PMID: 3160520 [PubMed - indexed for MEDLINE]
-------------------------------------------------------------------------------
1: Arch Surg. 1976 Jun;111(6):719-22. Related Articles, Link
Division of the piriformis muscle for the treatment of sciatica. Post laminectomy
syndrome and osteoarthritis of the spine.
Mizuguchi T.
Division of the piriformis muscle at its tendinous insertion was employed for the
treatment of sciatica in 14 patients with post laminectomy syndrome and osteoarthritis
of the spine. Of these patients, 85% had satisfactory results. It is logical that
the piriformis muscle can play an important role in the production of sciatic
associated with intraspinal lesions. Tension on the sciatic nerve, which passes
in close approximation to the piriformis muscle anteriorly, can be relieved by
division of the piriformis muscle.
PMID: 1275705 [PubMed - indexed for MEDLINE]
---
Link
Science for the Brain - Related Articles:
The nation's leading supporter of biomedical research on disorders of the brain
and nervous system
More about Piriformis Syndrome
Studies with patients
Research literature
Press releases
Search NINDS...
NINDS is part of the National Institutes of Health:
You are here: Home > Disorders > Piriformis Syndrome
NINDS Piriformis Syndrome Information Page
Organizations
What is Piriformis Syndrome?
Piriformis syndrome is a rare neuromuscular disorder that occurs when the piriformis
muscle compresses or irritates the sciatic nerve-the largest nerve in the body. The
piriformis muscle is a narrow muscle located in the buttocks. Compression of the
sciatic nerve causes pain-frequently described as tingling or numbness-in the buttocks
and along the nerve, often down to the leg. The pain may worsen as a result of sitting
for a long period of time, climbing stairs, walking, or running.
Is there any treatment?
Generally, treatment for the disorder begins with stretching exercises and massage.
Anti-inflammatory drugs may be prescribed. Cessation of running, bicycling, or similar
activities may be advised. A corticosteroid injection near where the piriformis muscle
and the sciatic nerve meet may provide temporary relief. In some cases, surgery is
recommended.
What is the prognosis?
The prognosis for most individuals with piriformis syndrome is good. Once symptoms
of the disorder are addressed, individuals can usually resume their normal activities.
In some cases, exercise regimens may need to be modified in order to reduce the likelihood
of recurrence or worsening.
What research is being done?
Within the NINDS research programs, piriformis syndrome is addressed primarily through
studies associated with pain research. NINDS vigorously pursues a research program seeking
new treatments for pain and nerve damage with the ultimate goal of reversing debilitating
conditions such as piriformis syndrome.
---
Piriformis Syndrome: Link
New minimal access, outpatient surgery developed at INM greatly improves outcome
and reduces recovery time
Family practice Physician
Chapel Medical Clinic
9739 California Avenue
South Gate, CA 90280
Phone: 323-567-1212
-------------------------------------------------------------------------------
Ebenezer Chambi: Dialogue with an Adventist physician, health educator, and
community leader Link
Ebenezer Chambi MD - Chambi Ebenezer MD
9739 California Ave
South Gate, CA 90280
Phones: (323) 564-2228
by Michael Peabody
Born in Peru, Dr. Ebenezer Chambi developed early in his life a sense of community
and an inclination to service. His family was active in the local church. Throughout
his educational experience, he was guided by a commitment to help others. In 1970,
he completed his pre-medical studies at Union College (now Peru Union University)
located near Lima, the capital. Although he wanted to study medicine in his homeland,
the then prevailing political situation made this virtually impossible. His older
brothers had moved to Mexico to pursue their medical training; so did he.
Completing his medical degree from the Autonomous University of Guadalajara, Mexico,
in 1975, he did his residencies in Puerto Rico and Los Angeles, California. After
completing the latter, Dr. Ebenezer Chambi joined a research team to study epilepsy.
Currently, he is practicing general medicine at the Chapel Medical Clinic in South
Gate, California. In addition to ensuring quality care to his patients, Dr. Ebenezer
Chambi brings his Christian commitment to bear on his profession by continually
promoting preventive care and healthful living. He is involved in his community through
a variety of activities ranging from sponsoring folk music concerts to speaking to
high school students on health. In recognition of his community service, he received
in 1994 the La Sierra University Presidential Citation for Humanitarian Service.
Ebenezer Chambi and his wife, Esther, have three children who are pursuing advanced
studies: Esther Janet, Ebenezer Howard, and Eber Caleb.
Dr. Ebenezer Chambi, what influences have shaped your life?
Perhaps the same four major influences that shape all of us: family, education,
community, and religion. The family teaches us how to care for each other. Parents
care for children, children care for each other and their parents. In a good home,
we learn to love people unconditionally. Education is one of the major ways to learn
about ourselves and develop our talents and intellectual skills. It structures our
personality. Community teaches us that we are not alone-no one is an island. We
depend on other people and they depend on us. Christianity gives us inner strength,
especially when we feel discouraged and don't have energy to keep going. There is a
higher power, God, ready to help us. Religion gives us the powerful tool of confidence.
It brings us strength and hope. It keeps us from giving up on life. At the end of
the journey, it gives us the assurance of a better life.
What type of research did you do in epilepsy?
Epilepsy can be a very debilitating disease, and our team wanted to find its cause
and determine whether it could be successfully treated or even cured. We studied a
diverse population in the Los Angeles area, seeking ways of helping epilepsy victims.
The results were rewarding. Some were cured. Many were able to live relatively normal
lives and return to their vocations.
Currently, what does your practice cover?
I am involved in general practice. Beyond the regular treatment of patients, I focus
on preventive medicine. I want to teach people how to live healthier, happier lives.
In my practice, I see a lot of baby boomers. I'm one of them, so I know what they are
like and how they live. Because they work so many hours and have so many activities,
they often wait until the last possible moment to come to see me, knowing that a visit
to the doctor takes time. They usually don't come in when they have a slight cold or
a stomach ache. They visit my office only when they sense that they are in serious
trouble and need help. We do a complete check-up, including blood and urine tests.
Most of the time we find that they have high cholesterol levels; they are not eating
right and not exercising. Most of the common problems can be prevented, and I emphasize
that.
How do you convince busy people to live healthier lives?
The key is behavior modification. We can give objective explanations of why a person
should exercise more or spend some time relaxing rather than overworking, but it is
challenging to convince people that they need to make fundamental changes in how they
live. At times a physician needs to be quite direct, even blunt, to persuade patients
to radically alter their lifestyle.
A while back, a man, suffering from exhaustion, came to my office. He was working at
two jobs so he could buy a new house every year. His wife told me that he worked too
many hours a day and did not take time to relax and enjoy life. She told me that they
already owned three homes and that he wanted to buy another one. I told her, "Don't
worry. The more he works, the more houses he will leave to you when he dies!" He got
the message and changed his habits.
Do you also utilize the media to educate the public?
When I was doing my residence in Puerto Rico, I started a radio program on health
prevention and promotion. Then here, in the Los Angeles area, I hosted for ten years
a weekly radio forum called El Médico Habla (The Physician Speaks) that was quite
popular. We have also prepared several short video programs on health that I make
available to pastors and TV cable stations.
Does the emphasis on exercise and nutrition in the popular media help in having
people change their lifestyle?
Yes. Ten or 15 years ago, it was more difficult to convince people that they needed
to exercise and eat well. But now, the media's coverage of prevention and health has
made my job easier in terms of education. The problem is that many people who understand
the principles of healthful living aren't putting them into practice. They still eat
too much fast food and stay up too late watching the late shows.
Fortunately, people are beginning to see the light. The city where I practice has a
park where you can see more people running, walking, and doing other exercises than
in any other park in the nearby cities. I like to think this has something to do with
our emphasis on exercise.
The hamburger place that is near our office now also sells vegetarian burgers. I think
that shows some of the positive influence we've had on people who are trying to eat
more healthful foods.
How can people who are not involved in the health-care profession effectively spread
the message of healthful living?
All of us exert an influence and convey a silent message wherever we go. People are
searching for a better life, and they look up to good role models. If we spend time
with people, we can influence them positively by your example. I've found it effective
not to preach at people, but rather to lead by example. We can encourage others to see
that there's a better life.
It's easy to become so focused on our own studies or profession that we forget that
we are part of a larger community outside our walls. How can a person who has become
so insulated begin to interact with the larger community beyond their family or church?
Before I became active in the community, it was easy to be critical of those outside
my circle. But after I became involved, I discovered how much good I could do and how
much I enjoyed it.
Get to know other people, especially those with whom we would not normally associate.
It will help with your social and intellectual development. You will also learn how
your community works and how you can help.
Becoming involved begins with something as simple as the way you greet people. Start
with a solid and sincere, "Good morning. How are you?" Speak words of encouragement.
Learn to listen. Meet with the people who are having problems in your area of expertise
who don't know where to look for help. Focus on relieving their suffering.
A few years ago, an earthquake hit the Los Angeles area. When people asked me why I
left my office to volunteer in the relief efforts, I told them that I was just paying
part of my debt to my community. The community has given me a lot and I want to give
back. It's a two-way street.
And don't forget to have fun! One of the things I do is organize folk-music concerts.
And though lots of people enjoy them, I enjoy them the most!
How do you apply this involvement in your church?
I love my church like a family. I do things not to be recognized or rewarded, but
because I want to do something for Christ and my church. If you start a project with
the goal of being recognized for your efforts, you miss the point. Instead, do the
job because it is important and necessary.
As a successful physician, a health educator, and community leader, what would your
counsel be to people who are just entering their careers?
Learn from successful people by watching how they live, how they get along with
others, and how they maintain their emotional balance. Emulate their good traits.
If I retrace my journey, being active in the church and in the community were the
most important factors that kept me on track. Those of us who have been blessed by
talents and education can do much good. Put yourself where God can use your skills.
Take the initiative to help the community and make people's lives better. That is
a worthwhile goal in life.
Interview by Michael Peabody. Michael Peabody is a third year law student at Pepperdine
University in Malibu, California. E-mail: mdpeabod@pepperdine.edu
Dr. Ebenezer Chambi's address: 9739 California Ave.; South Gate, California 90280; U.S.A.
-------------------------------------------------------------------------------
Orthopedics Link
Information about diagnosis and treatment of piriformis syndrome
What is piriformis syndrome?
Good question! No one really knows exactly what causes piriformis syndrome, or
if it really exists. Some physicians believe that piriformis syndrome is the
name given to hip/buttock pain that cannot be otherwise diagnosed. Others believe
that piriformis syndrome is a very real cause of pain and disability.
What is the piriformis muscle?
The piriformis is a muscle that travels behind the hip joint. The piriformis
muscle is small compared to other muscles around the hip and thigh, and it
aids in external rotation (turning out) of the hip joint. The piriformis muscle
and its tendon have an intimate relationship to the sciatic nerve--the largest
nerve in the body--which supplies the lower extremities with motor and sensory
function. The piriformis tendon and sciatic nerve cross each other behind the
hip joint, in the deep buttock. Both structures are about one centimeter in
diameter.
What do people think happens in piriformis syndrome?
It is thought that the piriformis muscle tendon may be tethering the sciatic
nerve, and causing an irritation to the nerve. While it has not be proven,
the theory supported by some physicians is that when the piriformis muscle
and its tendon are too tight, the sciatic nerve is choked. This may decrease
the blood flow to the nerve and irritate the nerve because of pressure.
What else may be causing this pain?
Sometimes referred to as "deep buttock pain," other causes of this type of
pain include spine problems (including herniated discs, spinal stenosis, etc.),
sciatica, and tendonitis. The diagnosis of piriformis syndrome is often given
when all of these diagnoses are eliminated as possible causes of pain. Other
signs of piriformis syndrome include examination maneuvers that attempt to
isolate the function of this muscle, and the finding of pain directly over
the tendon of the piriformis muscle.
Is there any treatment for piriformis syndrome?
Unfortunately, the treatment of piriformis syndrome is quite general, and
often this is a difficult problem to recover from. Some treatment suggestions are:
1. Physical Therapy - Emphasis on stretching and strengthening the hip rotator
muscles
2. Rest - Avoid the activities that cause symptoms for at least a few weeks
3. Anti-Inflammatory Medication - To decrease inflammation around the tendon
4. Deep Massage - Advocated by some physicians
5. On some occasions, when these treatments fail, patients have surgery to
release, or loosen, the piriformis muscle tendon. This surgery is not a
small procedure, and generally considered the last resort if a lengthy
period of conservative treatment does not solve the problem.
=============================================================================
eMedicine Specialties > Physical Medicine and Rehabilitation > Lower Limb Musculoskeletal
Conditions Link
Piriformis Syndrome
Last Updated: June 14, 2004 Rate this Article
Email to a Colleague
Synonyms and related keywords: hip socket neuropathy, pseudosciatica, wallet sciatica,
deep gluteal syndrome, piriformis syndrome
AUTHOR INFORMATION Section 1 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Author: Milton J Klein, DO, Consulting Staff, Department of Physical Medicine and
Rehabilitation, Sewickley Valley Hospital and Ohio Valley General Hospital
Milton J Klein, DO, is a member of the following medical societies: American Academy
of Disability Evaluating Physicians, American Academy of Osteopathy, American Academy
of Physical Medicine and Rehabilitation, American Association of Electrodiagnostic
Medicine, American Medical Association, American Osteopathic Association, and American
Osteopathic College of Physical Medicine and Rehabilitation
Editor(s): Rajesh R Yadav, MD, Assistant Professor, Section of Physical Medicine
and Rehabilitation, MD Anderson Cancer Center, University of Texas at Houston;
Francisco Talavera, PharmD, PhD, Senior Pharmacy Editor, Pharmacy, eMedicine;
Michael T Andary, MD, MS, Residency Program Director, Associate Professor,
Department of Physical Medicine and Rehabilitation, Michigan State University
College of Osteopathic Medicine; Kelly L Allen, MD, Consulting Staff, Department
of Physical Medicine and Rehabilitation, Lourdes Regional Rehabilitation Center,
Our Lady of Lourdes Medical Center; and Consuelo T Lorenzo, MD, Consulting Staff,
Department of Physical Medicine and Rehabilitation, Alegent Health Care, Immanuel
Rehabilitation Center
INTRODUCTION Section 2 of 10
Author Information Introduction Clinical Differentials Workup Treatment
Follow-up Miscellaneous Pictures Bibliography
Background: Piriformis syndrome has remained a controversial diagnosis since
its initial description in 1928. Piriformis syndrome usually is caused by neuritis
of the proximal sciatic nerve. The piriformis muscle can either irritate or compress
the proximal sciatic nerve due to spasm and/or contracture, and this problem can
mimic discogenic sciatica (pseudosciatica).
Pathophysiology: The piriformis muscle is flat, pyramid-shaped, and oblique.
This muscle originates to the anterior of the S2-S4 vertebrae, the sacrotuberous
ligament, and the upper margin of the greater sciatic foramen (see Image 1).
This muscle passes through the greater sciatic notch and inserts on the superior
surface of the greater trochanter of the femur. With the hip extended, the piriformis
muscle is the primary external rotator; however, with the hip flexed, the piriformis
muscle itself becomes a hip abductor. This muscle is innervated by branches from
L5, S1, and S2. A lower lumbar radiculopathy also may cause secondary irritation
of the piriformis muscle, which may complicate the diagnosis and hinder patient
progress.
Many developmental variations of the relationship between the sciatic nerve in
the pelvis and piriformis muscle have been observed. In approximately 20% of the
population, the muscle belly is split with one or more parts of the sciatica
nerve dividing the muscle belly itself. In 10% of the population, the tibial/peroneal
divisions are not enclosed in a common sheath. Usually, the peroneal portion splits the
piriformis muscle belly; the tibial division rarely splits the muscle belly.
Involvement of the superior gluteal nerve usually is not seen in cases of piriformis
syndrome. This nerve leaves the sciatic nerve trunk and passes through the canal
above the piriformis muscle.
Blunt injury may cause hematoma formation and subsequent scarring between the sciatic
nerve and short external rotators. Nerve injury can occur with prolonged pressure on
the nerve or vasa nervorum.
Etiology can be subdivided into a few categories as follows:
Hyperlordosis
Muscle anomalies with hypertrophy
Fibrosis (due to trauma)
Partial or total nerve anatomical abnormalities
Other causes can include the following:
Pseudo aneurysms of the inferior gluteal artery adjacent to the piriformis syndrome
Bilateral piriformis syndrome due to prolonged sitting during an extended
neurosurgical procedure
Cerebral palsy
Total hip arthroplasty
Myositis ossificans
Vigorous physical activity
This syndrome remains controversial because, in most cases, the diagnosis is clinical,
and no confirmatory tests exist to support the clinical findings.
Frequency:
In the US: Given the lack of agreement on exactly how to diagnose this condition,
estimates of frequency of sciatica caused by piriformis syndrome vary from rare to
approximately 6% of sciatica cases seen in a general family practice.
Approximately 90% of adults have had at least one episode of disabling LBP in their
lifetime.
Mortality/Morbidity: Piriformis syndrome is not life-threatening, but it can have
significant associated morbidity. The total cost of low back pain (LBP) and sciatica is
significant, exceeding $16 billion in both direct and indirect costs.
Sex: Some reports suggest a 6:1 female-to-male predominance. CLINICAL Section
3 of 10 Author Information Introduction Clinical Differentials Workup Treatment
Follow-up Miscellaneous Pictures Bibliography
History: Piriformis syndrome often is not recognized as a cause of LBP and associated
sciatica. This clinical syndrome is due to a compression of the sciatic nerve by the
piriformis muscle. This condition is identical in clinical presentation to LBP with
associated L5, S1 radiculopathy due to discogenic and/or lower lumbar facet arthropathy
with foraminal narrowing. Not uncommonly, patients demonstrate both of these clinical
entities simultaneously. This diagnostic dilemma highlights the need for patients with
LBP and associated radicular pain to undergo a complete history and physical examination,
including a digital rectal examination.
Many cases of refractory trochanteric bursitis are observed to have an underlying occult
piriformis syndrome due to the insertion of the piriformis muscle on the greater
trochanter of the hip. If both the trochanteric bursitis and the piriformis syndrome
are treated inadequately, both conditions remain resistant to medical management.
Physical: Examination findings may include the following:
Piriformis muscle spasm often is detected by careful deep palpation.
Digital rectal examination may reveal tenderness on lateral pelvic wall that
reproduces symptoms.
Reproduction of sciatica type pain with weakness is noted by resisted abduction/external
rotation (Pace test).
The Freiberg test is another diagnostic sign that elicits pain upon forced internal
rotation of the extended thigh.
The Beatty maneuver reproduces buttock pain by selectively contracting the piriformis
muscle. The patient lies on the uninvolved side and abducts the involved thigh upward;
this activates the ipsilateral piriformis muscle, which is both a hip external rotator
and abductor with the hip flexed.
A painful point may be present at the lateral margin of the sacrum.
Shortening of the involved lower extremity may be seen.
The patient may have difficulty sitting due to an intolerance of weight bearing on
the buttock.
The patient may have the tendency to demonstrate a splayed foot on the involved side
when in the supine position.
Piriformis syndrome alone is rarely a cause of a focal neuromuscular impairment; either
a sciatic mononeuropathy or an L5-S1 radiculopathy can mimic both of these conditions,
obscuring diagnosis of piriformis syndrome.
A Morton foot may predispose the patient to developing piriformis syndrome. The
prominent second metatarsal head destabilizes the foot during the push-off phase
of the gait cycle, causing foot pronation and internal rotation of the lower limb.
The piriformis muscle (external hip rotator) reactively contracts repetitively during
each push-off phase of the gait cycle as a compensatory mechanism, leading to piriformis
syndrome.
Causes: Approximately 50% of patients with piriformis syndrome have a history of trauma,
with either a direct buttock contusion or hip/lower back torsional injury. The remaining
50% of cases are of spontaneous onset, so the treating physician must have a high index of
suspicion for this problem, lest it be overlooked.
DIFFERENTIALS Section 4 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Lumbar Degenerative Disc Disease
Lumbar Facet Arthropathy
Lumbar Spondylolysis and Spondylolisthesis
Myofascial Pain
Trochanteric Bursitis
Other Problems to be Considered:
Lumbosacral radiculopathy
Buttock pain
Ischial tuberosity bursitis
Sciatica
Check the Internet for Related Articles:
Lumbar Degenerative Disc Disease
Lumbar Facet Arthropathy
Lumbar Spondylolysis and Spondylolisthesis
Myofascial Pain
Trochanteric Bursitis
Continuing Education
CME available for this topic. Click here to take this CME.
WORKUP Section 5 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Lab Studies:
Laboratory studies generally are not indicated in diagnosing piriformis syndrome.
Imaging Studies:
Diagnostic imaging of the lumbar spine is mandatory to exclude associated discogenic
and/or osteoarthritic contributing pathology.
Reports in the literature on piriformis muscle describe imaging by nuclear
diagnostic studies and MRI of the pelvis, but these tests are neither practical
nor reliable diagnostic approaches to this problem. The history and clinical
diagnostic examination provide the greatest and most specific diagnostic yield
for this problem.
Other Tests:
Results of electrodiagnostic testing for piriformis syndrome usually are normal.
Reports of positional H-reflex abnormalities can be found in the literature;
however, such findings have not been widely accepted or reproduced.
TREATMENT Section 6 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Rehabilitation Program:
Physical Therapy: Because a definitive method to accurately diagnose this problem
is not available, treatment regimens are controversial and have not been subjected
to randomized blind clinical trials. Despite this fact, numerous treatment strategies
exist for patients with piriformis syndrome.
Functional biomechanical deficits may include the following:
Tight piriformis muscle
Tight hip external rotators and adductors
Hip abductor weakness
Lower lumbar spine dysfunction
Sacroiliac joint hypomobility
Functional adaptations to these deficits include the following:
Ambulation with thigh in external rotation
Functional limb length shortening
Shortened stride length
Once the diagnosis has been made, these underlying perpetuating biomechanical factors
must be corrected.
Consider the use of ultrasound and other heat modalities prior to physical therapy
sessions. Prior to performing piriformis stretches, the hip joint capsule should be
mobilized anteriorly and posteriorly to allow for more effective stretching. Soft
tissue therapies of the piriformis muscle can be helpful, including longitudinal
gliding with passive internal hip rotation, as well as transverse gliding and sustained
longitudinal release with the patient lying on his/her side. Addressing sacroiliac
joint and low back dysfunction also is important.
A home stretching program should be provided to the patient. These stretches are an
essential component of the treatment program. During the acute phase of treatment,
stretching every 2-3 hours (while awake) is a key to the success of non operative
treatment. Prolonged stretching of the piriformis muscle is accomplished in either
a supine or orthostatic position with the involved hip flexed and passively adducted/
internally rotated.
Medical Issues/Complications: No consensus exists on overall treatment of piriformis
syndrome due to lack of objective clinical trials. Conservative treatment (eg,
stretching, manual techniques, injections, activity modifications, modalities like
heat or ultrasound, natural healing) is successful in most cases.
Injection therapy can be incorporated if the situation is refractory to the
aforementioned treatment program. For effective injection, the piriformis muscle
must be localized manually by digital rectal examination. Then the piriformis muscle
is injected using a 3.5-inch (8.9-cm) spinal needle. Care must be taken to avoid
direct injection of the sciatic nerve.
Surgical Intervention: Surgical management is the treatment of last resort. Surgery
for this condition involves resection of the muscle itself or the muscle tendon
near its insertion at the superior aspect of the greater trochanter of the femur
(as described by Mizuguchi). These surgical procedures are described as effective,
and they do not cause any associated superimposed postoperative disability.
Consultations:
Because of the enigmatic nature of piriformis syndrome, initial consultation obtained
from an orthopedic surgeon or similar specialist usually is nonspecific. This disorder
is considered to be a soft tissue problem that presents as low back or buttock pain
with sciatica. After all differential diagnoses have been excluded, consider piriformis
syndrome. Due to the traumatic etiology of most cases, piriformis syndrome usually is
associated with other more proximal causes of LBP, sciatica, and buttock pain (thereby
further clouding the diagnosis).
Other Treatment (injection, manipulation, etc.):
The Spray N' Stretch myofascial treatment and ultrasound modality preceding physical
therapy sessions are useful.
Manual muscle medicine, including facilitated positional release, may be helpful.
Injections with steroids, local anesthetics, and botulinum toxin have been reported
in the literature for this condition. No single technique is universally accepted.
Localization techniques include manual localization of muscle with fluoroscopic and
electromyographic guidance. The piriformis muscle, after localization with a digital
rectal examination, can be injected with a 3.5-inch (8.9-cm) spinal needle. Care should
be taken to avoid direct injection of the sciatic nerve.
FOLLOW-UP Section 7 of 10
Author Information Introduction Clinical Differentials Workup Treatment
Follow-up Miscellaneous
Further Inpatient Care:
Inpatient care would be necessary only if surgical intervention is warranted.
Surgery is the last resort treatment for severe cases of piriformis syndrome.
Further Outpatient Care:
Piriformis syndrome usually is treated effectively with conservative measures.
Please refer to the Treatment section for a discussion of treatment recommendations.
Deterrence/Prevention:
No method has been demonstrated to prevent piriformis syndrome. The best prevention
is to maintain biomechanical balance by restoration of a more physiologic weight
bearing distribution with a level pelvis/sacral base and equal leg lengths, achieved
by heel lift therapy if necessary. This treatment approach also prevents recurrences
of piriformis syndrome, especially if the underlying etiology is a leg-length discrepancy.
The patient also must engage in a general stretching program that includes bilateral
piriformis muscles.
Complications:
The most significant complication is failure to recognize, diagnose, and treat this
disabling condition. If left untreated, a patient may undergo unsuccessful back
surgery for a disc herniation; however, a coexisting occult piriformis syndrome
can result in a failed back syndrome.
Another complication is inadvertent direct injection of the sciatic nerve, which
usually results in a non disabling and temporary sciatic mononeuropathy.
Prognosis:
The prognosis depends upon early recognition and treatment. As this is a soft
tissue syndrome, it has a tendency to be chronic, usually due to late diagnosis
and treatment and has a less favorable prognosis.
Patient Education:
For conservative measures to be effective, the patient must be educated with an
aggressive home-based stretching program to maintain piriformis muscle flexibility.
He or she must comply with the program even beyond the point of discontinuation of
formal medical treatment.
MISCELLANEOUS Section 8 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Medical/Legal Pitfalls:
The greatest medical/legal concern is either misdiagnosis or failure to diagnose
piriformis syndrome. In most cases, the diagnosis is one of exclusion. Therefore,
if piriformis syndrome is not in the differential diagnosis list, it may be overlooked.
The patient becomes a chronic pain patient doomed to a lifetime of disability and
chronic management with medication. Because the diagnosis usually is elusive, missing
the diagnosis does not constitute malicious negligence and, therefore, rarely would
be sufficient grounds alone for a medical malpractice lawsuit.
Piriformis syndrome may be a secondary perpetuating factor underlying chronic
posttraumatic intractable LBP. Negligent misdiagnosis or delayed diagnosis of
this condition has caused a significant degree of unnecessary disability and
financial loss.
Special Concerns:
In female patients, piriformis syndrome may be a cause of dyspareunia, but, again,
this connection becomes impossible to prove. Diagnosis of piriformis syndrome requires
a high index of suspicion by either the primary care physician or the obstetric/
gynecologic specialist/surgeon. A bimanual simultaneous vaginal-rectal examination
of female patients to determine this soft tissue diagnosis helps the physician to
prescribe appropriate treatment.
Although it is a misdiagnosed etiology of LBP/sciatica, piriformis syndrome can
be a significant cause of soft tissue pain and disability. This problem requires
a skillful, attentive physician to conduct a thorough history/physical examination
that provides an accurate diagnosis. Once the clinical diagnosis has been made, a
specific treatment can be formulated to provide the best outcome with a minimal degree
of long-term disability.
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Miscellaneous Pictures Bibliography
Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis).
In the piriformis syndrome, the irritation extends to the full thickness
of the nerve (sciatic neuritis).
BIBLIOGRAPHY Section 10 of 10
Author Information Introduction Clinical Differentials Workup Treatment Follow-up
Barton PM: Piriformis syndrome: a rational approach to management. Pain 1991 Dec; 47(3):
345-52[Medline].
Beatty RA: The piriformis muscle syndrome: a simple diagnostic maneuver. Neurosurgery
1994; 34: 512-514[Medline].
Beauchesne RP, Schutzer SF: Myositis ossificans of the piriformis muscle: an unusual
cause of piriformis syndrome. A case report. J Bone Joint Surg Am 1997 Jun; 79(6):
906-10[Medline].
Brown JA, Braun MA, Namey TC: Piriformis syndrome in a 10-year-old boy as a complication
of operation with the patient in the sitting position. Neurosurgery 1988 Jul; 23(1):
117-9[Medline].
Durrani Z, Winnie AP: Piriformis muscle syndrome: an under diagnosed cause of sciatica.
J Pain Symptom Manage 1991 Aug; 6(6): 374-9[Medline].
Fishman LM, Zybert PA: Electrophysiologic evidence of piriformis syndrome. Arch Phys
Med Rehabil 1992 Apr; 73(4): 359-64[Medline].
Freidberg AH: Sciatic pain and its relief by operation on muscle and fascia. Arch
Surg 1937; 34: 337-349.
Frymoyer JW: Back pain and sciatica. N Engl J Med 1988 Feb 4; 318(5): 291-300[Medline].
Jankiewicz JJ, Hennrikus WL, Houkom JA: The appearance of the piriformis muscle
syndrome in computed tomography and magnetic resonance imaging. A case report and
review of the literature. Clin Orthop 1991 Jan; (262): 205-9[Medline].
Karl RD Jr, Yedinak MA, Hartshorne MF: Scintigraphic appearance of the piriformis
muscle syndrome. Clin Nucl Med 1985 May; 10(5): 361-3[Medline].
Mizuguchi T: Division of the piriformis muscle for the treatment of sciatica.
Postlaminectomy syndrome and osteoarthritis of the spine. Arch Surg 1976 Jun; 111(6):
719-22[Medline].
Noftal F: The Piriformis Syndrome. Can J Surg 1988 Jul; 31(4): 210[Medline].
Pace JB, Nagle D: Piriformis syndrome. West J Med 1976 Jun; 124(6): 435-9[Medline].
Papadopoulos SM, McGillicuddy JE, Albers JW: Unusual cause of "piriformis muscle
syndrome". Arch Neurol 1990 Oct; 47(10): 1144-6[Medline].
Parziale JR, Hudgins TH, Fishman LM: The piriformis syndrome. Am J Orthop 1996
Dec; 25(12): 819-23[Medline].
Rask MR: Superior gluteal nerve entrapment syndrome. Muscle Nerve 1980 Jul-Aug;
3(4): 304-7[Medline].
Retzlaff EW, Berry AH, Haight AS: The piriformis muscle syndrome. J Am Osteopath
Assoc 1974 Jun; 73(10): 799-807[Medline].
Robinson D: Piriformis syndrome in relation to sciatic pain. Am J Surg 1947;
73: 355-358.
Schiowitz S: Facilitated positional release. J Am Osteopath Assoc 1990 Feb;
90(2): 145-6, 151-5[Medline].
Steiner C, Staubs C, Ganon M: Piriformis syndrome: pathogenesis, diagnosis,
and treatment. J Am Osteopath Assoc 1987 Apr; 87(4): 318-23[Medline].
TePoorten BA: The piriformis muscle. J Am Osteopath Assoc 1969 Oct; 69(2):
150-60[Medline].
Thiele GH: Tonic spasm of the levator ani, coccygeus and piriformis muscles.
Trans Am Proct Soc 1936; 37: 145-155.
Uchio Y, Nishikawa U, Ochi M: Bilateral Piriformis Syndrome after Total Hip
Arthroplasty. Arch Orthop Trauma Surg 1988; 117: 177-179.
Yeoman W: The relation of arthritis of the sacroiliac joint to sciatica.
Lancet 1928; ii: 1119-1122.
NOTE:
Medicine is a constantly changing science and not all therapies are clearly
established. New research changes drug and treatment therapies daily. The authors,
editors, and publisher of this journal have used their best efforts to provide
information that is up-to-date and accurate and is generally accepted within medical
standards at the time of publication. However, as medical science is constantly
changing and human error is always possible, the authors, editors, and publisher
or any other party involved with the publication of this article do not warrant
the information in this article is accurate or complete, nor are they responsible
for omissions or errors in the article or for the results of using this information.
The reader should confirm the information in this article from other sources prior
to use. In particular, all drug doses, indications, and contraindications should
be confirmed in the package insert.
FULL DISCLAIMER
Medicine is a constantly changing science and not all therapies are clearly established.
New research changes drug and treatment therapies daily. The authors, editors, and
publisher of this journal have used their best efforts to provide information that
is up-to-date and accurate and is generally accepted within medical standards at the
time of publication. However, as medical science is constantly changing and human
error is always possible, the authors, editors, and publisher or any other party
involved with the publication of this article do not warrant the information in this
article is accurate or complete, nor are they responsible for omissions or errors
in the article or for the results of using this information. The reader should
confirm the information in this article from other sources prior to use. In particular,
all drug doses, indications, and contraindications should be confirmed in the package
insert.
----
: Arch Surg. 1976 Jun;111(6):719-22. Related Articles, Link
Division of the piriformis muscle for the treatment of sciatica. Postlaminectomy
syndrome and osteoarthritis of the spine.
Mizuguchi T.
Division of the piriformis muscle at its tendinous insertion was employed for the
treatment of sciatica in 14 patients with post laminectomy syndrome and osteoarthritis
of the spine. Of these patients, 85% had satisfactory results. It is logical that the
piriformis muscle can play an important role in the production of sciatic associated
with intraspinal lesions. Tension on the sciatic nerve, which passes in close approximation
to the piriformis muscle anteriorly, can be relieved by division of the piriformis
muscle.
----
1: Neurosurgery. 1994 Mar;34(3):512-4; discussion 514. Related Articles, Link
Comment in:
Neurosurgery. 1994 Sep;35(3):545.
The piriformis muscle syndrome: a simple diagnostic maneuver.
Beatty RA.
Department of Neurosurgery, University of Illinois, College of Medicine, Chicago.
Current maneuvers to diagnose the piriformis syndrome are less than ideal. Freiberg's
maneuver of forceful internal rotation of the extended thigh elicits buttock pain by
stretching the piriformis muscle, and Pace's maneuver elicits pain by having the patient
abduct the legs in the seated position, which causes a contraction of the piriformis
muscle. This report describes a maneuver performed by the patient lying with the painful
side up, the painful leg flexed, and the knee resting on the table. Buttock pain is
produced when the patient lifts and holds the knee several inches off the table. The
maneuver produced deep buttock pain in three patients with piriformis syndrome. In 100
consecutive patients with surgically documented herniated lumbar discs, the maneuver
often produced lumbar and leg pain but not deep buttock pain. In 27 patients with
primary hip abnormalities, pain was often produced in the trochanteric area but not
in the buttock.
he maneuver described in this report was helpful in diagnosing the piriformis syndrome.
It relies on contraction of the muscle, rather than stretching, which the author believes
better reproduces the actual syndrome.
Publication Types:
Case Reports
PMID: 8190228 [PubMed - indexed for MEDLINE]
----
Muscle Nerve. 1980 Jul-Aug;3(4):304-7. Related Articles, Link
Superior gluteal nerve entrapment syndrome.
Rask MR.
Entrapment of the superior gluteal nerve can occur as a result of compression by
anterior-superior tendinous fibers of the piriformis muscle and cause aching claudication
-type buttock pain, weakness of abduction of the affected hip with a waddling gait, and
tenderness to palpation in the area of the buttock super lateral to the greater sciatic
notch. Instilling anesthetic into the point of entrapment may relieve the pain completely
but superior gluteal neurolysis may be required to effect a permanent cure.
Publication Types:
Case Reports
PMID: 7412775 [PubMed - indexed for MEDLINE]
-------------------------------------------------------------------------------
1: Clin Nucl Med. 1985 May;10(5):361-3. Related Articles, Link
Scintigraphic appearance of the piriformis muscle syndrome.
Karl RD Jr, Yedinak MA, Hartshorne MF, Cawthon MA, Bauman JM, Howard WH, Bunker SR.
This is the first report in the nuclear medicine literature of the scintigraphic
appearance of the piriformis muscle syndrome. This syndrome previously has been
thought to be a purely clinical diagnosis and imaging modalities have been ignored.
However, its confusing clinical presentation can lead to unnecessary surgical exploration
This case is presented to illustrate the characteristic scintigraphic pattern and
suggest the role of nuclear medicine scanning in establishing the diagnosis.
Publication Types:
Case Reports
PMID: 3160520 [PubMed - indexed for MEDLINE]
-------------------------------------------------------------------------------
1: Arch Surg. 1976 Jun;111(6):719-22. Related Articles, Link
Division of the piriformis muscle for the treatment of sciatica. Post laminectomy
syndrome and osteoarthritis of the spine.
Mizuguchi T.
Division of the piriformis muscle at its tendinous insertion was employed for the
treatment of sciatica in 14 patients with post laminectomy syndrome and osteoarthritis
of the spine. Of these patients, 85% had satisfactory results. It is logical that
the piriformis muscle can play an important role in the production of sciatic
associated with intraspinal lesions. Tension on the sciatic nerve, which passes
in close approximation to the piriformis muscle anteriorly, can be relieved by
division of the piriformis muscle.
PMID: 1275705 [PubMed - indexed for MEDLINE]
---
Link
Science for the Brain - Related Articles:
The nation's leading supporter of biomedical research on disorders of the brain
and nervous system
More about Piriformis Syndrome
Studies with patients
Research literature
Press releases
Search NINDS...
NINDS is part of the National Institutes of Health:
You are here: Home > Disorders > Piriformis Syndrome
NINDS Piriformis Syndrome Information Page
Organizations
What is Piriformis Syndrome?
Piriformis syndrome is a rare neuromuscular disorder that occurs when the piriformis
muscle compresses or irritates the sciatic nerve-the largest nerve in the body. The
piriformis muscle is a narrow muscle located in the buttocks. Compression of the
sciatic nerve causes pain-frequently described as tingling or numbness-in the buttocks
and along the nerve, often down to the leg. The pain may worsen as a result of sitting
for a long period of time, climbing stairs, walking, or running.
Is there any treatment?
Generally, treatment for the disorder begins with stretching exercises and massage.
Anti-inflammatory drugs may be prescribed. Cessation of running, bicycling, or similar
activities may be advised. A corticosteroid injection near where the piriformis muscle
and the sciatic nerve meet may provide temporary relief. In some cases, surgery is
recommended.
What is the prognosis?
The prognosis for most individuals with piriformis syndrome is good. Once symptoms
of the disorder are addressed, individuals can usually resume their normal activities.
In some cases, exercise regimens may need to be modified in order to reduce the likelihood
of recurrence or worsening.
What research is being done?
Within the NINDS research programs, piriformis syndrome is addressed primarily through
studies associated with pain research. NINDS vigorously pursues a research program seeking
new treatments for pain and nerve damage with the ultimate goal of reversing debilitating
conditions such as piriformis syndrome.
---
Piriformis Syndrome: Link
New minimal access, outpatient surgery developed at INM greatly improves outcome
and reduces recovery time
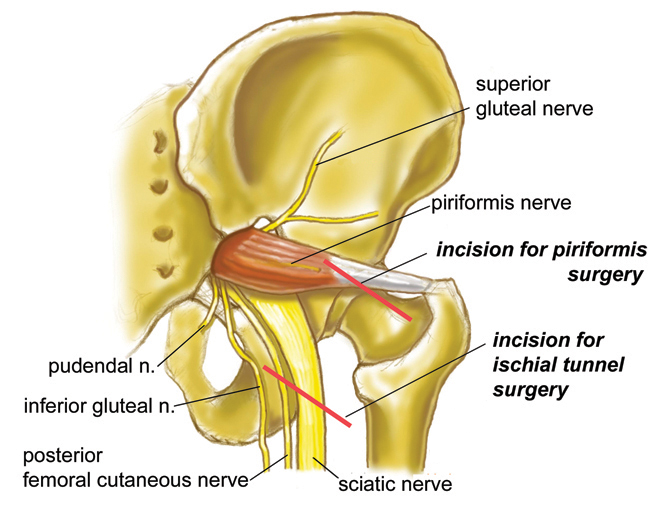 Piriformis Surgery Incision
Piriformis surgery is now a small procedure which can be carried out under local
anaesthetic as an outpatient. Traditional piriformis surgery is a large and debilitating
operation but no patient should be having these operations today. There were two types
of traditional piriformis surgery, one involves a large lateral hip incision similar
to the approach used for a hip replacement surgery. The second involves a very large
incision and involves completely detaching all of the gluteal muscles from the iliac
crest. Both of these types of surgery result in weeks of debilitation, walking on
crutches and pain, with only limited success treating the original problem.
The new type of "minimal access surgery" developed at the Institute for Nerve Medicine
by Dr. Aaron Filler involves only a small incision, and in most cases can be performed
on an outpatient basis. Large scale formal outcome trials involving hundreds of patients
with follow-up out to eight years show no detectable effect on normal walking in any
of the patients - this a great change from the traditional surgery that often leaves
permanent problems with gait. Recovery takes only a few days in most patients.
Those patients who have positive physical exam findings, positive MR neurography
findings and a clear positive response to MRI guided piriformis injection have had
a 85% to 90% good to excellent outcome.
---
Piriformis Syndrome & Sciatica Link
The nerve-related leg pain of Sciatica is often due to piriformis muscle syndrome.
Unlike the sciatica from a herniated disk, there is often little or no back pain
while buttock pain predominates. The pain is worse when sitting, relieved by standing
or walking, and often extends no farther down the leg than the ankle or mid-foot.
When toes are involved, it usually affects all five toes.
Piriformis Flexion Diagram
Piriformis Surgery Incision
Piriformis surgery is now a small procedure which can be carried out under local
anaesthetic as an outpatient. Traditional piriformis surgery is a large and debilitating
operation but no patient should be having these operations today. There were two types
of traditional piriformis surgery, one involves a large lateral hip incision similar
to the approach used for a hip replacement surgery. The second involves a very large
incision and involves completely detaching all of the gluteal muscles from the iliac
crest. Both of these types of surgery result in weeks of debilitation, walking on
crutches and pain, with only limited success treating the original problem.
The new type of "minimal access surgery" developed at the Institute for Nerve Medicine
by Dr. Aaron Filler involves only a small incision, and in most cases can be performed
on an outpatient basis. Large scale formal outcome trials involving hundreds of patients
with follow-up out to eight years show no detectable effect on normal walking in any
of the patients - this a great change from the traditional surgery that often leaves
permanent problems with gait. Recovery takes only a few days in most patients.
Those patients who have positive physical exam findings, positive MR neurography
findings and a clear positive response to MRI guided piriformis injection have had
a 85% to 90% good to excellent outcome.
---
Piriformis Syndrome & Sciatica Link
The nerve-related leg pain of Sciatica is often due to piriformis muscle syndrome.
Unlike the sciatica from a herniated disk, there is often little or no back pain
while buttock pain predominates. The pain is worse when sitting, relieved by standing
or walking, and often extends no farther down the leg than the ankle or mid-foot.
When toes are involved, it usually affects all five toes.
Piriformis Flexion Diagram
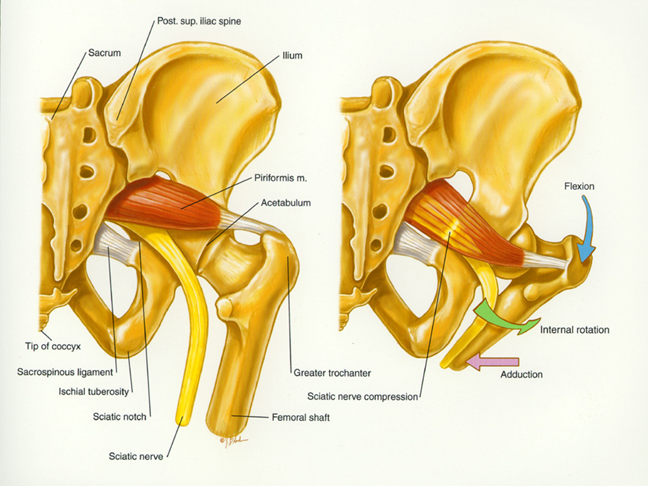 This drawing illustrates the important anatomy for piriformis syndrome and shows
how certain leg positions pull the piriformis muscle up against the sciatic nerve
causing buttock pain and radiating leg pain.
Piriformis Syndrome
Anatomy of the piriformis muscle and sciatic nerve
in a T1 weighted axial MRI scan
Piriformis Muscle Open MRI Anatomy Photo Link
This drawing illustrates the important anatomy for piriformis syndrome and shows
how certain leg positions pull the piriformis muscle up against the sciatic nerve
causing buttock pain and radiating leg pain.
Piriformis Syndrome
Anatomy of the piriformis muscle and sciatic nerve
in a T1 weighted axial MRI scan
Piriformis Muscle Open MRI Anatomy Photo Link
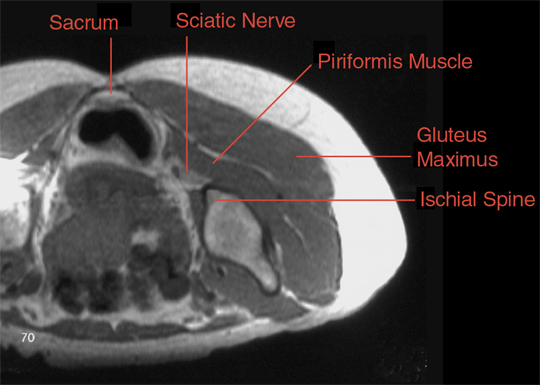 This T1 weighted axial MRI scan shows the anatomy used to guide the injection of the piriformis
muscle in an Open MRI scanner.
Link
to MR Images of hypersensitivity to left side of Piriformis Muscle
Piriformis Flexion Exam Manouver
This T1 weighted axial MRI scan shows the anatomy used to guide the injection of the piriformis
muscle in an Open MRI scanner.
Link
to MR Images of hypersensitivity to left side of Piriformis Muscle
Piriformis Flexion Exam Manouver
 Critical physical exam maneuver for muscle based piriformis syndrome: The patient's
foot is placed lateral to the contra lateral knee. Resisted abduction or adduction
against the examiner's hand may reproduce the symptoms. Straight leg rising is
typically negative. There is often relief obtained by traction on the involved leg,
particularly by pulling upwards at a ten to twenty degree angle and towards the
contra lateral side by a similar amount. The distribution of symptoms typically involves
both L5 (big toe) and S1 (small toe) components because this a pan-sciatic syndrome.
The symptoms often progress no further than the ankle in distinction to sciatica
from a lumbar disk which typically radiates into the toes. Link
---
SEARCH Receive Spine News patient>conditions>other
Piriformis Syndrome Spine Universe ChiropracticLink
Piriformis Syndrome is caused by an entrapment (pinching) of the sciatic nerve
as it exits the Greater Sciatic notch in the gluteal region. There are two normal
variations for the exit of the sciatic nerve in this region. The first places the
sciatic nerve inferior (below) to the Piriformis muscle and superior (above) the
gemellus muscle. Entrapment in this area is likely due to a myospasm or contracture
(tightening or shortening respectively) of either of these two muscles.
The second common site of entrapment is when the sciatic nerve actually pierces
the piriformis muscle itself. This can occur in about 1% to 10% of all humans.
In this case myospasm and or contraction of the piriformis muscle itself can lead
to pain along the back of the thigh to the knee, loss of sensation or numbness
and tingling in the sole of the foot. This particular syndrome can often mimic
its more notorious counterpart known as sciatica, and that being the case, it is
often misdiagnosed as sciatica. The main difference between sciatica and piriformis
syndrome is in the cause. Sciatica is directly due to a lumbar disc pressing on
the sciatic nerve as it exits the intervertebral foramen in the lumbar spine. What
both of these complaints have in common is that both can produce pain, numbness
and tingling below the knee and into the foot.
The main diagnostic tests performed by your doctor of Chiropractic is what
distinguishes one from the other. With piriformis syndrome your chiropractor
will not get positive tests results that indicate lumbar spine involvement.
Often the patient may not be aware that there is a problem. Some cases won't
show up until a complete neurological exam is performed on the lower extremity.
The patient may have chief complaints ranging from no pain to pain in the lower
back to gluteal pain to numbness and tingling in the foot. As can be seen the
symptoms in this condition can vary widely making the doctor who is not used to
differentially diagnosing this condition from sciatica confused as to the cause
of the condition.
Many weekend athletes and people who spend long hours sitting are prone to this
syndrome. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
For the patient who sits for extended periods of time, their primary cause is
due to contracture of the piriformis muscle. In this case the piriformis muscle
is shortened and does not allow for the smooth movement of the sciatic nerve during
leg motion. A one-time direct trauma to the pelvis is very rarely a cause for
piriformis syndrome due to the protection afforded the pelvis by the overlying
musculature and fat. The causes of myospasm are many. Over use as during excessive
fast walking without proper warm up and stretching (as during exercise), prolonged
sitting, as for your treatment, many variables can hamper your successful recovery.
Smoking, obesity, job and exercise as noted above in prolonged sitting and not
warming up and stretching.
Any treatment plan must include stretching of the gluteal muscles as well as
stretching of the piriformis muscles. Your Chiropractor can help you by instructing
you on the proper exercises and stretches to perform. Many Chiropractors may also
prescribe some form of massage be performed to the piriformis muscle in the gluteal
region in order to relax these muscles.
Your chiropractor may also prescribe certain herbals remedies such as valerian
root and passion flower to help relax the associated muscles during your recovery
phase. Spinal adjustment as well as hip adjustment may also be required to relieve
your symptoms.
--------------------------------------------------------------------------------
Dynamic Chiropractic
June 21, 1991, Volume 09, Issue 13
Printer Friendly Version
Email to a Friend
Alternative Health
Acupuncture
Piriformis Syndrome: Part I Link
--------------------------------------------------------------------------------
The patient with an unrelenting sciatica may be suffering with a piriformis syndrome.
This syndrome is considered an entrapment neuropathy caused by pressure on the sciatic
nerve by an enlarged or inflamed piriformis muscle. The sciatic nerve can be compressed
between the swollen muscle fibers and the bony pelvis.1 Pace and Nagle2 estimated that
45 of 750 cases referred to their back clinic were treated for this syndrome. They
found that the condition was six times more prevalent in women than men. Because this
syndrome is not common it is often overlooked and needless surgery may result. Wyant3
states that the functional test for piriformis syndrome should be a routine part of
the physical examination of all patients presenting with lower spinal backache.
Besides backache, the piriformis muscle contracture and associated adhesions has
been related to radiating pain from the sacrum to the hip joint over the gluteal
region to the posterior thigh, coccydynia,4 dyspareunia, male impotency5, and oblique
axis rotation of the sacrum with its effect on the total spine up to the atlanto-
occipital region.5
According to Gray6 and Freiberg7 the piriformis arises from the anterior sacrum
between the second to fourth anterior sacral foramina, from the margin of the greater
sciatic foramen and from the anterior surface of the sacrotuberous ligament, the
anterior sacrospinous ligament and the capsule of the sacroiliac joint. Freiberg
states that the piriformis is the only muscle that bridges the sacroiliac joint. The
piriformis passes through the greater sciatic foramen (the upper part of which it
fills) and inserts by a rounded tendon into the upper border of the greater trochanter.
Pecian8 examined 130 human specimens to determine the anatomical relations of the
sciatic nerve and the piriformis. He found that in 6.15 percent of the cases the
peroneal part of the sciatic nerve passes between the tendinous parts of the piriformis
and a pinching of the nerve can occur. He found at least five other variations of the
sciatic nerve in relation to the piriformis muscle. He concluded that when the nerve
passed between the tendinous portion of the piriformis the nerve would more likely be
pinched during passive medial rotation of the thigh which stretches the piriformis,
causing the nerve to be pressed against the extended piriformis. In this case, resisted
testing of the piriformis or ordinary active piriformis contraction would separate the
tendinous portion of the piriformis surrounding the sciatic nerve and would not
compress the nerve.
Mizuguche9 felt that before the piriformis could aggravate the sciatic nerve there
first had to be a preexisting tension on the sciatic nerve by scarring or arachnoiditis
around the nerve roots secondary to laminectomy or some space-occupying lesion such as
osteoarthritic spurs. He thought that ordinary walking would cause the piriformis to
impinge the shortened nerve. A history of trauma to the sacroiliac or gluteal region
has also been blamed10.
The straight leg raise may be positive due to a contracted piriformis muscle. In a study
by Freiberg and Vinke11 on 10 cadavers it was found that after raising the leg 25 degrees,
the sacrotuberous ligament becomes taut because of its attachment to the ischial tuberosity
and the hamstrings. A contracted piriformis muscle which originates off the sacrotuberous
ligament also tightened during the SLR.
The functional tests for a piriformis syndrome is naturally based on the function of
the piriformis muscle. One of the main reasons for muscle testing is to determine if
a muscle is painful. Since the piriformis muscle is an external hip rotator when the
hip is in extension and an abductor when the hip is in flexion,9 external hip rotation
should be tested with the patient supine with the legs hanging off the table edge at
the knees. The patient then attempts to push his leg medially against resistance. The
abduction test for the piriformis could be tested with the patient sitting facing the
examiner. The patient attempts to abduct the knee against resistance.2 The patient will
complain of pain and possible weakness due to the pain. There may be pain when the patient
sits or squats due to external rotation of the thigh and hip.5 Passive internal rotation
of the thigh with the patient supine could also aggravate the condition. Pressure on the
piriformis by way of rectal or vaginal examination may reproduce the symptoms.3 A positive
"piriformis sign" due to piriformis contracture may be seen by the persistent external
rotation of one lower extremity when the patient is supine. A contracted piriformis may
result in a functional short leg.5 The symptoms of female pain during coitus (dyspareunia)
could be due to the externally rotated hips, but female pain and male impotency is also
attributed to piriformis compression of the pudendal nerve and blood vessels.5
According to Retzlaff et al.,5 on the side of the piriformis contracture the sacral base
will be rotated anteriorly and examination of a prone patient will show a deepened sulcus
on that side. The apex of the sacrum will appear posterior on the opposite side at the
level of the posterior inferior illiac spine (oblique axis rotation of the sacrum). This
may cause rotoscoliosis of the lumbar spine and increased lumbar lordosis which may
effect the function of the whole spine. Digital pressure over the piriformis may refer
pain along the complaint area.
Part II will discuss a variety of conservative treatments for this syndrome.
Warren Hammer, M.S., D.C., D.A.B.C.O.
Editor's Note:
Dr. Hammer will conduct his next soft tissue seminar.
You may call 1-800-327-2289 to register.
Dr. Hammer's new book, Functional Soft Tissue Examination and Treatment by Manual
Methods: The Extremities, is now available. Please see the Preferred Reading and
Viewing list on page xx, part #T126 to order your copy.
References
Jankiewicz JJ, Hennrikus WL, Houkom JA: "The appearance of the piriformis muscle
syndrome in computed tomography and magnetic resonance imaging: a case report and
review of the literature." Clin Orth & Rel Res:262,205-209.
Pace JB, Nagle D: "Piriformis syndrome." West J Med 24:436, 1976.
Wyant G: "Chronic pain syndromes and their treatment: III. The piriformis syndrome."
Can Anaesth Soc J. 26:305, 1976.
Thiele GH: "Tonic spasm of the levator ani, coccygeus and piriformis muscles."
Trans Am Pract Soc 37:145-155, 1936.
Retzlaff E, Berry AH, Haight AS et al. "The piriformis muscle syndrome."
J AM Osteopath Assoc 73:799-807.
Gray H: Anatomy of the Human Body. 26th ed. Philadelphia: Lea & Febiger, 1956:541.
Freiberg AH: "Sciatic pain and its relief by operations on the muscle and fascia."
Arch Surg 34:337m 1937.
Pecian M: "Contribution to the etiological explanation of the piriformis syndrome."
Acta Anat (Basel) 105:181-186, 1979.
Mizughuchi T: "Division of the piriformis muscle in the treatment of sciatica."
Arch Surg 111:719-722, 1976.
Robinson D: "Piriformis syndrome in relation to sciatic pain." Am J Surg 73:356-358, 1947.
Freiburg AH, Vinke TA: "Sciatica and the sacroiliac join." J Bone Joint Surg 16:126, 1934.
----0
Siatica.org
Diagnosis and Treatment of Piriformis Syndrome Link
Piriformis syndrome is estimated to cause 6-8% of sciatica, but is more common in
the general population because it has been under diagnosed and under treated.
The following outline is intended to present elements of the history and physical
findings that suggest piriformis syndrome, and the electrophysiological technique
for documenting its presence, injection technique and physical therapy. Finally,
there is a section on outcome and alternative treatments and current clinical
research protocols.
Diagnosis
The patient with piriformis syndrome typically complains of sciatic pain, tenderness
in the buttock, and more difficulty sitting than standing. The pain usually arises
from overuse: athletics, heavy work, or prolonged sitting, though traumatic causes
are also reasonably common, including automobile accidents, falls, and penetrating
wounds.
Physical findings include tenderness of the buttock region, increased pain with
adduction, internal rotation and flexion of the affected thigh while the patient
is in the contra lateral decubitus position, weakened abduction of the flexed thigh,
and iliotibial band syndrome.
EMG findings include positive FAIR-test, signs of denervation (acute or chronic) in
the pattern of the posterior tibial or the peroneal nerves, as opposed to a radicular
distribution, reduced CMAPs and/or SNAPs on the affected side, and a positive FAIR-test.
The FAIR-test compares the sum of M-wave plus H-reflex in the anatomical position with
the sum of M-wave plus H-reflex in the Flexed, Adducted, Internally Rotated position.
Piriformis FAIR-test position (Contra lateral Decubitus)
Critical physical exam maneuver for muscle based piriformis syndrome: The patient's
foot is placed lateral to the contra lateral knee. Resisted abduction or adduction
against the examiner's hand may reproduce the symptoms. Straight leg rising is
typically negative. There is often relief obtained by traction on the involved leg,
particularly by pulling upwards at a ten to twenty degree angle and towards the
contra lateral side by a similar amount. The distribution of symptoms typically involves
both L5 (big toe) and S1 (small toe) components because this a pan-sciatic syndrome.
The symptoms often progress no further than the ankle in distinction to sciatica
from a lumbar disk which typically radiates into the toes. Link
---
SEARCH Receive Spine News patient>conditions>other
Piriformis Syndrome Spine Universe ChiropracticLink
Piriformis Syndrome is caused by an entrapment (pinching) of the sciatic nerve
as it exits the Greater Sciatic notch in the gluteal region. There are two normal
variations for the exit of the sciatic nerve in this region. The first places the
sciatic nerve inferior (below) to the Piriformis muscle and superior (above) the
gemellus muscle. Entrapment in this area is likely due to a myospasm or contracture
(tightening or shortening respectively) of either of these two muscles.
The second common site of entrapment is when the sciatic nerve actually pierces
the piriformis muscle itself. This can occur in about 1% to 10% of all humans.
In this case myospasm and or contraction of the piriformis muscle itself can lead
to pain along the back of the thigh to the knee, loss of sensation or numbness
and tingling in the sole of the foot. This particular syndrome can often mimic
its more notorious counterpart known as sciatica, and that being the case, it is
often misdiagnosed as sciatica. The main difference between sciatica and piriformis
syndrome is in the cause. Sciatica is directly due to a lumbar disc pressing on
the sciatic nerve as it exits the intervertebral foramen in the lumbar spine. What
both of these complaints have in common is that both can produce pain, numbness
and tingling below the knee and into the foot.
The main diagnostic tests performed by your doctor of Chiropractic is what
distinguishes one from the other. With piriformis syndrome your chiropractor
will not get positive tests results that indicate lumbar spine involvement.
Often the patient may not be aware that there is a problem. Some cases won't
show up until a complete neurological exam is performed on the lower extremity.
The patient may have chief complaints ranging from no pain to pain in the lower
back to gluteal pain to numbness and tingling in the foot. As can be seen the
symptoms in this condition can vary widely making the doctor who is not used to
differentially diagnosing this condition from sciatica confused as to the cause
of the condition.
Many weekend athletes and people who spend long hours sitting are prone to this
syndrome. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
For the patient who sits for extended periods of time, their primary cause is
due to contracture of the piriformis muscle. In this case the piriformis muscle
is shortened and does not allow for the smooth movement of the sciatic nerve during
leg motion. A one-time direct trauma to the pelvis is very rarely a cause for
piriformis syndrome due to the protection afforded the pelvis by the overlying
musculature and fat. The causes of myospasm are many. Over use as during excessive
fast walking without proper warm up and stretching (as during exercise), prolonged
sitting, as for your treatment, many variables can hamper your successful recovery.
Smoking, obesity, job and exercise as noted above in prolonged sitting and not
warming up and stretching.
Any treatment plan must include stretching of the gluteal muscles as well as
stretching of the piriformis muscles. Your Chiropractor can help you by instructing
you on the proper exercises and stretches to perform. Many Chiropractors may also
prescribe some form of massage be performed to the piriformis muscle in the gluteal
region in order to relax these muscles.
Your chiropractor may also prescribe certain herbals remedies such as valerian
root and passion flower to help relax the associated muscles during your recovery
phase. Spinal adjustment as well as hip adjustment may also be required to relieve
your symptoms.
--------------------------------------------------------------------------------
Dynamic Chiropractic
June 21, 1991, Volume 09, Issue 13
Printer Friendly Version
Email to a Friend
Alternative Health
Acupuncture
Piriformis Syndrome: Part I Link
--------------------------------------------------------------------------------
The patient with an unrelenting sciatica may be suffering with a piriformis syndrome.
This syndrome is considered an entrapment neuropathy caused by pressure on the sciatic
nerve by an enlarged or inflamed piriformis muscle. The sciatic nerve can be compressed
between the swollen muscle fibers and the bony pelvis.1 Pace and Nagle2 estimated that
45 of 750 cases referred to their back clinic were treated for this syndrome. They
found that the condition was six times more prevalent in women than men. Because this
syndrome is not common it is often overlooked and needless surgery may result. Wyant3
states that the functional test for piriformis syndrome should be a routine part of
the physical examination of all patients presenting with lower spinal backache.
Besides backache, the piriformis muscle contracture and associated adhesions has
been related to radiating pain from the sacrum to the hip joint over the gluteal
region to the posterior thigh, coccydynia,4 dyspareunia, male impotency5, and oblique
axis rotation of the sacrum with its effect on the total spine up to the atlanto-
occipital region.5
According to Gray6 and Freiberg7 the piriformis arises from the anterior sacrum
between the second to fourth anterior sacral foramina, from the margin of the greater
sciatic foramen and from the anterior surface of the sacrotuberous ligament, the
anterior sacrospinous ligament and the capsule of the sacroiliac joint. Freiberg
states that the piriformis is the only muscle that bridges the sacroiliac joint. The
piriformis passes through the greater sciatic foramen (the upper part of which it
fills) and inserts by a rounded tendon into the upper border of the greater trochanter.
Pecian8 examined 130 human specimens to determine the anatomical relations of the
sciatic nerve and the piriformis. He found that in 6.15 percent of the cases the
peroneal part of the sciatic nerve passes between the tendinous parts of the piriformis
and a pinching of the nerve can occur. He found at least five other variations of the
sciatic nerve in relation to the piriformis muscle. He concluded that when the nerve
passed between the tendinous portion of the piriformis the nerve would more likely be
pinched during passive medial rotation of the thigh which stretches the piriformis,
causing the nerve to be pressed against the extended piriformis. In this case, resisted
testing of the piriformis or ordinary active piriformis contraction would separate the
tendinous portion of the piriformis surrounding the sciatic nerve and would not
compress the nerve.
Mizuguche9 felt that before the piriformis could aggravate the sciatic nerve there
first had to be a preexisting tension on the sciatic nerve by scarring or arachnoiditis
around the nerve roots secondary to laminectomy or some space-occupying lesion such as
osteoarthritic spurs. He thought that ordinary walking would cause the piriformis to
impinge the shortened nerve. A history of trauma to the sacroiliac or gluteal region
has also been blamed10.
The straight leg raise may be positive due to a contracted piriformis muscle. In a study
by Freiberg and Vinke11 on 10 cadavers it was found that after raising the leg 25 degrees,
the sacrotuberous ligament becomes taut because of its attachment to the ischial tuberosity
and the hamstrings. A contracted piriformis muscle which originates off the sacrotuberous
ligament also tightened during the SLR.
The functional tests for a piriformis syndrome is naturally based on the function of
the piriformis muscle. One of the main reasons for muscle testing is to determine if
a muscle is painful. Since the piriformis muscle is an external hip rotator when the
hip is in extension and an abductor when the hip is in flexion,9 external hip rotation
should be tested with the patient supine with the legs hanging off the table edge at
the knees. The patient then attempts to push his leg medially against resistance. The
abduction test for the piriformis could be tested with the patient sitting facing the
examiner. The patient attempts to abduct the knee against resistance.2 The patient will
complain of pain and possible weakness due to the pain. There may be pain when the patient
sits or squats due to external rotation of the thigh and hip.5 Passive internal rotation
of the thigh with the patient supine could also aggravate the condition. Pressure on the
piriformis by way of rectal or vaginal examination may reproduce the symptoms.3 A positive
"piriformis sign" due to piriformis contracture may be seen by the persistent external
rotation of one lower extremity when the patient is supine. A contracted piriformis may
result in a functional short leg.5 The symptoms of female pain during coitus (dyspareunia)
could be due to the externally rotated hips, but female pain and male impotency is also
attributed to piriformis compression of the pudendal nerve and blood vessels.5
According to Retzlaff et al.,5 on the side of the piriformis contracture the sacral base
will be rotated anteriorly and examination of a prone patient will show a deepened sulcus
on that side. The apex of the sacrum will appear posterior on the opposite side at the
level of the posterior inferior illiac spine (oblique axis rotation of the sacrum). This
may cause rotoscoliosis of the lumbar spine and increased lumbar lordosis which may
effect the function of the whole spine. Digital pressure over the piriformis may refer
pain along the complaint area.
Part II will discuss a variety of conservative treatments for this syndrome.
Warren Hammer, M.S., D.C., D.A.B.C.O.
Editor's Note:
Dr. Hammer will conduct his next soft tissue seminar.
You may call 1-800-327-2289 to register.
Dr. Hammer's new book, Functional Soft Tissue Examination and Treatment by Manual
Methods: The Extremities, is now available. Please see the Preferred Reading and
Viewing list on page xx, part #T126 to order your copy.
References
Jankiewicz JJ, Hennrikus WL, Houkom JA: "The appearance of the piriformis muscle
syndrome in computed tomography and magnetic resonance imaging: a case report and
review of the literature." Clin Orth & Rel Res:262,205-209.
Pace JB, Nagle D: "Piriformis syndrome." West J Med 24:436, 1976.
Wyant G: "Chronic pain syndromes and their treatment: III. The piriformis syndrome."
Can Anaesth Soc J. 26:305, 1976.
Thiele GH: "Tonic spasm of the levator ani, coccygeus and piriformis muscles."
Trans Am Pract Soc 37:145-155, 1936.
Retzlaff E, Berry AH, Haight AS et al. "The piriformis muscle syndrome."
J AM Osteopath Assoc 73:799-807.
Gray H: Anatomy of the Human Body. 26th ed. Philadelphia: Lea & Febiger, 1956:541.
Freiberg AH: "Sciatic pain and its relief by operations on the muscle and fascia."
Arch Surg 34:337m 1937.
Pecian M: "Contribution to the etiological explanation of the piriformis syndrome."
Acta Anat (Basel) 105:181-186, 1979.
Mizughuchi T: "Division of the piriformis muscle in the treatment of sciatica."
Arch Surg 111:719-722, 1976.
Robinson D: "Piriformis syndrome in relation to sciatic pain." Am J Surg 73:356-358, 1947.
Freiburg AH, Vinke TA: "Sciatica and the sacroiliac join." J Bone Joint Surg 16:126, 1934.
----0
Siatica.org
Diagnosis and Treatment of Piriformis Syndrome Link
Piriformis syndrome is estimated to cause 6-8% of sciatica, but is more common in
the general population because it has been under diagnosed and under treated.
The following outline is intended to present elements of the history and physical
findings that suggest piriformis syndrome, and the electrophysiological technique
for documenting its presence, injection technique and physical therapy. Finally,
there is a section on outcome and alternative treatments and current clinical
research protocols.
Diagnosis
The patient with piriformis syndrome typically complains of sciatic pain, tenderness
in the buttock, and more difficulty sitting than standing. The pain usually arises
from overuse: athletics, heavy work, or prolonged sitting, though traumatic causes
are also reasonably common, including automobile accidents, falls, and penetrating
wounds.
Physical findings include tenderness of the buttock region, increased pain with
adduction, internal rotation and flexion of the affected thigh while the patient
is in the contra lateral decubitus position, weakened abduction of the flexed thigh,
and iliotibial band syndrome.
EMG findings include positive FAIR-test, signs of denervation (acute or chronic) in
the pattern of the posterior tibial or the peroneal nerves, as opposed to a radicular
distribution, reduced CMAPs and/or SNAPs on the affected side, and a positive FAIR-test.
The FAIR-test compares the sum of M-wave plus H-reflex in the anatomical position with
the sum of M-wave plus H-reflex in the Flexed, Adducted, Internally Rotated position.
Piriformis FAIR-test position (Contra lateral Decubitus)
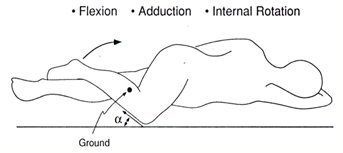 -----
PIRIFORMIS SYNDROME Link
Gabe Mirkin, M.D.
If it hurts to touch a point that's in the middle of one side of your buttocks,
you probably have piriformis syndrome.
This chronic condition is very difficult to diagnose, because other injuries may
produce exactly the same symptoms. Similar pain may be the result of an injury
to bones, muscles, tendons, bursae (pads between the tendons and bones), the hip
joint, or the sciatic nerve, but there are ways to determine from which condition
you might be suffering.
If you feel most pain when you land after hopping on one leg, you might have an
injured hip joint or a stress fracture in your pelvis or upper leg bones. An x-ray
will usually reveal a joint injury, but only a bone scan will reveal a stress
fracture.
If you feel pain in your buttocks, particularly when you touch your toes while
keeping your knees straight, you might have a tear in the large muscles or tendons
that run down the back of your hips.
If you feel pain when you touch a spot that's either on the lowest point of your
pelvis (the part that touches a chair when you sit) or at the top of your femur
(thigh), you might have injured your bursae (bursitis) or torn the tendons that
are attached to bones at these sites.
If your back hurts, particularly when you bend backwards, and the pain goes down
the back of your leg to below your knees, your sciatic nerve is probably being
pinched in your back.
Cause: The sciatic nerve is the longest nerve in your body. It starts on the lower
part of your spine, [passes through a hole between the piriformis muscle above it
and several other muscles beneath it, and goes down the back of your leg to below
the knee. When you run, the piriformis muscle contracts and squeezes the sciatic
nerve underneath it. Repeatedly squeezing and relaxing the piriformis muscle can
damage the sciatic nerve and cause pain. This injury is thought to be caused by
an innate tightness of the piriformis muscle or a structural abnormality in the
path of the sciatic nerve. It can't be attributed to a specific error in training.
Treatment: Piriformis syndrome won't ease until you stop running. Don't run again
until you can run without feeling pain in your buttocks. If it hurts to touch, it
hasn't healed.
In most cases, pedaling a bicycle will also be painful. You probably shouldn't do
any exercise that causes you to bend at the hip while keeping your knees straight,
because this will stretch the sciatic nerve. You might be able to swim, if it isn't
painful. Medication doesn't usually alleviate the pain, and even if it does, the
pain will return as soon as you stop taking it.
Sometimes, the pain will disappear after a rest of a few days to several months;
frequently it does not. In this case your doctor will be able to make an accurate
diagnosis by injecting a mixture of xylocaine and corticosteroid drugs directly
into the piriformis muscle where it passes over the sciatic nerve. If the pain
disappears, you may resume running only after a few weeks, but remember that this
injury tends to recur. If you feel pain in that area, stop running immediately,
and don't attempt to run again until you can do so without pain.
This article recorded 11/15/02
-----
Spinehealth.com
Link
Common causes of back pain
Related information
o Physical therapy
o Piriformis syndrome--another irritation to the sciatic nerve
o What you need to know about sciatica
Overview
Piriformis syndrome:
What is the Piriformis muscle? Link
The Piriformis is one of the small muscles deep in the buttocks that rotates
the leg outwards. It runs from the base of the spine and attaches to the thigh
bone (femur) roughly where the outside crease in your bum is. The sciatic nerve
runs very close to this muscle and sometimes even through it!
What can the athlete do?
Apply heat.
Stretch the Piriformis muscle.
Strengthen the Piriformis muscle.
See a sports injury professional who can advise on treatment, rehabilitation and prevention
What can a sports injury professional do?
Apply specific sports massage techniques.
Stretch the Piriformis muscle using Muscle Energy Techniques.
Apply ultrasound.
Advise on strengthening and rehabilitation to avoid injury recurrence.
If these stretches don't help it is possible that you will need Piriformis Release Surgery.
===================================================================================
Piriformis Syndrome (Sciatic Pain) - learn how you can reduce your sciatic
pain and piriformis syndrome. ... Piriformis Syndrome (Sciatic Pain) in the following
link:
Read about the four causes that cause Piriformis Syndrome: Link
===================================================================================
The piriformis muscle and the sciatic nerve
The piriformis muscle is a small muscle located in the buttocks that rotates the
hip. It runs horizontally, and the sciatic nerve runs vertically directly beneath
the muscle. The muscle can become tight and place pressure on the sciatic nerve,
resulting in leg pain which may be difficult to distinguish from a radiculopathy
(nerve pinching in the spine), which is also commonly called sciatica.
The patient's spinal imaging studies will not show any nerve pinching, and on
physical exam, motion of the patient's hip will generate the pain.
Conservative care for piriformis syndrome
Treatment for piriformis syndrome typically consists of:
Physical therapy that includes manual release (deep massage), along with hip
range of motion exercises can help piriformis syndrome.
For severe cases of piriformis syndrome, the muscle may be injected with lidocaine
to decrease spasm and help the patient make progress in physical therapy.
By: Peter F. Ullrich, Jr., MD
September 8, 1999
Updated February 28, 2001
=============================================================================
Receive Spine News
Piriformis Syndrome Link
Timothy J. Maggs, M.D.
If you've ever felt pain in the hip, pain in the center of the butt or pain
down the back of the leg, you are likely suffering, at least partially, with
piriformis syndrome. The piriformis is a muscle which runs from your sacrum
(mid-line base of spine) to the outer hip bone (trochanter). This muscle truly
works overtime on anyone who runs at all.
The muscles in and around the gluteal region help with three areas
1.rotation of the hip and leg;
2.balance while one foot is off the ground; and
3.stability for the pelvic region.
Needless to say, all of these characteristics are highly needed by runners.
Conclusion--the piriformis muscle is pretty important for all of us.
Injuries to the Piriformis
This muscle is a prime candidate for repetitive motion injury (RMI). RMI occurs
when a muscle is asked to perform beyond it's level of capability, not given
enough time to recover, and asked to perform again. The typical response from
a muscle in this situation is to tighten, which is a defensive response of the
muscle. This tightness, however, manifests itself in several ways to a runner.
The first symptom suggesting piriformis syndrome would be pain in and around the
outer hip bone. The tightness of the muscle produces increased tension between
the tendon and the bone which produces either direct discomfort and pain or an
increased tension in the joint producing a bursitis. Again, a bursitis is an
inflammation of the fluid filled sac in a joint caused by an elevation of stress
and tension within that joint.
The second symptom suggesting piriformis syndrome would be pain directly in the
center of the buttocks. Although this is not as common as the other two symptoms,
this pain can be elicited with direct compression over the belly of the buttocks
area. A tight muscle is a sore muscle upon compression due to a reduced blood
flow to that muscle.
The third symptom suggesting piriformis syndrome would be a sciatic neuralgia,
or pain from the buttocks down the back of the leg and sometimes into different
portions of the lower leg. The sciatic nerve runs right through the belly of the
piriformis muscle and if the piriformis muscle contracts from being overused, the
sciatic nerve now becomes strangled, producing pain, tingling and numbness.
Simple Physiology
Any muscle repetitively used needs to have an opportunity to recover. This recover
can either be on Nature's clock, or can be facilitated and sped up with proper
knowledge and treatment. Since the muscle is tightening due to overuse, continued
use will only make it worse. This injured muscle needs to relax and have increased
blood flow encouraged to it for more rapid healing. This tightness that exists
also reduces the normal blood flow going to the muscle reducing the speed with
which the muscle can recover. To encourage fresh, oxygen-rich blood to the muscle
is the most powerful means of getting the muscle to begin to relax and function
normally. Multiple massages per day to this area are greatly encouraged.
The next step in this "recovery" process is to use a tennis ball under the butt
and hip area. While sitting down on the floor, roll away from the side of involvement
and place a tennis ball just inside the outer hip bone under the butt area. As you
begin to allow your weight onto the tennis ball, note areas of increased pain and
soreness. Trigger points will tend to accumulate in a repetitively used muscle,
and until these toxins are manually broken up and eliminated, the muscle will have
an artificial ceiling with regard to flexibility potential and recovery potential
So, if it's sore and hurts while you're sitting on it, you're doing a good job. Let
the ball work under each spot for 15-20 seconds before moving it to another area.
Once you've been on the ball for 4-5 minutes, now put the ankle of the involved
leg over the knee of the non-involved leg (crossing your legs). Now place the
tennis ball just inside the outer hip bone again and work the tendon of the piriformis
muscle. While this pain is typically excruciating and takes some time to effectively
reduce, the benefits here are huge. Be patient, be consistent and good things
will happen.
Additional Treatments
Due to the fact that the sciatic neuralgia and the hip bursitis or tendonitis are
both inflammatory in nature, ice, or cryotherapy, over the involved area 15-20
minutes at a time will be beneficial. This should be done multiple times per day.
Stretching of the hip muscles should not be done until the acute pain is gone. At
that point in time, begin with gentle stretching, such as the cross-legged stretch
while pulling up on the knee. The muscle should have increased flexibility before
an active return to running.
Finally, I'm always discouraging the use of pharmaceutical anti-inflammatories.
Not only do they greatly aggravate the intestines, but they also suggest an artificial
wellness that can lead to bigger problems. Proteolytic enzymes, such as bromelain,
are both natural and extremely beneficial with no side effects. For more information,
visit your health food store or check out Rehab Plus on our website.
=============================================================================
All About Piriformis Syndrome & Approach to Treatment Link
Sponsored by: Relief-Mart - Quality health products for the back and spine.
Piriformis Syndrome is a term for a condition in which the sciatic nerve becomes
pinched in the region of the buttocks. This pinching can cause symptoms which
include numbness, tingling, burning and achy soreness along the sciatic nerve
path, a nerve which extends from the buttock area down the back of the leg to
the foot. The sciatic nerve runs through a muscle in the buttocks region called
the Piriformis. When the muscle shortens or spasms due to trauma, it can compress
the sciatic nerve. This cause of sciatica symptoms is known as Piriformis Syndrome.
The Piriformis muscle can be shortened and irritated from overuse of the muscle
with repetitive movements like aerobics and dancing. The approach to treating
Piriformis Syndrome is to reduce the compressive forces that are causing the pressure
on the nerve. This can be accomplished through manual muscle stretching, massage,
mobilization and pelvic adjustive techniques to take pressure of the Sacroiliac
joints, and stretches to increase the length and loosen up the Piriformis muscle.
At the onset of the irritation goals will be to lessen the pain and help to minimize
any inflammation. The listed Therapies, Products and Activities section will give
more information on how to help your condition, however, as each Piriformis Syndrome
condition is different, always consult your doctor to determine what treatment
is right for your particular situation.
What if you have burning pains as your main symptoms:
--------
Medications
One of the most frequent questions our health experts encounter is whether medication
should be taken, and which one would be right for them. It is important to remember
those medications are aimed at temporarily reducing pain, inflammation, and relaxing
the body, but have not been proven to increase healing to the area. Here are some
of the most commonly mentioned medications:
For over-the-counter medication, Ibuprofen has been indicated for temporary pain
relief. Studies have also shown that in higher amounts, Ibuprofen can act as an
anti-inflammatory, but a medical doctor's prescription is needed for this dosage.
Aspirin and acetaminophen are also indicated for muscle pain relief, but do not
show anti-inflammatory properties in prescription dosages. Acetaminophen does not
have warnings about adverse reactions for people with aspirin allergies, as it is
not an aspirin derivative. It has also been demonstrated to be better tolerated
by people with weak intestinal systems. While Aspirin is known to be more abrasive
on the intestinal system, it may have other side benefits such as blood thinning
that prevents the blood clots which can lead to strokes and myocardial infarctions
As these medications work to block pain and inflammation temporarily, it stands to
reason that the need for these medications can occur when a person can no longer
function due to the pain or when it hinders sleep and thereby impedes the bodies
natural healing process. A person on pain medication should consider that they may
more easily overdo it during the temporary relief period, which could cause further
injury to the muscles.
*As side effects can occur, always consult your medical doctor to determine if and
what medication is appropriate for your situation.*
Exercises and Stretches for the Back
Muscular stretching can be a very important part of the healing process for tightened
muscles of the back. It is essential to lengthen any shortened muscular tissue of
the back to help prevent further pulling on the already shortened fibers. Muscular
strengthening exercises will be important once the back irritation has subsided.
Back strengthening exercises help to build stability to weak tissue. It should be
noted that irritated muscles can become further damaged with strengthening exercises
that are premature to the healing of the area. The exercises below are general
exercises to increase flexibility and can help to stabilize the back. However, it
should be noted that for most of these exercises, you should not feel the stretch
in the back itself. For example, the back of the legs have a group of muscles called
the hamstrings. These muscles originate in the lower pelvis and insert into the leg.
When the hamstrings are tight, the back itself can be tightened due to the pulling
on the pelvis. Therefore, stretching the hamstrings will not only loosen the leg
muscles up but they will take the strain off the back.
Warning:
exercises should never be performed if they cause irritation
to your back or any other condition while they are being performed! As each
Piriformis Syndrome condition is different, always consult your doctor before
performing any of these exercises to determine what exercises, if any, are right
for your particular condition. If you have any discomfort after performing any
of these exercises, discontinue and immediately and consult a doctor to properly
assess your situation.*
STRETCHES:
Gluteus Stretch
-----
PIRIFORMIS SYNDROME Link
Gabe Mirkin, M.D.
If it hurts to touch a point that's in the middle of one side of your buttocks,
you probably have piriformis syndrome.
This chronic condition is very difficult to diagnose, because other injuries may
produce exactly the same symptoms. Similar pain may be the result of an injury
to bones, muscles, tendons, bursae (pads between the tendons and bones), the hip
joint, or the sciatic nerve, but there are ways to determine from which condition
you might be suffering.
If you feel most pain when you land after hopping on one leg, you might have an
injured hip joint or a stress fracture in your pelvis or upper leg bones. An x-ray
will usually reveal a joint injury, but only a bone scan will reveal a stress
fracture.
If you feel pain in your buttocks, particularly when you touch your toes while
keeping your knees straight, you might have a tear in the large muscles or tendons
that run down the back of your hips.
If you feel pain when you touch a spot that's either on the lowest point of your
pelvis (the part that touches a chair when you sit) or at the top of your femur
(thigh), you might have injured your bursae (bursitis) or torn the tendons that
are attached to bones at these sites.
If your back hurts, particularly when you bend backwards, and the pain goes down
the back of your leg to below your knees, your sciatic nerve is probably being
pinched in your back.
Cause: The sciatic nerve is the longest nerve in your body. It starts on the lower
part of your spine, [passes through a hole between the piriformis muscle above it
and several other muscles beneath it, and goes down the back of your leg to below
the knee. When you run, the piriformis muscle contracts and squeezes the sciatic
nerve underneath it. Repeatedly squeezing and relaxing the piriformis muscle can
damage the sciatic nerve and cause pain. This injury is thought to be caused by
an innate tightness of the piriformis muscle or a structural abnormality in the
path of the sciatic nerve. It can't be attributed to a specific error in training.
Treatment: Piriformis syndrome won't ease until you stop running. Don't run again
until you can run without feeling pain in your buttocks. If it hurts to touch, it
hasn't healed.
In most cases, pedaling a bicycle will also be painful. You probably shouldn't do
any exercise that causes you to bend at the hip while keeping your knees straight,
because this will stretch the sciatic nerve. You might be able to swim, if it isn't
painful. Medication doesn't usually alleviate the pain, and even if it does, the
pain will return as soon as you stop taking it.
Sometimes, the pain will disappear after a rest of a few days to several months;
frequently it does not. In this case your doctor will be able to make an accurate
diagnosis by injecting a mixture of xylocaine and corticosteroid drugs directly
into the piriformis muscle where it passes over the sciatic nerve. If the pain
disappears, you may resume running only after a few weeks, but remember that this
injury tends to recur. If you feel pain in that area, stop running immediately,
and don't attempt to run again until you can do so without pain.
This article recorded 11/15/02
-----
Spinehealth.com
Link
Common causes of back pain
Related information
o Physical therapy
o Piriformis syndrome--another irritation to the sciatic nerve
o What you need to know about sciatica
Overview
Piriformis syndrome:
What is the Piriformis muscle? Link
The Piriformis is one of the small muscles deep in the buttocks that rotates
the leg outwards. It runs from the base of the spine and attaches to the thigh
bone (femur) roughly where the outside crease in your bum is. The sciatic nerve
runs very close to this muscle and sometimes even through it!
What can the athlete do?
Apply heat.
Stretch the Piriformis muscle.
Strengthen the Piriformis muscle.
See a sports injury professional who can advise on treatment, rehabilitation and prevention
What can a sports injury professional do?
Apply specific sports massage techniques.
Stretch the Piriformis muscle using Muscle Energy Techniques.
Apply ultrasound.
Advise on strengthening and rehabilitation to avoid injury recurrence.
If these stretches don't help it is possible that you will need Piriformis Release Surgery.
===================================================================================
Piriformis Syndrome (Sciatic Pain) - learn how you can reduce your sciatic
pain and piriformis syndrome. ... Piriformis Syndrome (Sciatic Pain) in the following
link:
Read about the four causes that cause Piriformis Syndrome: Link
===================================================================================
The piriformis muscle and the sciatic nerve
The piriformis muscle is a small muscle located in the buttocks that rotates the
hip. It runs horizontally, and the sciatic nerve runs vertically directly beneath
the muscle. The muscle can become tight and place pressure on the sciatic nerve,
resulting in leg pain which may be difficult to distinguish from a radiculopathy
(nerve pinching in the spine), which is also commonly called sciatica.
The patient's spinal imaging studies will not show any nerve pinching, and on
physical exam, motion of the patient's hip will generate the pain.
Conservative care for piriformis syndrome
Treatment for piriformis syndrome typically consists of:
Physical therapy that includes manual release (deep massage), along with hip
range of motion exercises can help piriformis syndrome.
For severe cases of piriformis syndrome, the muscle may be injected with lidocaine
to decrease spasm and help the patient make progress in physical therapy.
By: Peter F. Ullrich, Jr., MD
September 8, 1999
Updated February 28, 2001
=============================================================================
Receive Spine News
Piriformis Syndrome Link
Timothy J. Maggs, M.D.
If you've ever felt pain in the hip, pain in the center of the butt or pain
down the back of the leg, you are likely suffering, at least partially, with
piriformis syndrome. The piriformis is a muscle which runs from your sacrum
(mid-line base of spine) to the outer hip bone (trochanter). This muscle truly
works overtime on anyone who runs at all.
The muscles in and around the gluteal region help with three areas
1.rotation of the hip and leg;
2.balance while one foot is off the ground; and
3.stability for the pelvic region.
Needless to say, all of these characteristics are highly needed by runners.
Conclusion--the piriformis muscle is pretty important for all of us.
Injuries to the Piriformis
This muscle is a prime candidate for repetitive motion injury (RMI). RMI occurs
when a muscle is asked to perform beyond it's level of capability, not given
enough time to recover, and asked to perform again. The typical response from
a muscle in this situation is to tighten, which is a defensive response of the
muscle. This tightness, however, manifests itself in several ways to a runner.
The first symptom suggesting piriformis syndrome would be pain in and around the
outer hip bone. The tightness of the muscle produces increased tension between
the tendon and the bone which produces either direct discomfort and pain or an
increased tension in the joint producing a bursitis. Again, a bursitis is an
inflammation of the fluid filled sac in a joint caused by an elevation of stress
and tension within that joint.
The second symptom suggesting piriformis syndrome would be pain directly in the
center of the buttocks. Although this is not as common as the other two symptoms,
this pain can be elicited with direct compression over the belly of the buttocks
area. A tight muscle is a sore muscle upon compression due to a reduced blood
flow to that muscle.
The third symptom suggesting piriformis syndrome would be a sciatic neuralgia,
or pain from the buttocks down the back of the leg and sometimes into different
portions of the lower leg. The sciatic nerve runs right through the belly of the
piriformis muscle and if the piriformis muscle contracts from being overused, the
sciatic nerve now becomes strangled, producing pain, tingling and numbness.
Simple Physiology
Any muscle repetitively used needs to have an opportunity to recover. This recover
can either be on Nature's clock, or can be facilitated and sped up with proper
knowledge and treatment. Since the muscle is tightening due to overuse, continued
use will only make it worse. This injured muscle needs to relax and have increased
blood flow encouraged to it for more rapid healing. This tightness that exists
also reduces the normal blood flow going to the muscle reducing the speed with
which the muscle can recover. To encourage fresh, oxygen-rich blood to the muscle
is the most powerful means of getting the muscle to begin to relax and function
normally. Multiple massages per day to this area are greatly encouraged.
The next step in this "recovery" process is to use a tennis ball under the butt
and hip area. While sitting down on the floor, roll away from the side of involvement
and place a tennis ball just inside the outer hip bone under the butt area. As you
begin to allow your weight onto the tennis ball, note areas of increased pain and
soreness. Trigger points will tend to accumulate in a repetitively used muscle,
and until these toxins are manually broken up and eliminated, the muscle will have
an artificial ceiling with regard to flexibility potential and recovery potential
So, if it's sore and hurts while you're sitting on it, you're doing a good job. Let
the ball work under each spot for 15-20 seconds before moving it to another area.
Once you've been on the ball for 4-5 minutes, now put the ankle of the involved
leg over the knee of the non-involved leg (crossing your legs). Now place the
tennis ball just inside the outer hip bone again and work the tendon of the piriformis
muscle. While this pain is typically excruciating and takes some time to effectively
reduce, the benefits here are huge. Be patient, be consistent and good things
will happen.
Additional Treatments
Due to the fact that the sciatic neuralgia and the hip bursitis or tendonitis are
both inflammatory in nature, ice, or cryotherapy, over the involved area 15-20
minutes at a time will be beneficial. This should be done multiple times per day.
Stretching of the hip muscles should not be done until the acute pain is gone. At
that point in time, begin with gentle stretching, such as the cross-legged stretch
while pulling up on the knee. The muscle should have increased flexibility before
an active return to running.
Finally, I'm always discouraging the use of pharmaceutical anti-inflammatories.
Not only do they greatly aggravate the intestines, but they also suggest an artificial
wellness that can lead to bigger problems. Proteolytic enzymes, such as bromelain,
are both natural and extremely beneficial with no side effects. For more information,
visit your health food store or check out Rehab Plus on our website.
=============================================================================
All About Piriformis Syndrome & Approach to Treatment Link
Sponsored by: Relief-Mart - Quality health products for the back and spine.
Piriformis Syndrome is a term for a condition in which the sciatic nerve becomes
pinched in the region of the buttocks. This pinching can cause symptoms which
include numbness, tingling, burning and achy soreness along the sciatic nerve
path, a nerve which extends from the buttock area down the back of the leg to
the foot. The sciatic nerve runs through a muscle in the buttocks region called
the Piriformis. When the muscle shortens or spasms due to trauma, it can compress
the sciatic nerve. This cause of sciatica symptoms is known as Piriformis Syndrome.
The Piriformis muscle can be shortened and irritated from overuse of the muscle
with repetitive movements like aerobics and dancing. The approach to treating
Piriformis Syndrome is to reduce the compressive forces that are causing the pressure
on the nerve. This can be accomplished through manual muscle stretching, massage,
mobilization and pelvic adjustive techniques to take pressure of the Sacroiliac
joints, and stretches to increase the length and loosen up the Piriformis muscle.
At the onset of the irritation goals will be to lessen the pain and help to minimize
any inflammation. The listed Therapies, Products and Activities section will give
more information on how to help your condition, however, as each Piriformis Syndrome
condition is different, always consult your doctor to determine what treatment
is right for your particular situation.
What if you have burning pains as your main symptoms:
--------
Medications
One of the most frequent questions our health experts encounter is whether medication
should be taken, and which one would be right for them. It is important to remember
those medications are aimed at temporarily reducing pain, inflammation, and relaxing
the body, but have not been proven to increase healing to the area. Here are some
of the most commonly mentioned medications:
For over-the-counter medication, Ibuprofen has been indicated for temporary pain
relief. Studies have also shown that in higher amounts, Ibuprofen can act as an
anti-inflammatory, but a medical doctor's prescription is needed for this dosage.
Aspirin and acetaminophen are also indicated for muscle pain relief, but do not
show anti-inflammatory properties in prescription dosages. Acetaminophen does not
have warnings about adverse reactions for people with aspirin allergies, as it is
not an aspirin derivative. It has also been demonstrated to be better tolerated
by people with weak intestinal systems. While Aspirin is known to be more abrasive
on the intestinal system, it may have other side benefits such as blood thinning
that prevents the blood clots which can lead to strokes and myocardial infarctions
As these medications work to block pain and inflammation temporarily, it stands to
reason that the need for these medications can occur when a person can no longer
function due to the pain or when it hinders sleep and thereby impedes the bodies
natural healing process. A person on pain medication should consider that they may
more easily overdo it during the temporary relief period, which could cause further
injury to the muscles.
*As side effects can occur, always consult your medical doctor to determine if and
what medication is appropriate for your situation.*
Exercises and Stretches for the Back
Muscular stretching can be a very important part of the healing process for tightened
muscles of the back. It is essential to lengthen any shortened muscular tissue of
the back to help prevent further pulling on the already shortened fibers. Muscular
strengthening exercises will be important once the back irritation has subsided.
Back strengthening exercises help to build stability to weak tissue. It should be
noted that irritated muscles can become further damaged with strengthening exercises
that are premature to the healing of the area. The exercises below are general
exercises to increase flexibility and can help to stabilize the back. However, it
should be noted that for most of these exercises, you should not feel the stretch
in the back itself. For example, the back of the legs have a group of muscles called
the hamstrings. These muscles originate in the lower pelvis and insert into the leg.
When the hamstrings are tight, the back itself can be tightened due to the pulling
on the pelvis. Therefore, stretching the hamstrings will not only loosen the leg
muscles up but they will take the strain off the back.
Warning:
exercises should never be performed if they cause irritation
to your back or any other condition while they are being performed! As each
Piriformis Syndrome condition is different, always consult your doctor before
performing any of these exercises to determine what exercises, if any, are right
for your particular condition. If you have any discomfort after performing any
of these exercises, discontinue and immediately and consult a doctor to properly
assess your situation.*
STRETCHES:
Gluteus Stretch
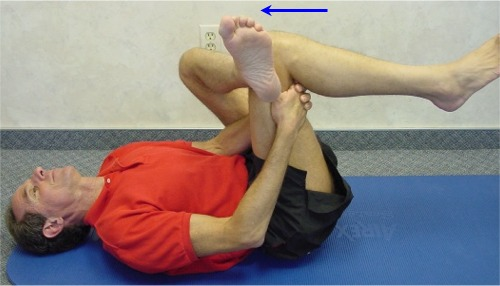 Piriformis Gluteus Stretch
Laying down on your back, bend your right knee, and place your left leg over the
right leg, resting the outside of the left ankle slightly above the right knee.
Place your right hand around the outside of your right thigh and place the left
hand around the inside of your right thigh. Lock the two hands together. Now pull
forward towards your chest to achieve a stretch in the left gluteus portion of you
buttocks. Do the exact opposite to achieve a stretch of the right gluteus portion
of the buttocks. Hold each stretch for a minimum of 30 seconds, any less than 15
seconds and the muscle will not conform to the new increase in length. Do 3 reps,
3-6 times a day. Any pain you feel with this exercise should only be a local
stretching sensation to the back of your thigh and buttocks area, without aggravating
your condition.
Piriformis Stretch
Piriformis Gluteus Stretch
Laying down on your back, bend your right knee, and place your left leg over the
right leg, resting the outside of the left ankle slightly above the right knee.
Place your right hand around the outside of your right thigh and place the left
hand around the inside of your right thigh. Lock the two hands together. Now pull
forward towards your chest to achieve a stretch in the left gluteus portion of you
buttocks. Do the exact opposite to achieve a stretch of the right gluteus portion
of the buttocks. Hold each stretch for a minimum of 30 seconds, any less than 15
seconds and the muscle will not conform to the new increase in length. Do 3 reps,
3-6 times a day. Any pain you feel with this exercise should only be a local
stretching sensation to the back of your thigh and buttocks area, without aggravating
your condition.
Piriformis Stretch
 Piriformis Stretch
Laying down on your back, bend your right leg and pull up your right knee towards
your opposite chest with your left hand. You should feel the stretch in the Piriformis
portion of the right buttocks. Do the exact opposite to achieve a stretch of the left
Piriformis portion of the buttocks. Hold each stretch for a minimum of 30 seconds,
any less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the back of your thigh and buttocks area, without
aggravating your condition.
TFL Stretch
Piriformis Stretch
Laying down on your back, bend your right leg and pull up your right knee towards
your opposite chest with your left hand. You should feel the stretch in the Piriformis
portion of the right buttocks. Do the exact opposite to achieve a stretch of the left
Piriformis portion of the buttocks. Hold each stretch for a minimum of 30 seconds,
any less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the back of your thigh and buttocks area, without
aggravating your condition.
TFL Stretch
 TFL Stretch
Start with stretching the TFL portion of the left hip and outside thigh. While
standing, hold your left hand securely on a solid surface to support your body
as you place your left leg past your right until you reach a maximum stretch.
Follow this with tilting your upper back to the right side while simultaneously
pushing the left side of the hip. Do the exact opposite to achieve a stretch of
the right TFL portion of the hip and outside thigh. Hold each stretch for a
minimum of 30 seconds, any less than 15 seconds and the muscle will not conform
to the new increase in length. Do 3 reps, 3-6 times a day. Any pain you feel
with this exercise should only be a local stretching sensation to the TFL portion
of the hip and outside thigh, without aggravating your condition.
Calf Stretch
TFL Stretch
Start with stretching the TFL portion of the left hip and outside thigh. While
standing, hold your left hand securely on a solid surface to support your body
as you place your left leg past your right until you reach a maximum stretch.
Follow this with tilting your upper back to the right side while simultaneously
pushing the left side of the hip. Do the exact opposite to achieve a stretch of
the right TFL portion of the hip and outside thigh. Hold each stretch for a
minimum of 30 seconds, any less than 15 seconds and the muscle will not conform
to the new increase in length. Do 3 reps, 3-6 times a day. Any pain you feel
with this exercise should only be a local stretching sensation to the TFL portion
of the hip and outside thigh, without aggravating your condition.
Calf Stretch
 Calf Stretch
Start with stretching the right Gastrocnemius portion of the right calf area.
While standing, place your right leg in front of you and your left foot directly
behind you. Place the toes of your right forefoot up against a door or other flat
wall surface, keeping your heel down to the floor. Lean your upper body forward
to place a stretch on the back of the calf. Do the exact opposite to achieve a
stretch of the left calf area. Hold each stretch for a minimum of 30 seconds. Any
less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the calf area of the leg, without aggravating your
condition.
Psoas Stretch
Calf Stretch
Start with stretching the right Gastrocnemius portion of the right calf area.
While standing, place your right leg in front of you and your left foot directly
behind you. Place the toes of your right forefoot up against a door or other flat
wall surface, keeping your heel down to the floor. Lean your upper body forward
to place a stretch on the back of the calf. Do the exact opposite to achieve a
stretch of the left calf area. Hold each stretch for a minimum of 30 seconds. Any
less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the calf area of the leg, without aggravating your
condition.
Psoas Stretch
 Psoas Stretch
Start with stretching the right Psoas muscle. While standing, place your right leg
in front of you and your left foot directly behind you as far as you can comfortably
stretch it. Shift your lower body forward, while simultaneously pushing your upper
body backwards with your arms. Do the exact opposite to achieve a stretch of the
right Psoas portion of your front upper thigh area. Hold each stretch for a minimum
of 30 seconds. Any less than 15 seconds and the muscle will not conform to the new
increase in length. Do 3 reps, 3-6 times a day. Any pain you feel with this exercise
should only be a local stretching sensation to the Psoas area of the upper thigh,
without aggravating your condition.
Quadriceps Stretch
Psoas Stretch
Start with stretching the right Psoas muscle. While standing, place your right leg
in front of you and your left foot directly behind you as far as you can comfortably
stretch it. Shift your lower body forward, while simultaneously pushing your upper
body backwards with your arms. Do the exact opposite to achieve a stretch of the
right Psoas portion of your front upper thigh area. Hold each stretch for a minimum
of 30 seconds. Any less than 15 seconds and the muscle will not conform to the new
increase in length. Do 3 reps, 3-6 times a day. Any pain you feel with this exercise
should only be a local stretching sensation to the Psoas area of the upper thigh,
without aggravating your condition.
Quadriceps Stretch
 Quadriceps Stretch
Yoga and Meditation to Relax the Back
Regardless of the current situation your back is in, relaxing could be key to helping
it heal. While meditation can always be useful for achieving this, Yoga can at times
be irritating if caution is not taken. Yoga is a series of slow movements combined
with stretches and meditation to allow for an increase in flexibility and relaxation
to the muscles and joints, as well as to help optimally integrate the connection
between the mind and body. However, what might seem to be easy maneuvers should
still be treated cautiously, as your individual situation may prohibit certain Yoga
moves. One simple meditation practice that is usually met with good success is to
close your eyes and visualize yourself in the most happy and relaxing place you know
of. Sometimes just taking the time to do this can be what you need to begin the
healing process.
Medical Practitioners Link
A doctor of medicine can take the time to evaluate your condition and confirm
your specific diagnosis. Medical doctors prescribe either over the counter or
prescription only medication. They can prescribe medications that temporarily
relieve inflammation, temporarily relax muscles, and temporarily relieve pain.
Many medical doctors work with physical therapists and chiropractors to provide
conservative management for the many back pain conditions a patient can experience.
Orthopedic doctors have extended training in joint-related conditions such as this.
While Orthopedic doctors can perform back surgery, this drastic step should only be
used when all other treatment options have been exhausted, as back surgery carries
many risks, and not usually recommended for most conditions.
=============================================================================
Running Online Link
Piriformis Syndrome (aka. Pain in the Butt)
============================================================================
Piriformis Syndrome: Link
What is it?
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the
the path of the sciatic nerve. The nerve pain, called "sciatica", often goes
down the back of the thigh and/or into the lower back. The pains is deep in
the buttocks, which is made worse by sitting, climbing stairs or performing
squats. The affected leg is often externally rotated (toes point out) when
relaxed, such as when lying face down on the bed with your feet over the end
of the mattress. Some reports suggest a 6:1 female to male predominance.
The piriformis muscle assists in abducting the and laterally rotating the thigh.
It lies deep in the gluteal muscles and originates from he sacral spine and
attaches to the greater trochanter of the femur. The sciatic nerve usually
passes underneath the piriformis muscle, but in approximately 10% of the
population, travels through the muscle. It is thought that acute or chronic
injury causes swelling of the muscle and irritates the sciatic nerve, resulting
in sciatica. Patients with an aberrant course of the nerve through the muscle
are particularly predisposed to this condition.
=============================================================================
Other causes of Piriformis Syndrome when surgery fails: Link
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain
What is referred pain?
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain
Muscles and Trigger Points:
Many times your pain is actually coming from muscles and the surrounding
connective tissue (fascia).
Situation: when the muscle becomes tight or shortened and is no longer able
to relax to its full resting length a piriformis syndrome problem exists.
When muscle fibers become chronically shortened, the result is a tender nodule
in the muscle, usually in the middle of the muscle or at its attachments.
These tender areas or Trigger Points (TrPs) are named for their astonishing ability
to "trigger" or refer pain to distant areas, far from the actual origin.
=============================================================================
Referred Pain Link
According to Doctors Janet Travell and David Simons in their widely acclaimed
medical textbook, Myofascial Pain and Dysfunction: The Trigger Point Manual,
referred pain is the defining symptom of a myofascial trigger point. It is felt
most often as an oppressive deep ache, this ache can trigger a sciatica symptom
down your effected leg giving you pain both in the buttock and also throughout
the sciatic nerve as it continues down your leg with referred pain.
Some common examples of referred pain are headaches, sinus pain, and the kind
of pain in the neck that won't let you turn your head. Jaw pain, earache, and
sore throat can also be expressions of referred pain. Another is the incapacitating
pain in the side that comes from running too hard and or not used to that
particular exercise and have overdone.
Sore feet and sprained ankles are other examples of referred pain.
Stiffness and pain in a joint should always make you think first of possible trigger
points in nearby muscles that have been subjected to strain or overwork. Pain in
such joints as the knuckles, wrists, elbows, shoulders, knees, and hips are almost
always nothing more serious trigger points which are knotts that need to be
massaged in order to give your muscles relief and full flexibility.
With certain muscles, the referred pain can often be found by pressing on a
trigger point knot that is bad enough to reproduce part of its referred
pain signals. This referred pain is caused by having disruption along the
nerve impulse sciatic nerve line.
Pain referral is difficult because the mechanisms of the human nervous
system is very small and hard to see or operate on. Tiny electrochemical
impulses can be detected and measured to some extent, but not with great
accuracy do to it being so small in size.
Referred pain is happens when your neurological wiring signals get confused.
Inputs from several sources are known to converge into single neurons (nerve cells)
at the spine and are modified before being transmitted to the brain.
One electrical signal can influence another, resulting in some big problems
if the original signal is mixed up from a pinched or decompressed sciatic nerve.
The displacement of pain seems occurs in very predictable patterns with only
small variations from person to person. The predictability shows that there may
be a functional advantage to the referral of pain which helps the sufferer.
Referred pain usually occurs very often in or near a joint, telling you to
modify your exercising and to slow down so that the condition will not
be aggravated to any larger of an extent.
After you've figured out why you have referred pain you can figure out where
it is coming from and then diagnosis and treatment becomes easier for you.
remarkably easy.
In The Trigger Point Therapy Workbook, nationally certified massage therapist
Clair Davies www.triggerpointbook.com has simplified Travell and Simons'
extensive research into referred pain and made it accessible to the non
professional person in the Clair Davies self-applied trigger point massage
book which will hopefully relieve some of the referred pain, numbness,
bad sensations caused by trigger points (which are the root to the cause of the
pain.)
The Trigger Point Therapy Workbook Link
by David G. Simons, M.D.
Clair Davies www.triggerpointbook.com possesses a good combination of
attributes for the common person: He is a skilled at his profession, has good
writing skills that everyone can understand and he shows a great determination to
help everyone get over their suffering from pain.
The Muscle is an orphan organ.
Nobody really studies all the aspects of the muscle and why it gets tied up
in knots and why the referred pain is so hard to figure out the origins of
the original tied up or compressed nerve or muscle. Usually both are involved.
His book shows how to recognize and treat myofascial trigger points.
Massage therapists do study trigger points although rarely trained medically,
are trained in how to find myofascial trigger points through diagnosis and
findings in their skilled treatment of that body part.
There is no well-recognized right way to get the job done which makes it
very hard to get the scientific research and funding in order to model a
clear cut study on diagnosis and treatment.
Myofascial trigger points are a neglected subject.
Virtually all fibromyalgia patients have myofascial trigger points that are
to their total pain and lack of recovery.
There main problem is that they have many more treatable multiple trigger points.
Inactivation of the trigger points of fibromyalgia patients requires especially
delicate and skilled treatment and will take months to completely heal.
Myofascial trigger points as the most common cause of musculoskeletal pain,
but finding someone who understands these trigger points will be very difficult
as best.
The guidance in the trigger point book is a good manual for finding out and
understanding the trigger points and the musculoskeletal pain one has in
which regular doctors were not able to find or diagnose properly.
Doctors treat the pain and not the problem of where the pain is coming from
and once the trigger points are worked on then the pain will go away permanently
instead of temporarily.
www.triggerpointbook.com
=============================================================================
University Sports Medicine
160 Farber Hall
Buffalo, New York 14214
(716) 829-2070
University of Michigan Health system Link
=============================================================================
Piriformis Syndrome
Quadriceps Stretch
Yoga and Meditation to Relax the Back
Regardless of the current situation your back is in, relaxing could be key to helping
it heal. While meditation can always be useful for achieving this, Yoga can at times
be irritating if caution is not taken. Yoga is a series of slow movements combined
with stretches and meditation to allow for an increase in flexibility and relaxation
to the muscles and joints, as well as to help optimally integrate the connection
between the mind and body. However, what might seem to be easy maneuvers should
still be treated cautiously, as your individual situation may prohibit certain Yoga
moves. One simple meditation practice that is usually met with good success is to
close your eyes and visualize yourself in the most happy and relaxing place you know
of. Sometimes just taking the time to do this can be what you need to begin the
healing process.
Medical Practitioners Link
A doctor of medicine can take the time to evaluate your condition and confirm
your specific diagnosis. Medical doctors prescribe either over the counter or
prescription only medication. They can prescribe medications that temporarily
relieve inflammation, temporarily relax muscles, and temporarily relieve pain.
Many medical doctors work with physical therapists and chiropractors to provide
conservative management for the many back pain conditions a patient can experience.
Orthopedic doctors have extended training in joint-related conditions such as this.
While Orthopedic doctors can perform back surgery, this drastic step should only be
used when all other treatment options have been exhausted, as back surgery carries
many risks, and not usually recommended for most conditions.
=============================================================================
Running Online Link
Piriformis Syndrome (aka. Pain in the Butt)
============================================================================
Piriformis Syndrome: Link
What is it?
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the
the path of the sciatic nerve. The nerve pain, called "sciatica", often goes
down the back of the thigh and/or into the lower back. The pains is deep in
the buttocks, which is made worse by sitting, climbing stairs or performing
squats. The affected leg is often externally rotated (toes point out) when
relaxed, such as when lying face down on the bed with your feet over the end
of the mattress. Some reports suggest a 6:1 female to male predominance.
The piriformis muscle assists in abducting the and laterally rotating the thigh.
It lies deep in the gluteal muscles and originates from he sacral spine and
attaches to the greater trochanter of the femur. The sciatic nerve usually
passes underneath the piriformis muscle, but in approximately 10% of the
population, travels through the muscle. It is thought that acute or chronic
injury causes swelling of the muscle and irritates the sciatic nerve, resulting
in sciatica. Patients with an aberrant course of the nerve through the muscle
are particularly predisposed to this condition.
=============================================================================
Other causes of Piriformis Syndrome when surgery fails: Link
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain
What is referred pain?
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain
Muscles and Trigger Points:
Many times your pain is actually coming from muscles and the surrounding
connective tissue (fascia).
Situation: when the muscle becomes tight or shortened and is no longer able
to relax to its full resting length a piriformis syndrome problem exists.
When muscle fibers become chronically shortened, the result is a tender nodule
in the muscle, usually in the middle of the muscle or at its attachments.
These tender areas or Trigger Points (TrPs) are named for their astonishing ability
to "trigger" or refer pain to distant areas, far from the actual origin.
=============================================================================
Referred Pain Link
According to Doctors Janet Travell and David Simons in their widely acclaimed
medical textbook, Myofascial Pain and Dysfunction: The Trigger Point Manual,
referred pain is the defining symptom of a myofascial trigger point. It is felt
most often as an oppressive deep ache, this ache can trigger a sciatica symptom
down your effected leg giving you pain both in the buttock and also throughout
the sciatic nerve as it continues down your leg with referred pain.
Some common examples of referred pain are headaches, sinus pain, and the kind
of pain in the neck that won't let you turn your head. Jaw pain, earache, and
sore throat can also be expressions of referred pain. Another is the incapacitating
pain in the side that comes from running too hard and or not used to that
particular exercise and have overdone.
Sore feet and sprained ankles are other examples of referred pain.
Stiffness and pain in a joint should always make you think first of possible trigger
points in nearby muscles that have been subjected to strain or overwork. Pain in
such joints as the knuckles, wrists, elbows, shoulders, knees, and hips are almost
always nothing more serious trigger points which are knotts that need to be
massaged in order to give your muscles relief and full flexibility.
With certain muscles, the referred pain can often be found by pressing on a
trigger point knot that is bad enough to reproduce part of its referred
pain signals. This referred pain is caused by having disruption along the
nerve impulse sciatic nerve line.
Pain referral is difficult because the mechanisms of the human nervous
system is very small and hard to see or operate on. Tiny electrochemical
impulses can be detected and measured to some extent, but not with great
accuracy do to it being so small in size.
Referred pain is happens when your neurological wiring signals get confused.
Inputs from several sources are known to converge into single neurons (nerve cells)
at the spine and are modified before being transmitted to the brain.
One electrical signal can influence another, resulting in some big problems
if the original signal is mixed up from a pinched or decompressed sciatic nerve.
The displacement of pain seems occurs in very predictable patterns with only
small variations from person to person. The predictability shows that there may
be a functional advantage to the referral of pain which helps the sufferer.
Referred pain usually occurs very often in or near a joint, telling you to
modify your exercising and to slow down so that the condition will not
be aggravated to any larger of an extent.
After you've figured out why you have referred pain you can figure out where
it is coming from and then diagnosis and treatment becomes easier for you.
remarkably easy.
In The Trigger Point Therapy Workbook, nationally certified massage therapist
Clair Davies www.triggerpointbook.com has simplified Travell and Simons'
extensive research into referred pain and made it accessible to the non
professional person in the Clair Davies self-applied trigger point massage
book which will hopefully relieve some of the referred pain, numbness,
bad sensations caused by trigger points (which are the root to the cause of the
pain.)
The Trigger Point Therapy Workbook Link
by David G. Simons, M.D.
Clair Davies www.triggerpointbook.com possesses a good combination of
attributes for the common person: He is a skilled at his profession, has good
writing skills that everyone can understand and he shows a great determination to
help everyone get over their suffering from pain.
The Muscle is an orphan organ.
Nobody really studies all the aspects of the muscle and why it gets tied up
in knots and why the referred pain is so hard to figure out the origins of
the original tied up or compressed nerve or muscle. Usually both are involved.
His book shows how to recognize and treat myofascial trigger points.
Massage therapists do study trigger points although rarely trained medically,
are trained in how to find myofascial trigger points through diagnosis and
findings in their skilled treatment of that body part.
There is no well-recognized right way to get the job done which makes it
very hard to get the scientific research and funding in order to model a
clear cut study on diagnosis and treatment.
Myofascial trigger points are a neglected subject.
Virtually all fibromyalgia patients have myofascial trigger points that are
to their total pain and lack of recovery.
There main problem is that they have many more treatable multiple trigger points.
Inactivation of the trigger points of fibromyalgia patients requires especially
delicate and skilled treatment and will take months to completely heal.
Myofascial trigger points as the most common cause of musculoskeletal pain,
but finding someone who understands these trigger points will be very difficult
as best.
The guidance in the trigger point book is a good manual for finding out and
understanding the trigger points and the musculoskeletal pain one has in
which regular doctors were not able to find or diagnose properly.
Doctors treat the pain and not the problem of where the pain is coming from
and once the trigger points are worked on then the pain will go away permanently
instead of temporarily.
www.triggerpointbook.com
=============================================================================
University Sports Medicine
160 Farber Hall
Buffalo, New York 14214
(716) 829-2070
University of Michigan Health system Link
=============================================================================
Piriformis Syndrome
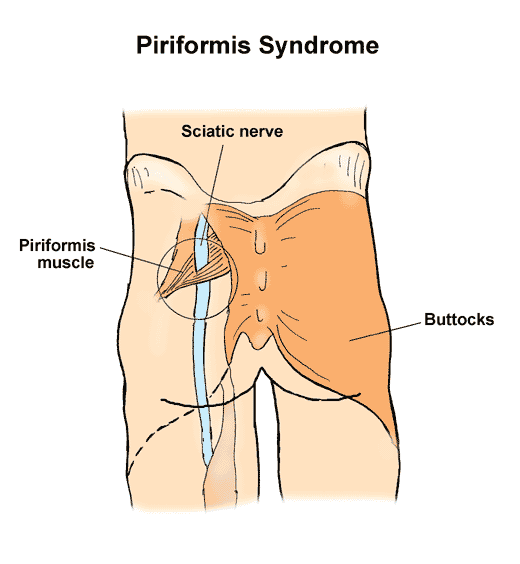 sciatic nerve passes through piriformis muscle
What is piriformis syndrome?
Piriformis syndrome refers to irritation of the sciatic nerve as it passes
through the piriformis muscle located deep in the buttock. Inflammation of
the sciatic nerve, called sciatica, causes pain in the back of the hip that
can often travel down into the leg.
How does it occur?
The piriformis muscle is located deep in the buttock and pelvis and allows
you to rotate your thigh outward. The sciatic nerve travels from your back
into your leg by passing through the piriformis muscle. If the piriformis
muscle is unusually tight or if it goes into spasm, the sciatic nerve can
become inflamed or irritated. Piriformis syndrome may also be related to
intense downhill running.
What are the symptoms? Link
You have pain deep in your buttock that may feel like a burning pain. The
pain usually travels down across your lower thigh. Your pain may increase
when you move your thigh outward, such as when you are sitting cross-legged.
sciatic nerve passes through piriformis muscle
What is piriformis syndrome?
Piriformis syndrome refers to irritation of the sciatic nerve as it passes
through the piriformis muscle located deep in the buttock. Inflammation of
the sciatic nerve, called sciatica, causes pain in the back of the hip that
can often travel down into the leg.
How does it occur?
The piriformis muscle is located deep in the buttock and pelvis and allows
you to rotate your thigh outward. The sciatic nerve travels from your back
into your leg by passing through the piriformis muscle. If the piriformis
muscle is unusually tight or if it goes into spasm, the sciatic nerve can
become inflamed or irritated. Piriformis syndrome may also be related to
intense downhill running.
What are the symptoms? Link
You have pain deep in your buttock that may feel like a burning pain. The
pain usually travels down across your lower thigh. Your pain may increase
when you move your thigh outward, such as when you are sitting cross-legged.
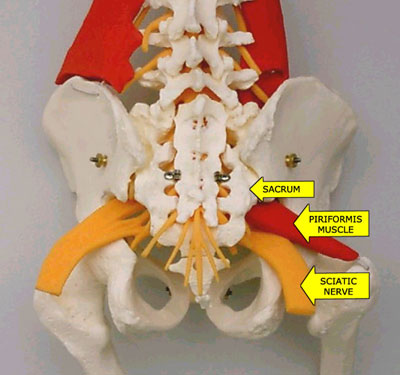 sciatic nerve runs below piriformis muscle
Link
Syndrome, piriformis: Irritation of the sciatic nerve caused by compression
of the nerve within the buttock by the piriformis muscle. Typically, the pain
of the piriformis syndrome is increased by contraction of the piriformis muscle,
prolonged sitting, or direct pressure applied to the muscle. Buttock pain is
common. The piriformis syndrome is one of the causes of sciatica.
The piriformis syndrome can cause difficulty walking due to pain in the buttock
and lower extremity.
The piriformis muscle begins at the front surface of the sacrum (the V-shaped
bone between the buttocks at the base of the spine) and passes through the greater
sciatic notch to attach to the top of the thigh bone (femur) at its bony prominence
called the greater trochanter. The gluteus maximus muscle covers over the piriformis
muscle in the buttocks.
The doctor can often detect tenderness of the piriformis muscle during a rectal
examination.
The piriformis syndrome is treated with rest and measures to reduce inflammation
of the piriformis muscle and its tendon. Treatments include piriformis stretching
exercises, physical therapy, anti-inflammatory medications, and pain medications.
With persistent symptoms, further treatment can include local injection of
anesthetic and cortisone medication.
Rarely, for severe cases, surgery is performed to relieve the pressure irritating
the sciatic nerve. During surgical operations, the piriformis muscle is either
thinned, elongated, divided, or removed.
How is it diagnosed?
Your health care provider will talk to you about when your symptoms began.
Since your sciatic nerve begins in the back, it can be irritated from a back
injury, such as a herniated disk. Your provider will ask if you have had any
injuries to your back or hip. He or she will examine your back to see if the
sciatic nerve is irritated there. He or she will examine your hip and legs
and move them to see if movement causes increased pain.
Your health care provider may order x-rays, a computed tomography (CT) scan,
or a magnetic resonance image (MRI) of your back to see if there is a back
injury. There are no x-ray tests that can detect if the nerve is being irritated
at the piriformis muscle.
How is it treated?
Treatment may include:
placing ice packs on your buttock for 20 to 30 minutes every 3 to 4 hours for
the first 2 to 3 days or until the pain goes away.
1. rest
2. taking prescribed anti-inflammatory medications or muscle relaxants
3. learning and doing stretching exercises of the piriformis muscle.
4. When can I return to my sport or activity?
5. The goal of rehabilitation is to return you to your sport or activity as
soon as is safely possible. If you return too soon you may worsen your injury,
which could lead to permanent damage. Everyone recovers from injury at a different
rate. Return to your sport or activity will be determined by how soon the nerve
recovers, not by how many days or weeks it has been since your injury occurred.
6. In general, the longer you have symptoms before you start treatment, the longer
it will take to get better.
You may safely return to your sport or activity when, starting from the top of
the list and progressing to the end, each of the following is true:
You have full range of motion in the affected leg compared to the unaffected leg.
You have full strength of the affected leg compared to the unaffected leg.
You can jog straight ahead without pain or limping.
You can sprint straight ahead without pain or limping.
You can do 45-degree cuts, first at half-speed, then at full-speed.
You can do 20-yard figures-of-eight, first at half-speed, then at full-speed.
You can do 90-degree cuts, first at half-speed, then at full-speed.
You can do 10-yard figures-of-eight, first at half-speed, then at full-speed.
You can jump on both legs without pain and you can jump on the affected leg without pain.
How I prevent piriformis syndrome?
Piriformis syndrome is best prevented by stretching the muscles that rotate your
thigh inward and outward. It is important to have a good warm-up before starting
your sport or activity.
Written by Pierre Rouzier, M.D., for McKesson Health
============================================================================
WELCOME TO
DOC PETE'S
CHIROPRACTIC Link
Piriformis Syndrome Link
=============================================================================
Piriformis Syndrome is caused by an entrapment (pinching) of the sciatic
nerve as it exits the Greater Sciatic notch in the gluteal region. There
are two normal variations for the exit of the sciatic nerve in this region.
The first places the sciatic nerve inferior (below) to the Piriformis muscle
and superior (above) the gemellus muscle. Entrapment in this area is likely
due to a myospasm or contracture (tightening or shortening respectively) of
either of these two muscles.
The second common site of entrapment is when the sciatic nerve actually pierces
the piriformis muscle itself -this can occur in about 1% to 10% of all humans.
In this case myospasm and or contraction of the piriformis muscle itself can
lead to pain along the back of the thigh to the knee, loss of sensation or
numbness and tingling in the sole of the foot.
This particular syndrome can often mimic its more notorious counterpart known
as sciatica, and that being the case, it is often misdiagnosed as sciatica..
The main difference between sciatica and piriformis syndrome is in the cause.
Sciatica is directly due to a lumbar disc pressing on the sciatic nerve as it
exits the intervertebral foramen in the lumbar spine. What both of these
complaints have in common is that both can produce pain, numbness and tingling
below the knee and into the foot. The main diagnostic tests performed by your
doctor of Chiropractic is what distinguishes one from the other. With piriformis
syndrome your chiropractor will not get positive tests results that indicate
lumbar spine involvement.
Often the patient may not be aware that there is a problem. Some cases won't
show up until a complete neurological exam is performed on the lower extremity.
The patient may have chief complaints ranging from no pain to pain in the lower
back to gluteal pain to numbness and tingling in the foot. As can be seen the
symptoms in this condition can vary widely making the doctor who is not used to
differentially diagnosing this condition from sciatica confused as to the cause
of the condition.
Many weekend athletes and people who spend long hours sitting are prone to this
syndrome. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
For the patient who sits for extended periods of time, their primary cause is
due to contracture of the piriformis muscle. In this case the piriformis muscle
is shortened and does not allow for the smooth movement of the sciatic nerve
during leg motion.
A one-time direct trauma to the pelvis is very rarely a cause for piriformis
syndrome due to the protection afforded the pelvis by the overlying musculature
and fat. The causes of myospasm are many. Over use as during excessive fast
walking without proper warm up and stretching (as during exercise), prolonged
sitting, repetitive trauma as in horseback riding and others.
As for your treatment, many variables can hamper your successful recovery.
Smoking, obesity, job and exercise as noted above in prolonged sitting and
not warming up and stretching. Any treatment plan must include stretching of
the gluteal muscles as well as stretching of the piriformis muscles.
Your Chiropractor can help you by instructing you on the proper exercises and
stretches to perform. Many Chiropractors may also prescribe some form of massage
be performed to the piriformis muscle in the gluteal region in order to relax
these muscles. Also your chiropractor may prescribe certain herbals remedies
such as valerian root and passion flower to help relax the associated muscles
during your recovery phase. Spinal adjustment as well as hip adjustment may also
be required to relieve your symptoms.
In my opinion any treatment program which does not start to bring relief in
the symptoms within three to four weeks (9-12 treatments) should be re-evaluated.
The patient should be given an exercise program that involves stretching of the
piriformis and gemelli muscles and strengthening exercises for weak muscles to
do at home (hence patient non-compliance can also increase recovery time). After
this initial nine to twelve treatments a complete re-evaluation of the symptoms
and treatment program should be done to assess the progress and to make necessary
changes to speed up recovery.
=============================================================================
=============================================================================
Epidemiology
Since an estimated 80 million Americans suffer low back pain and sciatica
annually, (8) 4.8 to 6.4 million people contract piriformis syndrome annually.
One reason for under diagnosis is that MRI, myelogram, CT, is unlikely to turn
up any evidence of piriformis syndrome. (9-11) It is a functional syndrome:
only certain positions and pressures bring out the pain, paresthesias, and
weakness that come with it. Structural imaging studies are of minimal value
here. (12-15)
Since it is sometimes considered a diagnosis of exclusion, many patients
receive painful and pointless surgical and other procedures based on limited
inquiries and faulty diagnosis.
Piriformis Syndrome is commonest among very active people such as athletes,
health club users, joggers, and performers, and those who sit a great deal
such as members of the financial community, lawyers, psychotherapists,
secretaries and vehicular drivers. After occupational causes, trauma is
the second greatest cause of piriformis syndrome. Lifting and other back
strain related activities are third, with many other initiating events
including misplaced gluteal injections, lipomas, and unusual furniture.
Clinical Experience
Treatment at first was simply physical therapy, informed and enriched by the
generous giving forth of experience from the international medical community.
In essence, the therapy lengthened the piriformis muscle, reducing spasm and
pressure on the descending sciatic nerve, and giving the nerve enough slack to
remove itself from harm's way. See the rest of the website for the specific
program. The therapy was helpful, but progress was slow. On the suggestion of
Dr. Janet Travell, we began injecting Triamcinolone Acetonide 20mg with 1.5cc
of 2% lidocaine into the motor point of the piriformis muscle, just medial to
its musculotendinous junction in the lateral buttock.
This had only rare minor and transient side-effects on non-diabetics, and
shortened the recovery time considerably.
On average 10.2 month follow-up time of 1014 cases of piriformis syndrome, more
than 80% of the patients had improved 50% or more within three months.(15) It
is important to note that these patients had suffered from piriformis syndrome
for an average of 6.2 years, and had seen an average of 6.5 clinicians before
coming to our offices.
Probably due to piriformis syndrome being considered a diagnosis of exclusion,
other, less important diagnostic entities had received undue attention in these
patients. Among these1014 cases there had been over 400 spinal, trochanteric and
gynecological surgeries, none of which was definitive, more than 1500 imaging
studies, of which less than 1/5 were relevant, and more than 10,000 appointments
with clinicians for diagnostics, epidurals, physical therapy, and alternative
methods of pain relief.
More recently we have conducted several IRB-approved studies of more specific
nerve blocks, using the toxin of the botulinum bacterium. In the latest and most
successful of these, we have found that 12,500 units of botulinum B toxin has
well above 85% efficacy, and fewer side effects than Triamcinolone and Lidocaine,
giving more relief faster, and appearing in early studies to last longer.
Containing no steroid, this preparation is also suitable for diabetics. Showing
a much more rapid decline in pain levels, and normalization of the FAIR-test,
it obviates physical therapy sessions that surpass the cost of the injection.
In summary, there are four reasons that botulinum toxin helps in the treatment
of piriformis syndrome.
A reliable correlation between diagnosis and effective treatment exists.
More than 5,000,000 currently improperly treated patients will continue to
suffer, and continue to consume health care resources in vain unless and until
adequate treatment is afforded them.
In clinical experience, injection of botulinum toxin has proven the most
effective treatment.
Cost-benefit analysis of current data strongly supports injection of botulinum
toxin in the treatment of piriformis syndrome.
Two other considerations are relevant:
Wider applicability. While the anti-insulinemic effect of steroids strongly
contraindicates their use in diabetic patients, there are virtually no documented
allergic reactions to botulinum toxins.
Longer efficacy. Steroid injection without physical therapy is generally
effective for 1-3 weeks. Botulinum toxin injections without physical therapy
are effective for at least three months. In the past, approximately 15% of
patients treated without botulinum toxin injections have had recurrence of
piriformis syndrome within three years. As of today, (14 months after our
first injection) we have seen 3 relapses following botulinum toxin injections
in 61 patients.
=============================================================================
Damn, that pain in my ass! Link
Here's what you need to know about Piriformis Syndrome (Sciatic Pain)...
by Jesse Cannone, CFT, CPRS + Steve Hefferon, CMT
If you're reading this article, it's a good bet that you have a radiating
pain running down
=============================================================================
Recovery Tip: In severe cases, the sciatic pain can run from the top of the
hip to the bottom of the foot. It is very important to recognize that changes
and shifting of pain is often times a sign of improvement. Furthermore as a
way of gauging recovery, take note of how far down the leg the pain goes. If
the pain goes to the foot one day and then only makes it to the calf and then
to the knee and then it can only make it to the hamstring that is a sign of
improvement. You should feel good about those noticeable improvements and
this should give you encouragement to keep working toward a full remission
of pain.
So how do you get rid of your pain? Will learning one new stretch be enough?
It very well may be. However depending on the severity of your condition you
may need to change your activities of daily living to include new stretches,
new exercises that include the use of the hip rotators like roller-blading,
basketball, tennis, etc, and even better, specific corrective exercise specific
to your situation... like those covered in our video. As always, learn as much
as you can about your condition, so that you can ask the tough questions to
your healthcare providers and get the best care possible.
One last point, sciatic pain is not caused by a lack of prescription
medications so don't think that taking some anti-inflammatory or muscle
relaxants will fix it... it won't! Also, many people are able to eliminate
sciatic pain within days just by performing a few exercises and stretches...
but not general exercise... the exact corrective exercises and stretches
they need to do.
=============================================================================
Piriformis Syndrome Link
A Real Pain in the Butt
Dr. Tim Maggs
For the Washington Running Report
=============================================================================
If you've ever felt pain in the hip, pain in the center of the butt, or pain
down the back of the leg, you likely are suffering, at least partially, with
piriformis syndrome. The piriformis is a muscle which runs from your sacrum
(mid-line base of spine) to the outer hip bone (trochanter). This muscle
truly works overtime on anyone who runs at all. The muscles in and around the
gluteal region help with three areas: 1) rotation of the hip and leg, 2)
balance while one foot is off the ground, and 3) stability for the pelvic
region. Needless to say, all of these characteristics are needed by runners.
Conclusion--the piriformis muscle is pretty important for all of us.
Injuries to the Piriformis
This muscle is a prime candidate for repetitive motion injury (RMI). RMI
occurs when a muscle is asked to perform beyond its level of capability,
not given enough time to recover, and asked to perform again. The typical
response from a muscle in this situation is to tighten, which is a defensive
response. This tightness, however, manifests itself in several ways to a runner.
The first symptom suggesting piriformis syndrome would be pain in and around
the outer hip bone. The tightness of the muscle produces increased tension
between the tendon and the bone which produces either direct discomfort and
pain or an increased tension in the joint, producing a bursitis. A bursitis
is an inflammation of the fluid filled sac in a joint caused by an elevation
of stress and tension within that joint.
The second symptom suggesting piriformis syndrome would be pain directly in
the center of the buttocks. Although this is not as common as the other two
symptoms, this pain can be elicited with direct compression over the belly
of the buttocks area. A tight muscle is a sore muscle upon compression due
to a reduced blood flow to that muscle.
The third symptom suggesting piriformis syndrome is a sciatic neuralgia, or
pain from the buttocks down the back of the leg and sometimes into different
portions of the lower leg. The sciatic nerve runs right through the belly of
the piriformis muscle and if the piriformis muscle contracts from being overused,
the sciatic nerve now becomes strangled, producing pain, tingling, and numbness.
Simple Physiology
Any muscle repetitively used needs to have an opportunity to recover. This
recovery can either be on Nature's clock, or can be facilitated and sped up
with proper knowledge and treatment. Since the muscle is tightening due to
overuse, continued use will only make it worse. This injured muscle needs to
relax and have increased blood flow to it for more rapid healing. The tightness
also reduces the normal blood flow going to the muscle, reducing the speed wit
which the muscle can recover. To encourage fresh, oxygen-rich blood to the
muscle is the most powerful means of getting the muscle to begin to relax and
function normally. Multiple massages per day to this area are greatly encouraged.
The next step in this "recovery" process is to use a tennis ball under the butt
and hip area. While sitting on the floor, roll away from the side of involvement
and place a tennis ball just inside the outer hip bone under the butt area. As
you begin to allow your weight onto the tennis ball, note areas of increased pain
and soreness. Trigger points will tend to accumulate in a repetitively used muscle,
and until these toxins are manually broken up and eliminated, the muscle will have
an artificial ceiling with regard to flexibility potential and recovery potential.
So, if it's sore and hurts while you are sitting on it, you're doing a good job.
Let the ball work under each spot for fifteen to twenty seconds before moving it
to another area. Once you've been on the ball for four to five minutes, put the
ankle of the involved leg over the knee of the noninvolved leg (crossing your legs).
Now place the tennis ball just inside the outer hip bone again and work the tendon
of the piriformis muscle. While this pain is typically excruciating and takes some
time to effectively reduce, the benefits here are huge. Be patient, be consistent,
and good things will happen.
Additional Treatments
Due to the fact that the sciatic neuralgia and the hip bursitis or tendonitis are
both inflammatory in nature, ice, or cryotherapy, over the involved area fifteen
to twenty minutes at a time will be beneficial. This should be done multiple
times per day.
Stretching of the hip muscles should not be done until the acute pain is gone.
Then, begin with gentle stretching, such as the cross-legged stretch, while pulling
up on the knee. The muscle should have increased flexibility before an active return
to running.
Finally, I always discourage the use of pharmaceutical anti- inflammatories. Not
only do they greatly aggravate the intestines, they suggest an artificial wellness
that can lead to bigger problems. Proteolytic enzymes, such as bromelain, are both
natural and extremely beneficial with no side effects. For more information, visit
your health food store or check out Rehab Plus on our website.
For further information, Dr. Maggs can be reached at (518) 869-1884, his Web site:
Dr. Maggs or via e-mail Running Doctor
=============================================================================
lose the back pain Link
Sciatica (Sciatic Pain, Piriformis Syndrome)
=============================================================================
Sciatica commonly refers to pain that radiates along the sciatic nerve and is
typically felt in the buttocks, down the back of the leg and possibly to the
foot. Sciatica is one of the most common forms of pain caused by compression
of the spinal nerves. Often the leg pain often feels much worse than the back
pain. Numbness, tingling, and a burning or prickling sensation in the back and
legs are also common symptoms.
Sciatica is actually a symptom and not disease. The term literally means that
a patient has pain down the leg from compression on the sciatic nerve. Usually
a herniated disc causes the sciatic pain. The diagnosis is what is causing
the compression (such as a disc herniation).
Most cases of sciatica are caused by a simple irritation to the nerve and will
get better with time. However, some sciatica symptoms may indicate a permanently
injured nerve. This is particularly if true weakness or numbness is present in
the back or the leg.
=============================================================================
syracusechargers.org
A Real Pain in the .... Link
=============================================================================
A while back I noted that very often I will be visited by a runner complaining
that his or her "sciatica is acting up." Generally, what they are saying is
they have some pain in the back of the thigh, maybe some in the buttock, low
back or even into the calf. Sciatica, by definition, is an inflammation or
irritation of the sciatic nerve, the largest nerve in the body, which originates
in the lower spine in the form of five separate nerve roots which join together
and traverse the buttock and descend into the lower limb all the way to the toes.
The problem is, sciatica is a vague term that doesn't really tell us very much
about the underlying reason for these symptoms since there can be several
explanations for them.
Some of the possible causes of this ailment which reviewed then included
sacroiliac joint dysfunction, lumbar spine arthritis or herniated discs, chronic
hamstring strains and a rather esoteric-sounding problem called the piriformis
syndrome, which we want to look at in more detail now.
The piriformis muscle is a relatively large structure found in the buttock,
originating on the sacrum (the lower part of the spine, or tailbone) and
crossing over at a slightly downward angle to the outside of the hip, attaching
to the outer portion of the upper thighbone (femur). Its function is to laterally
rotate and extend the hip joint. It is only one of several muscles in the buttock
which, as we've said, is an area through which the sciatic nerve passes, but the
piriformis has been singled-out as a potential cause of sciatica because anatomists
have found that in a fair number of people, all or part of the sciatic nerve
goes directly through this particular muscle. (The exact percentage of people
is unknown -- studies vary widely with some experts reporting 20% and others
as many as 60%!)
The speculation is that in these subjects, a tight piriformis muscle will
"squeeze" the nerve, causing irritation and subsequent pain. Runners, of course,
would be more likely to have a tight piriformis since they would be using it
more often and more intensely, especially during the push-off phase of gait when
hip extension and lateral rotation are needed most, but theoretically anyone
could experience this problem really if posture and biomechanics of walking
are abnormal.
Is it real? Does piriformis syndrome really exist? Well, the fact that we call
it a syndrome -- which in the medical field is a code word for "we don't really
know exactly what it is or know for sure what really causes it" -- tells us a lot.
It seems reasonable that the piriformis, like any muscle, can become overused
and painful, especially with running. But, like any muscle, this irritated muscle
can cause radiating or referred symptoms which would mimic sciatica pain while
there may not necessarily be any actual injury to the nerve itself. Or, conversely,
there are other potential causes of nerve inflammation in the buttock with no
involvement of the piriformis muscle. My favorite example is something actually
designated in the medical literature as "fat wallet syndrome," which is found most
often in long-distance drivers (truckers, salesmen). The prolonged pressure of a
billfold full of cash and credit-cards on the sciatic nerve is a not-infrequent
cause of sciatica. (The cure, of course, is for me to relief the patient of the
offending object...)
==============================================================================
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain
The Trigger Point Therapy Workbook;
You're Self-Treatment Guide for Pain Relief
Buy this book,, "The Trigger Point Therapy Workbook: Your Self-Treatment
Guide for Pain Relief" : Link
The Book Introduction Link
==============================================================================
They've tried chiropractic, acupuncture, magnets, pain diets, and herbal therapy.
They take their pain medicine and dutifully do their stretching exercises. Sometimes
they feel better for a while, but the pain always comes back. Nothing really seems
to get to the bottom of the problem. Despite being told there are no guarantees
of success, they fear surgery may be the only solution. They're beginning to wonder
if anybody really knows anything about pain.
If all this describes your own situation or that of someone you care about, this
book may provide the help you've been seeking. It proposes to give you a sensible
explanation of what's wrong and help you find the real cause of your pain. Even
better, it may well show you how to get rid of the pain yourself, hands-on. No
doctors. No pills. No bills.
There is growing evidence that most of our common aches and pains--and many
other puzzling physical complaints--are actually caused by trigger points, or
small contraction knots, in the muscles of the body. Pain clinic doctors skilled
at detecting and treating trigger points have found that they're the primary cause
of pain roughly seventy-five percent of the time and are at least a part of virtually
every pain problem. Even fibromyalgia, which is known to afflict millions of people,
is thought in many instances to have its beginning with trigger points.
Trigger points are known to cause headaches, neck and jaw pain, low back pain, the
symptoms of carpal tunnel syndrome, and many kinds of joint pain mistakenly ascribed
to arthritis, tendonitis, bursitis, or ligament injury. Trigger points cause problems
as diverse as earaches, dizziness, nausea, heartburn, false heart pain, heart
arrhythmia,
tennis elbow and genital pain. Trigger points can also cause colic in babies and bed-
wetting in older children and may be a contributing cause of such childhood horrors as
scoliosis, attention deficit disorder and dyslexia. They are a cause of sinus pain and
congestion. They may play a part in chronic fatigue and lowered resistance to infection.
And because trigger points can be responsible for long-term pain and disability that
seem to have no means of relief, they can cause depression.
The problems trigger points cause can be surprisingly easy to fix; in fact most people
can do it themselves if they have the right information. That's good, because the time
has come for ordinary people to take things into their own hands. The reason is that an
appallingly high percentage of doctors and other practitioners are still pretty much
out of the loop regarding trigger points, despite their having been written about in
medical journals for over sixty years. There has been, and continues to be, great
resistance to the whole idea.
Why has the medical profession not embraced the idea of trigger points? Partly, it's
because trigger points are commonly confused with acupressure points. Acupressure,
which has come down to us from ancient Chinese medicine, is alleged to have a positive
effect on supposed flows of energy throughout the body. Although acupressure and
other Eastern methods of healing do seem to have a beneficial effect, they're very
resistant to solid scientific investigation and are viewed by many doctors and a large
segment of the public as quack medicine with no proven results. If you don't know the
difference, the claims about trigger points sound like quack medicine too.
Our knowledge of trigger points, however, comes right out of Western medical research.
Trigger points are real. They can be felt with the fingers. They emit distinctive
electrical signals that can be measured by sensitive electronic equipment. Trigger
points have also been photographed in muscle tissue with the aid of the electron
microscope.
Most of what is known about trigger points is very well documented in the two-volume
medical text Myofascial Pain and Dysfunction: The Trigger Point Manual, by Janet Travell
and David Simons. These books tell virtually all there is to know about trigger points,
and the prospects for pain relief are very exciting. Much of the information in the
Trigger Point Manual is couched in difficult scientific terms but basic trigger point
science isn't hard to grasp if it's put into everyday language.
Travell and Simons describe a trigger point as simply a small contraction knot in muscle
tissue. It often feels like a partly cooked piece of macaroni or like a pea buried deep
in the muscle. A trigger point affects a muscle by keeping it both tight and weak. At
the same time, a trigger point maintains a hard contraction on the muscle fibers that
are directly connected to it. In turn, these taut bands of muscle fiber keep constant
tension on the muscle's attachments, often producing symptoms in adjacent joints. The
constant tension in the fibers of the trigger point itself restricts circulation in its
immediate area. The resulting accumulation of the by-products of metabolism, as well as
deprivation of the oxygen and nutrients needed for metabolism can perpetuate trigger points
for months, or even years, unless some intervention occurs. It's this self-sustaining
vicious cycle that needs to be broken.
The difficulty in treating trigger points is that they typically send pain to some other
site. Most conventional treatment of pain is based on the assumption that the cause of
pain will be found at the site of the pain. But trigger points almost always send their
pain elsewhere. This referred pain is what has always thrown everybody off, including
most doctors and much of the rest of the health-care community. According to Travell
and Simons, conventional treatments for pain so often fail because they focus on the
pain itself, treating the site of the pain, and overlooking and failing to treat the
cause, which may be some distance away.
Even worse than routinely treating the site of the pain is the pharmaceutical treatment
of the whole body for what is usually a local problem. Painkilling drugs, the increasingly
expensive treatment of choice these days, give us the illusion that something good is
happening, when in reality they only mask the problem. Most common pain, like headaches,
muscle aches, and joint pain, is a warning-a protective response to muscle overuse or
trauma. Pain is telling you that something is wrong and needs correction. It's not good
medicine to kill the messenger and ignore the message. When pain is seen in its true role
as the messenger and not the affliction itself, treatment can be directed to the cause
of pain.
Luckily, referred pain is now known to occur in predictable patterns. The valuable medical
advance made by Travell and Simons and their brilliant illustrator, Barbara Cummings,
has been in delineating these very patterns. Once you know where to look, trigger points
are easily located by touch and deactivated by any of several methods.
Unfortunately, the two clinically oriented methods put forth in The Trigger Point Manual
don't lend themselves to self-treatment. The goal of this book is to build on the work of
Travell and Simons and provide a more practical and cost-effective approach to pain
therapy: a classic do-it-yourself approach, rather than multiple professional office
visits. This new approach is a system of self-applied massage directed specifically at
trigger points. Significant relief of symptoms often comes in just minutes. Most problems
can be eliminated within three to ten days. Even long-standing chronic conditions can be
cleared up in as little as six weeks. Results may be longer in coming for those who
suffer from fibromyalgia, chronic fatigue, or widespread myofascial pain syndrome, but
even they can experience continuing progress and can have genuine hope of significant
improvement in their condition.
Self-applied trigger point massage works by accomplishing three things: it breaks into the
chemical and neurological feedback loop that maintains the myofascial contraction; it
increases circulation that has been restricted by the contracted tissue; and it directly
stretches the trigger point's knotted muscle fibers. The illustrations in this book show
you how to find the trigger points that are generating your specific problems, as well
as the exact hands-on techniques for deactivating them. Special attention has been given
to designing methods of massage that do no damage to hands that may already be in trouble
from overuse.
This book's primary use is as a self-instruction manual, but it can also be used as a
textbook for classroom use. This simplified and direct approach to treating myofascial
pain with self-applied massage can constitute a foundational course in trigger point
therapy in any professional training curriculum. Students in chiropractic colleges,
physical therapy departments, and massage schools will derive particular benefit. If
they can learn how to interpret their own referred pain and how to find and treat their
own trigger points, they will know exactly what to do when they encounter similar
problems in their future clients.
A class in self-applied trigger point massage would be a boon in medical schools for
exactly the same reasons. When new doctors can learn how to fix their own pain with
self-applied massage, they are in better touch with the realities of pain and with the
great potential in the treatment of trigger points. Such an addition to medical education
would profoundly improve the treatment of pain and lower much of its cost.
And it's not too late for physicians already in practice to learn about trigger points
and myofascial pain and put the knowledge to good use. They will find this book a quick
and practical introduction to the magnificent work of Travell and Simons and this
neglected branch of medicine. Hopefully, many will be encouraged to go to Travell and
Simons' Trigger Point Manual for a deeper scientific understanding and for even greater
benefit to their practice. A large segment of the public needs help and encouragement
in learning how to deal with their trigger point-induced pain. No one is better positioned
to provide this help than the medical community.
The medical profession is not unaware of the deficiencies of current methods of treating
pain. Doctors hurt too. Many of them worry like the rest of us about the relentless popping
of pills, and many experience frustration with their inability to offer better solutions
to their patients. Trigger point therapy, whether self-applied or administered by a
professional, has the potential to truly revolutionize pain treatment throughout the
world.
=============================================================================
Sciatica, Piriformis Syndrome, PIRIFORMIS TRIGGER POINTS Link
Sciatic Nerve Impingement, Erectile Dysfunction,
Buttocks Pain, Rectal Pain, Anal Pain,
Leg Pain, Tingling in Legs
According to Doctors Janet Travell and David Simons in their widely acclaimed medical
textbook, Myofascial Pain and Dysfunction: The Trigger Point Manual, myofascial
trigger points (tiny contraction knots) in overworked gluteus minimus and piriformis
muscles in the buttocks are actually the most frequent cause of sciatica.
Referred Symptoms
Symptoms of sciatica include aching pain, numbness, tingling, burning and
hypersensitivity in your low back, buttocks, hips, and down your legs into your
ankles and feet. Simple aching pain in these areas usually is referred from gluteus
minimus trigger points.
Piriformis trigger points, by keeping the muscles tight and rock hard, can cause
actual sciatic nerve compression. Pain from piriformis trigger points is harsher
and more electric than pain from gluteus minimus trigger points and is felt in
the back of the thigh, the calf, and the sole of the foot. There may also be other
abnormal sensations, such as numbness, tingling, burning, or hypersensitivity,
in any of these areas.
Piriformis Syndrome
A piriformis muscle that is shortened and swollen by trigger points can also
compress numerous other nerves and blood vessels coming out of the pelvis. This
can result in a sense of swelling in the buttocks, leg, calf, and foot. In addition,
a tight piriformis muscle can impinge upon the pudendal nerve, causing impotence
in males and pain in the groin, genitals, or rectal area of either gender.
Piriformis muscles that compress gluteal nerves and blood vessels are believed
to be responsible for gluteal muscle atrophy, wherein one or both buttocks waste
away.
For decades, the medical profession has known this particular group of sciatic
symptoms as "piriformis syndrome," although the cause of the piriformis enlargement
was never really understood. Surgical release of the piriformis muscle for the
treatment of sciatica was once a common treatment. Amazingly, this operation is
still performed by surgeons who are unaware of the effects of myofascial trigger
points.
Misdiagnosis:
In the medical world, sciatica is routinely assumed to be caused by pressure on
the sciatic nerve as a result of a compressed disk or other spinal abnormality.
Surgery on the spine in a search for the cause of presumed sciatic nerve impingement
is very common, even though it regularly fails to erase sciatic symptoms.
Doctors Travell and Simons believe that traditional medical solutions for sciatica
and piriformis syndrome is needlessly expensive and have an unacceptably high rate
of failure. Trigger points should be at the top of the list during any examination
for pain, numbness and other abnormal sensations in the hips and legs. Wider recognition
of the myofascial causes of sciatica could eliminate many unnecessary surgical
operations.
Self-Treatment: Myofascial Pain and Dysfunction: The Trigger Point Manual
You don't have to wait for the medical community to abandon antiquated methods and
catch up with trigger point science. You can take care of your own trigger points.
In The Trigger Point Therapy Workbook, nationally certified massage therapist Clair
Davies has simplified Travell and Simons' extensive research into myofascial pain
and made it accessible to the layman. His innovative methods of self-applied trigger
point massage will get rid of the numbness, tingling and aching pain of sciatica
and piriformis syndrome when trigger points are the cause. To learn more, please
visit the homepage.
sciatic nerve runs below piriformis muscle
Link
Syndrome, piriformis: Irritation of the sciatic nerve caused by compression
of the nerve within the buttock by the piriformis muscle. Typically, the pain
of the piriformis syndrome is increased by contraction of the piriformis muscle,
prolonged sitting, or direct pressure applied to the muscle. Buttock pain is
common. The piriformis syndrome is one of the causes of sciatica.
The piriformis syndrome can cause difficulty walking due to pain in the buttock
and lower extremity.
The piriformis muscle begins at the front surface of the sacrum (the V-shaped
bone between the buttocks at the base of the spine) and passes through the greater
sciatic notch to attach to the top of the thigh bone (femur) at its bony prominence
called the greater trochanter. The gluteus maximus muscle covers over the piriformis
muscle in the buttocks.
The doctor can often detect tenderness of the piriformis muscle during a rectal
examination.
The piriformis syndrome is treated with rest and measures to reduce inflammation
of the piriformis muscle and its tendon. Treatments include piriformis stretching
exercises, physical therapy, anti-inflammatory medications, and pain medications.
With persistent symptoms, further treatment can include local injection of
anesthetic and cortisone medication.
Rarely, for severe cases, surgery is performed to relieve the pressure irritating
the sciatic nerve. During surgical operations, the piriformis muscle is either
thinned, elongated, divided, or removed.
How is it diagnosed?
Your health care provider will talk to you about when your symptoms began.
Since your sciatic nerve begins in the back, it can be irritated from a back
injury, such as a herniated disk. Your provider will ask if you have had any
injuries to your back or hip. He or she will examine your back to see if the
sciatic nerve is irritated there. He or she will examine your hip and legs
and move them to see if movement causes increased pain.
Your health care provider may order x-rays, a computed tomography (CT) scan,
or a magnetic resonance image (MRI) of your back to see if there is a back
injury. There are no x-ray tests that can detect if the nerve is being irritated
at the piriformis muscle.
How is it treated?
Treatment may include:
placing ice packs on your buttock for 20 to 30 minutes every 3 to 4 hours for
the first 2 to 3 days or until the pain goes away.
1. rest
2. taking prescribed anti-inflammatory medications or muscle relaxants
3. learning and doing stretching exercises of the piriformis muscle.
4. When can I return to my sport or activity?
5. The goal of rehabilitation is to return you to your sport or activity as
soon as is safely possible. If you return too soon you may worsen your injury,
which could lead to permanent damage. Everyone recovers from injury at a different
rate. Return to your sport or activity will be determined by how soon the nerve
recovers, not by how many days or weeks it has been since your injury occurred.
6. In general, the longer you have symptoms before you start treatment, the longer
it will take to get better.
You may safely return to your sport or activity when, starting from the top of
the list and progressing to the end, each of the following is true:
You have full range of motion in the affected leg compared to the unaffected leg.
You have full strength of the affected leg compared to the unaffected leg.
You can jog straight ahead without pain or limping.
You can sprint straight ahead without pain or limping.
You can do 45-degree cuts, first at half-speed, then at full-speed.
You can do 20-yard figures-of-eight, first at half-speed, then at full-speed.
You can do 90-degree cuts, first at half-speed, then at full-speed.
You can do 10-yard figures-of-eight, first at half-speed, then at full-speed.
You can jump on both legs without pain and you can jump on the affected leg without pain.
How I prevent piriformis syndrome?
Piriformis syndrome is best prevented by stretching the muscles that rotate your
thigh inward and outward. It is important to have a good warm-up before starting
your sport or activity.
Written by Pierre Rouzier, M.D., for McKesson Health
============================================================================
WELCOME TO
DOC PETE'S
CHIROPRACTIC Link
Piriformis Syndrome Link
=============================================================================
Piriformis Syndrome is caused by an entrapment (pinching) of the sciatic
nerve as it exits the Greater Sciatic notch in the gluteal region. There
are two normal variations for the exit of the sciatic nerve in this region.
The first places the sciatic nerve inferior (below) to the Piriformis muscle
and superior (above) the gemellus muscle. Entrapment in this area is likely
due to a myospasm or contracture (tightening or shortening respectively) of
either of these two muscles.
The second common site of entrapment is when the sciatic nerve actually pierces
the piriformis muscle itself -this can occur in about 1% to 10% of all humans.
In this case myospasm and or contraction of the piriformis muscle itself can
lead to pain along the back of the thigh to the knee, loss of sensation or
numbness and tingling in the sole of the foot.
This particular syndrome can often mimic its more notorious counterpart known
as sciatica, and that being the case, it is often misdiagnosed as sciatica..
The main difference between sciatica and piriformis syndrome is in the cause.
Sciatica is directly due to a lumbar disc pressing on the sciatic nerve as it
exits the intervertebral foramen in the lumbar spine. What both of these
complaints have in common is that both can produce pain, numbness and tingling
below the knee and into the foot. The main diagnostic tests performed by your
doctor of Chiropractic is what distinguishes one from the other. With piriformis
syndrome your chiropractor will not get positive tests results that indicate
lumbar spine involvement.
Often the patient may not be aware that there is a problem. Some cases won't
show up until a complete neurological exam is performed on the lower extremity.
The patient may have chief complaints ranging from no pain to pain in the lower
back to gluteal pain to numbness and tingling in the foot. As can be seen the
symptoms in this condition can vary widely making the doctor who is not used to
differentially diagnosing this condition from sciatica confused as to the cause
of the condition.
Many weekend athletes and people who spend long hours sitting are prone to this
syndrome. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
For the patient who sits for extended periods of time, their primary cause is
due to contracture of the piriformis muscle. In this case the piriformis muscle
is shortened and does not allow for the smooth movement of the sciatic nerve
during leg motion.
A one-time direct trauma to the pelvis is very rarely a cause for piriformis
syndrome due to the protection afforded the pelvis by the overlying musculature
and fat. The causes of myospasm are many. Over use as during excessive fast
walking without proper warm up and stretching (as during exercise), prolonged
sitting, repetitive trauma as in horseback riding and others.
As for your treatment, many variables can hamper your successful recovery.
Smoking, obesity, job and exercise as noted above in prolonged sitting and
not warming up and stretching. Any treatment plan must include stretching of
the gluteal muscles as well as stretching of the piriformis muscles.
Your Chiropractor can help you by instructing you on the proper exercises and
stretches to perform. Many Chiropractors may also prescribe some form of massage
be performed to the piriformis muscle in the gluteal region in order to relax
these muscles. Also your chiropractor may prescribe certain herbals remedies
such as valerian root and passion flower to help relax the associated muscles
during your recovery phase. Spinal adjustment as well as hip adjustment may also
be required to relieve your symptoms.
In my opinion any treatment program which does not start to bring relief in
the symptoms within three to four weeks (9-12 treatments) should be re-evaluated.
The patient should be given an exercise program that involves stretching of the
piriformis and gemelli muscles and strengthening exercises for weak muscles to
do at home (hence patient non-compliance can also increase recovery time). After
this initial nine to twelve treatments a complete re-evaluation of the symptoms
and treatment program should be done to assess the progress and to make necessary
changes to speed up recovery.
=============================================================================
=============================================================================
Epidemiology
Since an estimated 80 million Americans suffer low back pain and sciatica
annually, (8) 4.8 to 6.4 million people contract piriformis syndrome annually.
One reason for under diagnosis is that MRI, myelogram, CT, is unlikely to turn
up any evidence of piriformis syndrome. (9-11) It is a functional syndrome:
only certain positions and pressures bring out the pain, paresthesias, and
weakness that come with it. Structural imaging studies are of minimal value
here. (12-15)
Since it is sometimes considered a diagnosis of exclusion, many patients
receive painful and pointless surgical and other procedures based on limited
inquiries and faulty diagnosis.
Piriformis Syndrome is commonest among very active people such as athletes,
health club users, joggers, and performers, and those who sit a great deal
such as members of the financial community, lawyers, psychotherapists,
secretaries and vehicular drivers. After occupational causes, trauma is
the second greatest cause of piriformis syndrome. Lifting and other back
strain related activities are third, with many other initiating events
including misplaced gluteal injections, lipomas, and unusual furniture.
Clinical Experience
Treatment at first was simply physical therapy, informed and enriched by the
generous giving forth of experience from the international medical community.
In essence, the therapy lengthened the piriformis muscle, reducing spasm and
pressure on the descending sciatic nerve, and giving the nerve enough slack to
remove itself from harm's way. See the rest of the website for the specific
program. The therapy was helpful, but progress was slow. On the suggestion of
Dr. Janet Travell, we began injecting Triamcinolone Acetonide 20mg with 1.5cc
of 2% lidocaine into the motor point of the piriformis muscle, just medial to
its musculotendinous junction in the lateral buttock.
This had only rare minor and transient side-effects on non-diabetics, and
shortened the recovery time considerably.
On average 10.2 month follow-up time of 1014 cases of piriformis syndrome, more
than 80% of the patients had improved 50% or more within three months.(15) It
is important to note that these patients had suffered from piriformis syndrome
for an average of 6.2 years, and had seen an average of 6.5 clinicians before
coming to our offices.
Probably due to piriformis syndrome being considered a diagnosis of exclusion,
other, less important diagnostic entities had received undue attention in these
patients. Among these1014 cases there had been over 400 spinal, trochanteric and
gynecological surgeries, none of which was definitive, more than 1500 imaging
studies, of which less than 1/5 were relevant, and more than 10,000 appointments
with clinicians for diagnostics, epidurals, physical therapy, and alternative
methods of pain relief.
More recently we have conducted several IRB-approved studies of more specific
nerve blocks, using the toxin of the botulinum bacterium. In the latest and most
successful of these, we have found that 12,500 units of botulinum B toxin has
well above 85% efficacy, and fewer side effects than Triamcinolone and Lidocaine,
giving more relief faster, and appearing in early studies to last longer.
Containing no steroid, this preparation is also suitable for diabetics. Showing
a much more rapid decline in pain levels, and normalization of the FAIR-test,
it obviates physical therapy sessions that surpass the cost of the injection.
In summary, there are four reasons that botulinum toxin helps in the treatment
of piriformis syndrome.
A reliable correlation between diagnosis and effective treatment exists.
More than 5,000,000 currently improperly treated patients will continue to
suffer, and continue to consume health care resources in vain unless and until
adequate treatment is afforded them.
In clinical experience, injection of botulinum toxin has proven the most
effective treatment.
Cost-benefit analysis of current data strongly supports injection of botulinum
toxin in the treatment of piriformis syndrome.
Two other considerations are relevant:
Wider applicability. While the anti-insulinemic effect of steroids strongly
contraindicates their use in diabetic patients, there are virtually no documented
allergic reactions to botulinum toxins.
Longer efficacy. Steroid injection without physical therapy is generally
effective for 1-3 weeks. Botulinum toxin injections without physical therapy
are effective for at least three months. In the past, approximately 15% of
patients treated without botulinum toxin injections have had recurrence of
piriformis syndrome within three years. As of today, (14 months after our
first injection) we have seen 3 relapses following botulinum toxin injections
in 61 patients.
=============================================================================
Damn, that pain in my ass! Link
Here's what you need to know about Piriformis Syndrome (Sciatic Pain)...
by Jesse Cannone, CFT, CPRS + Steve Hefferon, CMT
If you're reading this article, it's a good bet that you have a radiating
pain running down
=============================================================================
Recovery Tip: In severe cases, the sciatic pain can run from the top of the
hip to the bottom of the foot. It is very important to recognize that changes
and shifting of pain is often times a sign of improvement. Furthermore as a
way of gauging recovery, take note of how far down the leg the pain goes. If
the pain goes to the foot one day and then only makes it to the calf and then
to the knee and then it can only make it to the hamstring that is a sign of
improvement. You should feel good about those noticeable improvements and
this should give you encouragement to keep working toward a full remission
of pain.
So how do you get rid of your pain? Will learning one new stretch be enough?
It very well may be. However depending on the severity of your condition you
may need to change your activities of daily living to include new stretches,
new exercises that include the use of the hip rotators like roller-blading,
basketball, tennis, etc, and even better, specific corrective exercise specific
to your situation... like those covered in our video. As always, learn as much
as you can about your condition, so that you can ask the tough questions to
your healthcare providers and get the best care possible.
One last point, sciatic pain is not caused by a lack of prescription
medications so don't think that taking some anti-inflammatory or muscle
relaxants will fix it... it won't! Also, many people are able to eliminate
sciatic pain within days just by performing a few exercises and stretches...
but not general exercise... the exact corrective exercises and stretches
they need to do.
=============================================================================
Piriformis Syndrome Link
A Real Pain in the Butt
Dr. Tim Maggs
For the Washington Running Report
=============================================================================
If you've ever felt pain in the hip, pain in the center of the butt, or pain
down the back of the leg, you likely are suffering, at least partially, with
piriformis syndrome. The piriformis is a muscle which runs from your sacrum
(mid-line base of spine) to the outer hip bone (trochanter). This muscle
truly works overtime on anyone who runs at all. The muscles in and around the
gluteal region help with three areas: 1) rotation of the hip and leg, 2)
balance while one foot is off the ground, and 3) stability for the pelvic
region. Needless to say, all of these characteristics are needed by runners.
Conclusion--the piriformis muscle is pretty important for all of us.
Injuries to the Piriformis
This muscle is a prime candidate for repetitive motion injury (RMI). RMI
occurs when a muscle is asked to perform beyond its level of capability,
not given enough time to recover, and asked to perform again. The typical
response from a muscle in this situation is to tighten, which is a defensive
response. This tightness, however, manifests itself in several ways to a runner.
The first symptom suggesting piriformis syndrome would be pain in and around
the outer hip bone. The tightness of the muscle produces increased tension
between the tendon and the bone which produces either direct discomfort and
pain or an increased tension in the joint, producing a bursitis. A bursitis
is an inflammation of the fluid filled sac in a joint caused by an elevation
of stress and tension within that joint.
The second symptom suggesting piriformis syndrome would be pain directly in
the center of the buttocks. Although this is not as common as the other two
symptoms, this pain can be elicited with direct compression over the belly
of the buttocks area. A tight muscle is a sore muscle upon compression due
to a reduced blood flow to that muscle.
The third symptom suggesting piriformis syndrome is a sciatic neuralgia, or
pain from the buttocks down the back of the leg and sometimes into different
portions of the lower leg. The sciatic nerve runs right through the belly of
the piriformis muscle and if the piriformis muscle contracts from being overused,
the sciatic nerve now becomes strangled, producing pain, tingling, and numbness.
Simple Physiology
Any muscle repetitively used needs to have an opportunity to recover. This
recovery can either be on Nature's clock, or can be facilitated and sped up
with proper knowledge and treatment. Since the muscle is tightening due to
overuse, continued use will only make it worse. This injured muscle needs to
relax and have increased blood flow to it for more rapid healing. The tightness
also reduces the normal blood flow going to the muscle, reducing the speed wit
which the muscle can recover. To encourage fresh, oxygen-rich blood to the
muscle is the most powerful means of getting the muscle to begin to relax and
function normally. Multiple massages per day to this area are greatly encouraged.
The next step in this "recovery" process is to use a tennis ball under the butt
and hip area. While sitting on the floor, roll away from the side of involvement
and place a tennis ball just inside the outer hip bone under the butt area. As
you begin to allow your weight onto the tennis ball, note areas of increased pain
and soreness. Trigger points will tend to accumulate in a repetitively used muscle,
and until these toxins are manually broken up and eliminated, the muscle will have
an artificial ceiling with regard to flexibility potential and recovery potential.
So, if it's sore and hurts while you are sitting on it, you're doing a good job.
Let the ball work under each spot for fifteen to twenty seconds before moving it
to another area. Once you've been on the ball for four to five minutes, put the
ankle of the involved leg over the knee of the noninvolved leg (crossing your legs).
Now place the tennis ball just inside the outer hip bone again and work the tendon
of the piriformis muscle. While this pain is typically excruciating and takes some
time to effectively reduce, the benefits here are huge. Be patient, be consistent,
and good things will happen.
Additional Treatments
Due to the fact that the sciatic neuralgia and the hip bursitis or tendonitis are
both inflammatory in nature, ice, or cryotherapy, over the involved area fifteen
to twenty minutes at a time will be beneficial. This should be done multiple
times per day.
Stretching of the hip muscles should not be done until the acute pain is gone.
Then, begin with gentle stretching, such as the cross-legged stretch, while pulling
up on the knee. The muscle should have increased flexibility before an active return
to running.
Finally, I always discourage the use of pharmaceutical anti- inflammatories. Not
only do they greatly aggravate the intestines, they suggest an artificial wellness
that can lead to bigger problems. Proteolytic enzymes, such as bromelain, are both
natural and extremely beneficial with no side effects. For more information, visit
your health food store or check out Rehab Plus on our website.
For further information, Dr. Maggs can be reached at (518) 869-1884, his Web site:
Dr. Maggs or via e-mail Running Doctor
=============================================================================
lose the back pain Link
Sciatica (Sciatic Pain, Piriformis Syndrome)
=============================================================================
Sciatica commonly refers to pain that radiates along the sciatic nerve and is
typically felt in the buttocks, down the back of the leg and possibly to the
foot. Sciatica is one of the most common forms of pain caused by compression
of the spinal nerves. Often the leg pain often feels much worse than the back
pain. Numbness, tingling, and a burning or prickling sensation in the back and
legs are also common symptoms.
Sciatica is actually a symptom and not disease. The term literally means that
a patient has pain down the leg from compression on the sciatic nerve. Usually
a herniated disc causes the sciatic pain. The diagnosis is what is causing
the compression (such as a disc herniation).
Most cases of sciatica are caused by a simple irritation to the nerve and will
get better with time. However, some sciatica symptoms may indicate a permanently
injured nerve. This is particularly if true weakness or numbness is present in
the back or the leg.
=============================================================================
syracusechargers.org
A Real Pain in the .... Link
=============================================================================
A while back I noted that very often I will be visited by a runner complaining
that his or her "sciatica is acting up." Generally, what they are saying is
they have some pain in the back of the thigh, maybe some in the buttock, low
back or even into the calf. Sciatica, by definition, is an inflammation or
irritation of the sciatic nerve, the largest nerve in the body, which originates
in the lower spine in the form of five separate nerve roots which join together
and traverse the buttock and descend into the lower limb all the way to the toes.
The problem is, sciatica is a vague term that doesn't really tell us very much
about the underlying reason for these symptoms since there can be several
explanations for them.
Some of the possible causes of this ailment which reviewed then included
sacroiliac joint dysfunction, lumbar spine arthritis or herniated discs, chronic
hamstring strains and a rather esoteric-sounding problem called the piriformis
syndrome, which we want to look at in more detail now.
The piriformis muscle is a relatively large structure found in the buttock,
originating on the sacrum (the lower part of the spine, or tailbone) and
crossing over at a slightly downward angle to the outside of the hip, attaching
to the outer portion of the upper thighbone (femur). Its function is to laterally
rotate and extend the hip joint. It is only one of several muscles in the buttock
which, as we've said, is an area through which the sciatic nerve passes, but the
piriformis has been singled-out as a potential cause of sciatica because anatomists
have found that in a fair number of people, all or part of the sciatic nerve
goes directly through this particular muscle. (The exact percentage of people
is unknown -- studies vary widely with some experts reporting 20% and others
as many as 60%!)
The speculation is that in these subjects, a tight piriformis muscle will
"squeeze" the nerve, causing irritation and subsequent pain. Runners, of course,
would be more likely to have a tight piriformis since they would be using it
more often and more intensely, especially during the push-off phase of gait when
hip extension and lateral rotation are needed most, but theoretically anyone
could experience this problem really if posture and biomechanics of walking
are abnormal.
Is it real? Does piriformis syndrome really exist? Well, the fact that we call
it a syndrome -- which in the medical field is a code word for "we don't really
know exactly what it is or know for sure what really causes it" -- tells us a lot.
It seems reasonable that the piriformis, like any muscle, can become overused
and painful, especially with running. But, like any muscle, this irritated muscle
can cause radiating or referred symptoms which would mimic sciatica pain while
there may not necessarily be any actual injury to the nerve itself. Or, conversely,
there are other potential causes of nerve inflammation in the buttock with no
involvement of the piriformis muscle. My favorite example is something actually
designated in the medical literature as "fat wallet syndrome," which is found most
often in long-distance drivers (truckers, salesmen). The prolonged pressure of a
billfold full of cash and credit-cards on the sciatic nerve is a not-infrequent
cause of sciatica. (The cure, of course, is for me to relief the patient of the
offending object...)
==============================================================================
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain
The Trigger Point Therapy Workbook;
You're Self-Treatment Guide for Pain Relief
Buy this book,, "The Trigger Point Therapy Workbook: Your Self-Treatment
Guide for Pain Relief" : Link
The Book Introduction Link
==============================================================================
They've tried chiropractic, acupuncture, magnets, pain diets, and herbal therapy.
They take their pain medicine and dutifully do their stretching exercises. Sometimes
they feel better for a while, but the pain always comes back. Nothing really seems
to get to the bottom of the problem. Despite being told there are no guarantees
of success, they fear surgery may be the only solution. They're beginning to wonder
if anybody really knows anything about pain.
If all this describes your own situation or that of someone you care about, this
book may provide the help you've been seeking. It proposes to give you a sensible
explanation of what's wrong and help you find the real cause of your pain. Even
better, it may well show you how to get rid of the pain yourself, hands-on. No
doctors. No pills. No bills.
There is growing evidence that most of our common aches and pains--and many
other puzzling physical complaints--are actually caused by trigger points, or
small contraction knots, in the muscles of the body. Pain clinic doctors skilled
at detecting and treating trigger points have found that they're the primary cause
of pain roughly seventy-five percent of the time and are at least a part of virtually
every pain problem. Even fibromyalgia, which is known to afflict millions of people,
is thought in many instances to have its beginning with trigger points.
Trigger points are known to cause headaches, neck and jaw pain, low back pain, the
symptoms of carpal tunnel syndrome, and many kinds of joint pain mistakenly ascribed
to arthritis, tendonitis, bursitis, or ligament injury. Trigger points cause problems
as diverse as earaches, dizziness, nausea, heartburn, false heart pain, heart
arrhythmia,
tennis elbow and genital pain. Trigger points can also cause colic in babies and bed-
wetting in older children and may be a contributing cause of such childhood horrors as
scoliosis, attention deficit disorder and dyslexia. They are a cause of sinus pain and
congestion. They may play a part in chronic fatigue and lowered resistance to infection.
And because trigger points can be responsible for long-term pain and disability that
seem to have no means of relief, they can cause depression.
The problems trigger points cause can be surprisingly easy to fix; in fact most people
can do it themselves if they have the right information. That's good, because the time
has come for ordinary people to take things into their own hands. The reason is that an
appallingly high percentage of doctors and other practitioners are still pretty much
out of the loop regarding trigger points, despite their having been written about in
medical journals for over sixty years. There has been, and continues to be, great
resistance to the whole idea.
Why has the medical profession not embraced the idea of trigger points? Partly, it's
because trigger points are commonly confused with acupressure points. Acupressure,
which has come down to us from ancient Chinese medicine, is alleged to have a positive
effect on supposed flows of energy throughout the body. Although acupressure and
other Eastern methods of healing do seem to have a beneficial effect, they're very
resistant to solid scientific investigation and are viewed by many doctors and a large
segment of the public as quack medicine with no proven results. If you don't know the
difference, the claims about trigger points sound like quack medicine too.
Our knowledge of trigger points, however, comes right out of Western medical research.
Trigger points are real. They can be felt with the fingers. They emit distinctive
electrical signals that can be measured by sensitive electronic equipment. Trigger
points have also been photographed in muscle tissue with the aid of the electron
microscope.
Most of what is known about trigger points is very well documented in the two-volume
medical text Myofascial Pain and Dysfunction: The Trigger Point Manual, by Janet Travell
and David Simons. These books tell virtually all there is to know about trigger points,
and the prospects for pain relief are very exciting. Much of the information in the
Trigger Point Manual is couched in difficult scientific terms but basic trigger point
science isn't hard to grasp if it's put into everyday language.
Travell and Simons describe a trigger point as simply a small contraction knot in muscle
tissue. It often feels like a partly cooked piece of macaroni or like a pea buried deep
in the muscle. A trigger point affects a muscle by keeping it both tight and weak. At
the same time, a trigger point maintains a hard contraction on the muscle fibers that
are directly connected to it. In turn, these taut bands of muscle fiber keep constant
tension on the muscle's attachments, often producing symptoms in adjacent joints. The
constant tension in the fibers of the trigger point itself restricts circulation in its
immediate area. The resulting accumulation of the by-products of metabolism, as well as
deprivation of the oxygen and nutrients needed for metabolism can perpetuate trigger points
for months, or even years, unless some intervention occurs. It's this self-sustaining
vicious cycle that needs to be broken.
The difficulty in treating trigger points is that they typically send pain to some other
site. Most conventional treatment of pain is based on the assumption that the cause of
pain will be found at the site of the pain. But trigger points almost always send their
pain elsewhere. This referred pain is what has always thrown everybody off, including
most doctors and much of the rest of the health-care community. According to Travell
and Simons, conventional treatments for pain so often fail because they focus on the
pain itself, treating the site of the pain, and overlooking and failing to treat the
cause, which may be some distance away.
Even worse than routinely treating the site of the pain is the pharmaceutical treatment
of the whole body for what is usually a local problem. Painkilling drugs, the increasingly
expensive treatment of choice these days, give us the illusion that something good is
happening, when in reality they only mask the problem. Most common pain, like headaches,
muscle aches, and joint pain, is a warning-a protective response to muscle overuse or
trauma. Pain is telling you that something is wrong and needs correction. It's not good
medicine to kill the messenger and ignore the message. When pain is seen in its true role
as the messenger and not the affliction itself, treatment can be directed to the cause
of pain.
Luckily, referred pain is now known to occur in predictable patterns. The valuable medical
advance made by Travell and Simons and their brilliant illustrator, Barbara Cummings,
has been in delineating these very patterns. Once you know where to look, trigger points
are easily located by touch and deactivated by any of several methods.
Unfortunately, the two clinically oriented methods put forth in The Trigger Point Manual
don't lend themselves to self-treatment. The goal of this book is to build on the work of
Travell and Simons and provide a more practical and cost-effective approach to pain
therapy: a classic do-it-yourself approach, rather than multiple professional office
visits. This new approach is a system of self-applied massage directed specifically at
trigger points. Significant relief of symptoms often comes in just minutes. Most problems
can be eliminated within three to ten days. Even long-standing chronic conditions can be
cleared up in as little as six weeks. Results may be longer in coming for those who
suffer from fibromyalgia, chronic fatigue, or widespread myofascial pain syndrome, but
even they can experience continuing progress and can have genuine hope of significant
improvement in their condition.
Self-applied trigger point massage works by accomplishing three things: it breaks into the
chemical and neurological feedback loop that maintains the myofascial contraction; it
increases circulation that has been restricted by the contracted tissue; and it directly
stretches the trigger point's knotted muscle fibers. The illustrations in this book show
you how to find the trigger points that are generating your specific problems, as well
as the exact hands-on techniques for deactivating them. Special attention has been given
to designing methods of massage that do no damage to hands that may already be in trouble
from overuse.
This book's primary use is as a self-instruction manual, but it can also be used as a
textbook for classroom use. This simplified and direct approach to treating myofascial
pain with self-applied massage can constitute a foundational course in trigger point
therapy in any professional training curriculum. Students in chiropractic colleges,
physical therapy departments, and massage schools will derive particular benefit. If
they can learn how to interpret their own referred pain and how to find and treat their
own trigger points, they will know exactly what to do when they encounter similar
problems in their future clients.
A class in self-applied trigger point massage would be a boon in medical schools for
exactly the same reasons. When new doctors can learn how to fix their own pain with
self-applied massage, they are in better touch with the realities of pain and with the
great potential in the treatment of trigger points. Such an addition to medical education
would profoundly improve the treatment of pain and lower much of its cost.
And it's not too late for physicians already in practice to learn about trigger points
and myofascial pain and put the knowledge to good use. They will find this book a quick
and practical introduction to the magnificent work of Travell and Simons and this
neglected branch of medicine. Hopefully, many will be encouraged to go to Travell and
Simons' Trigger Point Manual for a deeper scientific understanding and for even greater
benefit to their practice. A large segment of the public needs help and encouragement
in learning how to deal with their trigger point-induced pain. No one is better positioned
to provide this help than the medical community.
The medical profession is not unaware of the deficiencies of current methods of treating
pain. Doctors hurt too. Many of them worry like the rest of us about the relentless popping
of pills, and many experience frustration with their inability to offer better solutions
to their patients. Trigger point therapy, whether self-applied or administered by a
professional, has the potential to truly revolutionize pain treatment throughout the
world.
=============================================================================
Sciatica, Piriformis Syndrome, PIRIFORMIS TRIGGER POINTS Link
Sciatic Nerve Impingement, Erectile Dysfunction,
Buttocks Pain, Rectal Pain, Anal Pain,
Leg Pain, Tingling in Legs
According to Doctors Janet Travell and David Simons in their widely acclaimed medical
textbook, Myofascial Pain and Dysfunction: The Trigger Point Manual, myofascial
trigger points (tiny contraction knots) in overworked gluteus minimus and piriformis
muscles in the buttocks are actually the most frequent cause of sciatica.
Referred Symptoms
Symptoms of sciatica include aching pain, numbness, tingling, burning and
hypersensitivity in your low back, buttocks, hips, and down your legs into your
ankles and feet. Simple aching pain in these areas usually is referred from gluteus
minimus trigger points.
Piriformis trigger points, by keeping the muscles tight and rock hard, can cause
actual sciatic nerve compression. Pain from piriformis trigger points is harsher
and more electric than pain from gluteus minimus trigger points and is felt in
the back of the thigh, the calf, and the sole of the foot. There may also be other
abnormal sensations, such as numbness, tingling, burning, or hypersensitivity,
in any of these areas.
Piriformis Syndrome
A piriformis muscle that is shortened and swollen by trigger points can also
compress numerous other nerves and blood vessels coming out of the pelvis. This
can result in a sense of swelling in the buttocks, leg, calf, and foot. In addition,
a tight piriformis muscle can impinge upon the pudendal nerve, causing impotence
in males and pain in the groin, genitals, or rectal area of either gender.
Piriformis muscles that compress gluteal nerves and blood vessels are believed
to be responsible for gluteal muscle atrophy, wherein one or both buttocks waste
away.
For decades, the medical profession has known this particular group of sciatic
symptoms as "piriformis syndrome," although the cause of the piriformis enlargement
was never really understood. Surgical release of the piriformis muscle for the
treatment of sciatica was once a common treatment. Amazingly, this operation is
still performed by surgeons who are unaware of the effects of myofascial trigger
points.
Misdiagnosis:
In the medical world, sciatica is routinely assumed to be caused by pressure on
the sciatic nerve as a result of a compressed disk or other spinal abnormality.
Surgery on the spine in a search for the cause of presumed sciatic nerve impingement
is very common, even though it regularly fails to erase sciatic symptoms.
Doctors Travell and Simons believe that traditional medical solutions for sciatica
and piriformis syndrome is needlessly expensive and have an unacceptably high rate
of failure. Trigger points should be at the top of the list during any examination
for pain, numbness and other abnormal sensations in the hips and legs. Wider recognition
of the myofascial causes of sciatica could eliminate many unnecessary surgical
operations.
Self-Treatment: Myofascial Pain and Dysfunction: The Trigger Point Manual
You don't have to wait for the medical community to abandon antiquated methods and
catch up with trigger point science. You can take care of your own trigger points.
In The Trigger Point Therapy Workbook, nationally certified massage therapist Clair
Davies has simplified Travell and Simons' extensive research into myofascial pain
and made it accessible to the layman. His innovative methods of self-applied trigger
point massage will get rid of the numbness, tingling and aching pain of sciatica
and piriformis syndrome when trigger points are the cause. To learn more, please
visit the homepage.
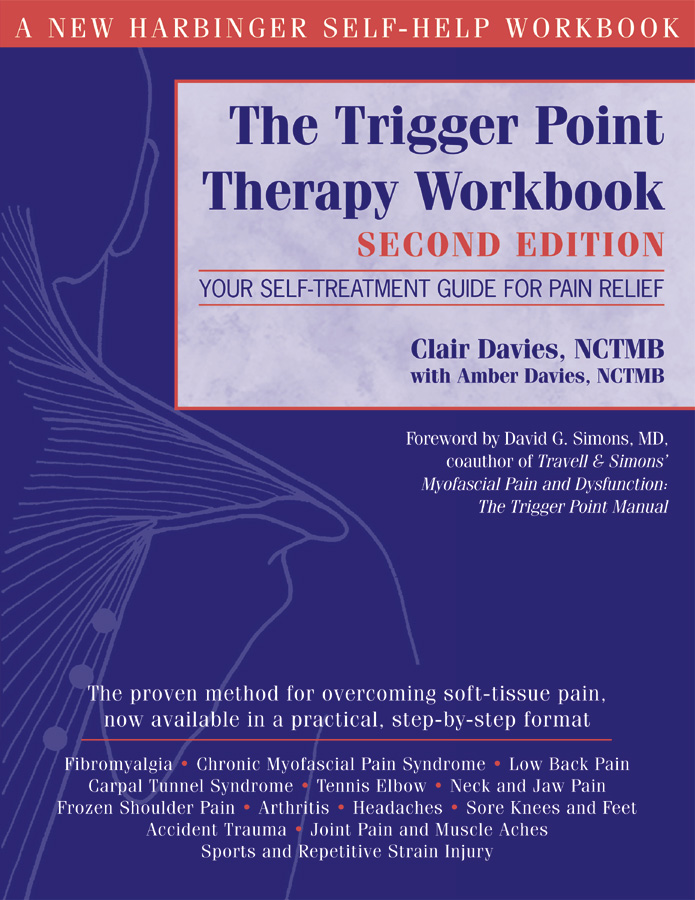 trigger point therapy book - buy yours today!
The Trigger Point Therapy Workbook - Second Edition
You're Self-Treatment Guide For Pain Relief
Clair Davies www.triggerpointbook.com, NCTMB
with Amber Davies, NCTMB
The proven method for over-coming soft tissue pain. Now available in a practical
step by step format.
===========================================
TRIGGER POINT THERAPY CHAPTER 1 Link
============================================
It was a spark of hope.
A New Technology
When I got home from the convention, I ordered the books: volumes I and II of
Myofascial Pain and Dysfunction: The Trigger Point Manual, by Janet Travell and
David Simons. The price of medical books was a shock and I bridled a bit, but I
finally had to ask myself: What is this knowledge worth? My shoulder answered
the question for me.
When the books came, I entered a world I hadn't known existed. As soon as I began t
read, the mystery of my shoulder problem began to clear. In the Trigger Point Manual,
I found hundreds of beautifully executed illustrations of the muscles of the body.
They showed the likely trigger points for every muscle and the patterns of pain they
predictably touched off.
I found that, although the physiology of a trigger point was extremely complex,
a trigger point for practical purposes could be viewed as what most people call
a "knot": a wad of muscle fibers staying in a hard contraction, never relaxing.
A trigger point in a muscle could be actively painful or it could manifest no pain
at all unless touched. More often, though, it would sneakily send its pain somewhere
else. I gathered that much of my pain, perhaps all of it, was probably this mysterious
displaced pain, this referred pain. I had never been able to figure out why all the
rubbing I had been doing had never done any good. It was a mistake to assume the
problem was at the place that hurt!
The pain in the front of my shoulder was actually coming from behind it, from trigger
points in the infraspinatus, a muscle that covered part of the outside of my shoulder
blade. The deep aching behind my shoulder was coming from trigger points in the
subscapularis, a muscle on the underside of my shoulder blade, sandwiched between
the shoulder blade and the ribs. The unrelenting pain at the inner edge of my shoulder
blade was being sent by trigger points in the scalene muscles, in the front and sides
of my neck. It was no wonder nobody knew what to do for me!
It was clear to me that all I had was a massive number of trigger points in the muscle
in my shoulder-trigger points in over twenty muscles, as it turned out. That first
massage therapist, the one I liked so much, had treated me very successfully with
ordinary massage techniques and I understood now that it was trigger points she was
dealing with. Perhaps I could deal with the trigger points myself using massage. I
began to think that this might be a job for someone with a technician's mentality-maybe
someone who was smart enough to take on the complexities of a piano would be well
equipped to fix trigger points.
Driven by my misery and by my excitement about these new ideas, I studied Travell
and Simons night and day. I found that my trigger points would yield under the touch
of my own hands if I persisted. After only about a month of assiduously applying
what I was learning chapter by chapter, I had succeeded in fixing my shoulder . . .
my own shoulder! I was astounded. The pain was gone. I could raise my arm. I could
sleep through the night. This stuff really worked!
Given the innately optimistic cast of my mind, I immediately took a larger view.
I saw that I had in my hands the tools to take effective care of myself, at least
when it came to any kind of myofascial pain. I supposed that I might be able to
treat any trigger point I could reach and extinguish virtually any pain I might
have. I could develop a complete system, a kind of new technology, and maybe other
people would be helped by it.
Mechanical Ingenuity
Travell and Simons had done a wonderful thing in giving the science of myofascial
pain to the medical community. The illustrations by Barbara Cummings brilliantly
clarified every aspect of the subject. Without these dedicated people, the science
of trigger points and referred pain would still be an impossible jumble, largely
unknown and inaccessible.
Unfortunately, Travell and Simons' two main methods for deactivating trigger points
weren't oriented toward self-treatment. They were designed specifically for the
doctor's office or the physical therapy clinic: a doctor could inject trigger points
with procaine, a local anesthetic; and a physical therapist could presumably stretch
trigger points out of existence. It bothered me, however, that the physical therapy
protocol, which Travell and Simons called their "workhorse" method, involved the muscle
stretching that I had found so ineffective and even dangerous, in that it had made
my shoulder problem dramatically worse. To be sure, Travell and Simons had made
stretching safer by using a refrigerant spray on the skin. "Distracting" the nervous
system with the spray meant the underlying muscles were less likely to tighten up
in defense. Nevertheless, safe or not, I felt that the spray and stretch method was
too elaborate to be practical for self-treatment, and that it would be impossible
to use on areas that were hard to reach.
Trying to get at the relatively small trigger points by stretching whole groups of
recalcitrant muscles seemed unnecessarily indirect and inefficient. The problem was
not with the generalized tension in the muscle, but rather with the trigger point,
a very specific, circumscribed place within the muscle. The trigger point's knotted
up muscle fibers obviously needed to relax and let go, but why not go straight to
the trouble spot and deal with it directly? Massage seemed to me the natural approach,
and it obviously worked with trigger points-that good massage therapist had proven
that much to me.
I wanted to find simple ways to use massage for self-treatment. I wanted to develop
a comprehensive method for dealing with trigger points anywhere in the body. I
wanted something that a regular person like me could immediately understand and
use. I was sure all this could be done.
Among the old-time piano men at Steinway, the highest compliment was to be called
"a pretty good mechanic." A good mechanic cared about the details and he stuck
with the job until he got it right; he could find the solution to a problem even
if it wasn't in the book. My life up to that point had been built around being
a good mechanic, and being able to find the simple solution. That's certainly
what I had to do in devising ways to self-treat trigger points. For the purposes
of treating trigger points, I felt the body was best thought of as a machine,
a mechanical system of levers, fulcrums and forces, especially in regard to the
bones and muscles. I could understand such a system. A lifetime of working with
my hands was about to begin to pay off in a new and unexpected way.
My first challenge was to learn the exact location of each muscle, to visualize
how it attached to the bones, and to understand the job the muscle did. Finding
the precise massage technique that a trigger point would respond to was where the
art would come in. The difficulty here was in figuring out how to reach unreachable
places and get effective leverage in awkward positions without hurting my hands
and fingers, which were already being overused in the course of an ordinary workday.
The project became an obsession. I studied Travell and Simons the first thing in
the morning and the last thing at night. I studied in the parking lot at McDonald's.
Using my own body as the laboratory, I discovered something new every day. I found
trigger points everywhere and became aware of pain that I didn't know I had. I only
wanted to talk about trigger points and often greeted family members excitedly with the
exclamation, "I found another one! I found another one!" Over a period of three
years, I learned how to find and deactivate trigger points in 120 pairs of muscles,
which enabled me to cope with every trigger point that Travell and Simons dealt
with in their books except those inside the pelvis.
A World of Pain
The misdiagnosis of pain is the most important issue taken up by Travell and Simons.
Referred pain from trigger points mimics the symptoms of a very long list of common
maladies; physicians, in weighing all the possible causes for a given condition,
have rarely even conceived of there being a myofascial source. The study of trigger
points has not historically been a part of medical education. Travell and Simons
hold that most of common everyday pain is caused by myofascial trigger points and
that ignorance of that basic concept could inevitably lead to false diagnoses and
the ultimate failure to deal effectively with pain. (Travell and Simons 1999: 12-14)
From the beginning, I had a sense that for some reason the great work of Janet Travell
and David Simons had fallen into a deep pit and was in danger of being buried and
forgotten. Surely, by now Travell's discoveries about pain should have swept the
country and changed the world of health care. The first volume of the Trigger Point
Manual had been published in 1983, but I couldn't find anything about trigger points
in the public library. None of the popular family medical guides even mentioned
trigger points. Nothing truly informative was to be found in bookstores. Doctors
were still using drugs as the primary treatment for pain. Many were actively hostile
to the concept of trigger points, discounting the idea as just more bogus medicine,
something purely imaginary.
Only massage therapists seemed to be informed about trigger points and referred pain,
and only exceptional individuals among them (in my own experience at least) were
treating trigger points effectively. What's more, the burgeoning variety of unproven
modalities offered by massage therapists gave the profession such an aura of flakiness
that the elegant science of myofascial pain treatment got unfairly confused with
treatments whose results could easily be attributed to the placebo effect. With
such an identity, how could the medical profession or the public at large ever take
it seriously?
Clearly, there was a world of pain out there in need of the simple and genuine
solutions I felt I had in hand. I despaired of doctors ever listening to me about
trigger point therapy. Taking the facts about myofascial pain directly to the public
seemed the more logical tack. I began to think about leaving the piano business
behind. There was something more important for me to do.
The first thing I wanted to do was to write about the self-treatment of pain for all
my ailing friends in the Piano Technicians Guild. Previous articles in the Piano
Technicians Journal had given me a following. I guessed that my ideas about pain
had a better chance of publication in this journal than almost anywhere else.
I also conceived of giving seminars and workshops about the self-treatment of pain,
and I thought that getting a massage school diploma might give me more credibility.
But I had an even better motive for going to massage school. My daughter Amber had
had chronic back pain ever since lifting a heavy chair during a scene change while
she was working in Summer Theater. Employing my new knowledge about trigger points,
I'd been trying to give her massage, but I just wasn't very good. I didn't know the
time-tested manual techniques used by massage therapists. It would be worth learning
to do massage right, if only to help my daughter; and anything I learned that benefited
my method of self-treatment would be a plus.
I applied to the biggest massage school I could find, one with a busy, well-managed
student clinic where I could get a great deal of experience in the shortest time
possible. At that moment, I couldn't imagine becoming a professional therapist, but
I definitely wanted the skills. With the help of my son-in-law, who I had trained
to take over my piano business, I plowed through a backlog of half a dozen rebuilding
jobs. We cleared my calendar in time for me to start a six-month clinical course
at the Utah College of Massage Therapy.
Massage School
There were forty-nine of us in the class: thirty-six women and thirteen men. We were
a greatly varied group of all backgrounds, from many states and foreign counties, and
ranging in age from seventeen to sixty. It soon became apparent that, although I was
the oldest in the class (and possibly prejudged by most of the others to be a creaking
fuddy-duddy), I was the only one who could claim to be free of pain. All the others
-young and old, male and female-had some kind of enduring problem with pain. I found
that it was almost a cliché that people go to massage school because they have chronic
pain and they're looking for the solution they haven't found elsewhere.
It seemed ironic to me that I arrived in Utah having read both volumes of Travell
and Simons' Trigger Point Manual and having gone a long way toward developing my
method of self-healing, yet I couldn't get anyone to listen. I had just left a
business where my word was taken as gospel. I had disciples. In the role of student,
my accustomed authority was reduced to nil. Nobody wanted to hear what I knew about
trigger points. I could only stand and watch as a fellow student would have a pain
crisis, usually bad neck pain or a back spasm, and run off to a chiropractor or to
the emergency room. I kept offering help and being turned down.
It was even harder to approach the instructors about do-it-yourself massage, but
the anatomy teacher apparently felt less threatened than the others. He was a big,
self-confident guy with a great sense of humor, who didn't fear losing his authority
with the students. During a break one day, he heard me talking to a classmate about
trigger points and asked if I knew how to fix pain. He said he often had pain that
shot diagonally across one side of his chest. He was having it again just that morning.
It wasn't his heart, he said; he'd had it checked. While he explained, I reached up
and began pressing on his neck just above his collarbone. He suddenly stopped talking
and winced, then exclaimed, "Hey, that's it! That's my pain! How did you do that?"
A trigger point in a scalene muscle was causing the pain in his chest. I showed him
how to work the trigger point himself and he told me later that the pain had gone
away and hadn't come back.
I couldn't get over it. This man was a registered nurse and a gifted teacher of
anatomy that knew his muscles but didn't know about his own trigger points. He was
a product of the same system that turns out physicians with the same astounding gap
in their knowledge.
After my classmates saw me go hands-on with our anatomy teacher's trigger points,
they began letting me show them some of my tricks. I showed one student how to kill
her sinus pain by working on her jaw muscles, another how to stop his feet from
hurting by massaging his calves, and another how to get rid of her dizzy spells
with attention to trigger points in the front of her neck. Several eventually came
to me for back pain of various kinds. Near the end of the course, I got to show the
whole class my techniques for getting rid of arm and hand pain, something we all
experienced working in the clinic. Several classes of budding massage therapists
worked in the weekend clinic where it was not unusual for us to give 1200 massages
on a Saturday and Sunday.
I saw the same pain patterns in the clinic that I had seen with my fellow students:
lots of back trouble, plus a broad selection of every other kind of pain you could
think of. I saw pain in every part of the body and every joint: shoulders, elbows,
wrists, knuckles, hips, knees, and ankles. Typically, the client had already been
the rounds of doctors, chiropractors, physical therapists, and so on, looking for
the magician in the white coat. They'd tried yoga, magnets, and pain diets, herbal
therapies, and acupuncture. Some had had their problem for ten years and more.
Many guessed they were just getting arthritis and so were habitually popping pills
They felt older than their years, handicapped by pain. They felt their careers
in danger. Depression due to constant pain was a prevailing theme.
It was exasperating to hear the same stories repeatedly, to know both how simple
their problems were and just what to do for them, and to know many clients were
coming for massage only as a last resort. In my view, massage is the only thing
that works for these kinds of pain, and should be the first thing tried, not the
last. I consistently found trigger points to be the cause of my clients' problems,
and clients nearly always got off my table feeling better. Many left my booth
feeling they'd finally found something that worked. I felt more and more that
I also had found something that worked. I liked giving massage a great deal-I
was surprised at how much. I asked for extra shifts and accumulated twice as
many hours as were required.
Until I was working regularly in clinic, I hadn't seen that giving massage to
others were a way of taking care of me. I'd only been thinking of getting a
diploma from a good school so I would have a bit of credibility when I went on
to teach self-massage. Unexpectedly, I got as much from the massages as my clients
did, maybe more. I felt myself becoming kinder and more empathic. Knowing how to
take care of my own pain had made me more fit for taking care of others, which
made me more fit for taking care of myself. My six months at the Utah College
of Massage Therapy was transformational. I regretted I hadn't done it sooner.
Recurrent Themes
While in massage school I finished writing my series of eight articles on self-applied
trigger point massage for the Piano Technicians Journal. Publication began two months
after I graduated. When the first article appeared, desperate piano tuners began
calling me for advice from all over the United States and Canada. They didn't want
to wait until the article on their particular problem came out. Many were on the
verge of quitting piano work because of chronic pain. Some had been in pain for
as long as twenty years, repeatedly going the rounds of the health-care community
just like I had, with the same frustrating results.
One tuner from New England had been afflicted with severe recurrent pain in both
knees since climbing Mount Katahdin, the highest point in Maine, twelve years
earlier. The pain had started as he descended the mountain and his friends had
had to carry him most of the way to the bottom. Now he couldn't even go out and
mow his lawn without being crippled for days by the effort. Working with me over
the phone, he was able to find and massage the horribly painful trigger points in
his thigh muscles that were causing the pain in his knees. Before we hung up, the
pain was gone. There had been no way for him to know that his trouble was not in
his knees but in his thigh muscles, strained by the unaccustomed mountain climbing:
his doctors, physical therapists, and chiropractors hadn't known. At the Piano
Technicians Guild National Convention a couple of months later, he happily told
me he'd continued working on his trigger points and hadn't had any more trouble
with his knees. I was as pleased as he was.
I was scheduled to give a workshop on the self-treatment of pain at that convention
and was worried that nobody would come. From the number of sufferers who had called
me on the phone, I should've known better. One hundred and ten people showed up,
and it was standing room only in the modest-sized meeting room. I knew at least
one thing about every person in the room before we even began: they all hurt.
Piano technicians are the most diverse, intelligent, creative group of people I've
ever had the privilege to know, and at the same time they're the most assertively
independent. Some literally would rather die than ask for help. If I could tell
them something about the treatment of pain that they could do themselves, they
wanted to hear it. They were all in such need that no one so much as looked away
throughout the whole program. I was very encouraged.
That was the first convention I went to not as a piano tuner, but as a massage
therapist. I didn't go to classes at all that week. I didn't go to committee
meetings. I didn't even party at night. I had something better to do. I spent
every day, from eight in the morning until ten at night, troubleshooting trigger
points and giving massage, only leaving my room to get a quick meal. They weren't
all piano tuners who came to me; spouses needed help too. Although there were some
recurrent themes, like shoulder pain, they brought me all kinds of problems-back
pain, neck pain, headaches, numb hands-just like in the massage school clinic.
People at the convention had come from all over North America, even from several
foreign countries. No matter where these people lived, they all had the same story:
they'd had trouble getting effective treatment. Nobody seemed to know what caused
their pain and nobody could help.
Back in Kentucky, as I began my private practice, again I saw all the by now
familiar patterns. All the people who came for massage had already been to a
physician or a pain clinic. Almost all had experimented with chiropractic. Many
had been to the emergency room for their pain. Most had been through physical
therapy. They had tried everything, including various forms of alternative medicine.
Some had even tried massage but hadn't been impressed. It had been "feel-good"
massage: it had been relaxing but hadn't put a dent in their pain.
Interestingly, almost all the people who came to me had some kind of back pain
along with whatever other pain complaint they had. Their previous treatments for
back pain had always focused on the spine. I heard about injections of papaya or
cortisone. People had usually been told they had arthritis or bad disks, or that
their cartilage had been worn away. They'd been shown X-rays that purported to
prove it. One woman was on her doctor's schedule to have her vertebrae fused. Some
had already had surgery, and frequently had as much pain after surgery as before.
Typically, the surgeon's last word was always that he was sorry but he'd done all
he could. Then he'd renew their prescription for painkillers and dump them off on
a physical therapist. I heard these stories over and over again. And over and over,
I found that trigger point therapy gave them the relief they'd been seeking for so
long. Had trigger points been the problem in the first place? Arthritis? Bad disks?
In Travell and Simons' Trigger Point Manual, I had read that you can have herniated
disks and arthritis of the spine and still find that myofascial trigger points are
the primary cause of your back pain.
One client said her doctor confided sympathetically that he had back pain too. He
wore magnets under his clothing just like she did. Many of my clients had tried
magnets and were often a little embarrassed to say so. Yes, the magnets did seem
to help, they said, but the pain always came back. It was the same with TENS units:
when you took them off, you still had your problem. (A transcutaneous electrical
nerve stimulation [TENS] unit gives you little shocks that interfere with pain
signals, but has no effect on the cause of the pain.)
Nearly everyone I treated was on pain medication of some kind, although few had
the illusion that painkillers were a real cure. People seem to know intuitively
that throwing a cloak over the pain only keeps you from seeing the real problem.
When you hide the problem, you never get the opportunity to address it. Looked at
in this way, painkillers actually perpetuate pain. People want real solutions;
they don't want to dope the problem away.
Another common theme among the people who came to me was numbness and pain in the
hands and fingers. I began to get the impression that the computer keyboard was
crippling the country. I saw wrist braces of all kinds. A doctor had wanted to
put one woman's wrists in casts to heal her numb hands. While many clients feared
they had carpal tunnel syndrome or had even been given the diagnosis, massage of
trigger point in the forearms, shoulder, and neck always took the pain and numbness
away. This outcome was usually a surprise to the client. It soon ceased to be a
surprise to me. Good results were so consistent with "carpal tunnel" symptoms that
I began to wonder whether true carpal tunnel syndrome really existed.
What did all this mean for me? I knew how to help myself and it was clear I
could help other people, but what was the best use of my newfound skills? There
was indeed a world of pain out there, but I'd started too late as a massage
therapist to hope to help very many people one on one. At my age, I wasn't going
to have a long career as a healer. What could I do for the world of pain with
the time and energy I had left? It became increasingly clear that I had to write
a book about trigger point therapy and get this information out to as many
people as possible.
Casting a Wider Net
A doctor should have written this book. It should've been written by a bona
fide, credentialed expert in a white coat with years and years of experience
and scores of articles published in medical journals. If "M.D." followed my name
on the cover of this book, I wouldn't have had to write this chapter. This chapter
is meant to give you some reason to trust what I have to say about pain, some
reason to suspend your disbelief long enough to give my methods a fair try. The
best evidence of whether my method is a good one for you will come from your own
personal experience with it. Trying it is the only way you can truly validate my
claims about its success.
I don't claim to be an authority on pain. Travell and Simons are the pain experts.
In writing this book, my job has primarily been to put their vast knowledge into
more understandable form and transmit it to you. Having figured out how to fix my
own pain counts for something, though. Being a massage therapist counts too, because
I've proven to myself and to my clients that I know how to fix pain for other people.
I thought you might be interested in my shoulder story. I thought you might be
interested in how the wisdom of Janet Travell and David Simons got me through my
difficulties and how they truly gave me a new life. From my success in defeating
pain, I thought you might gain a smidgen of hope: my new life offering the possibility
of a new life for you. My own hope is that this book will be a useful one. It's
you who will prove me right or wrong.
=============================================================================
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain Link
Self-Treatment Examples from
The Trigger Point Therapy Workbook
Original Doctors who found these techniques: Doctors Janet Travell and David Simons
=============================================================================
This is a splendid self-help book for people with persistent musculoskeletal
pain. It tells you how to identify the problem and carefully guides you
through the process of self-treatment. The principles of treating myofascial
pain and myofascial trigger points developed by Doctors Janet Travell and
David Simons form the basis of this book, and are well presented for use
by individuals with pain." Link
--ROBERT D. GERWIN, M.D., Neurologist, Assistant Professor, Johns Hopkin
s School of Medicine; author, Myofascial Pain: An Integrated Approach to
Diagnosis and Treatment (video series)
=============================================================================
Low Back Pain
The reason there are so many differing opinions about the cause of back pain
is that it's mostly referred pain. You may never find back pain's real cause
if you look for it only in the back muscles or the spine. Back pain very often
comes from trigger points in stomach muscles, for instance. The illustration
shows a gluteus medius trigger point that is one of the most common causes of
low back pain:
trigger point therapy book - buy yours today!
The Trigger Point Therapy Workbook - Second Edition
You're Self-Treatment Guide For Pain Relief
Clair Davies www.triggerpointbook.com, NCTMB
with Amber Davies, NCTMB
The proven method for over-coming soft tissue pain. Now available in a practical
step by step format.
===========================================
TRIGGER POINT THERAPY CHAPTER 1 Link
============================================
It was a spark of hope.
A New Technology
When I got home from the convention, I ordered the books: volumes I and II of
Myofascial Pain and Dysfunction: The Trigger Point Manual, by Janet Travell and
David Simons. The price of medical books was a shock and I bridled a bit, but I
finally had to ask myself: What is this knowledge worth? My shoulder answered
the question for me.
When the books came, I entered a world I hadn't known existed. As soon as I began t
read, the mystery of my shoulder problem began to clear. In the Trigger Point Manual,
I found hundreds of beautifully executed illustrations of the muscles of the body.
They showed the likely trigger points for every muscle and the patterns of pain they
predictably touched off.
I found that, although the physiology of a trigger point was extremely complex,
a trigger point for practical purposes could be viewed as what most people call
a "knot": a wad of muscle fibers staying in a hard contraction, never relaxing.
A trigger point in a muscle could be actively painful or it could manifest no pain
at all unless touched. More often, though, it would sneakily send its pain somewhere
else. I gathered that much of my pain, perhaps all of it, was probably this mysterious
displaced pain, this referred pain. I had never been able to figure out why all the
rubbing I had been doing had never done any good. It was a mistake to assume the
problem was at the place that hurt!
The pain in the front of my shoulder was actually coming from behind it, from trigger
points in the infraspinatus, a muscle that covered part of the outside of my shoulder
blade. The deep aching behind my shoulder was coming from trigger points in the
subscapularis, a muscle on the underside of my shoulder blade, sandwiched between
the shoulder blade and the ribs. The unrelenting pain at the inner edge of my shoulder
blade was being sent by trigger points in the scalene muscles, in the front and sides
of my neck. It was no wonder nobody knew what to do for me!
It was clear to me that all I had was a massive number of trigger points in the muscle
in my shoulder-trigger points in over twenty muscles, as it turned out. That first
massage therapist, the one I liked so much, had treated me very successfully with
ordinary massage techniques and I understood now that it was trigger points she was
dealing with. Perhaps I could deal with the trigger points myself using massage. I
began to think that this might be a job for someone with a technician's mentality-maybe
someone who was smart enough to take on the complexities of a piano would be well
equipped to fix trigger points.
Driven by my misery and by my excitement about these new ideas, I studied Travell
and Simons night and day. I found that my trigger points would yield under the touch
of my own hands if I persisted. After only about a month of assiduously applying
what I was learning chapter by chapter, I had succeeded in fixing my shoulder . . .
my own shoulder! I was astounded. The pain was gone. I could raise my arm. I could
sleep through the night. This stuff really worked!
Given the innately optimistic cast of my mind, I immediately took a larger view.
I saw that I had in my hands the tools to take effective care of myself, at least
when it came to any kind of myofascial pain. I supposed that I might be able to
treat any trigger point I could reach and extinguish virtually any pain I might
have. I could develop a complete system, a kind of new technology, and maybe other
people would be helped by it.
Mechanical Ingenuity
Travell and Simons had done a wonderful thing in giving the science of myofascial
pain to the medical community. The illustrations by Barbara Cummings brilliantly
clarified every aspect of the subject. Without these dedicated people, the science
of trigger points and referred pain would still be an impossible jumble, largely
unknown and inaccessible.
Unfortunately, Travell and Simons' two main methods for deactivating trigger points
weren't oriented toward self-treatment. They were designed specifically for the
doctor's office or the physical therapy clinic: a doctor could inject trigger points
with procaine, a local anesthetic; and a physical therapist could presumably stretch
trigger points out of existence. It bothered me, however, that the physical therapy
protocol, which Travell and Simons called their "workhorse" method, involved the muscle
stretching that I had found so ineffective and even dangerous, in that it had made
my shoulder problem dramatically worse. To be sure, Travell and Simons had made
stretching safer by using a refrigerant spray on the skin. "Distracting" the nervous
system with the spray meant the underlying muscles were less likely to tighten up
in defense. Nevertheless, safe or not, I felt that the spray and stretch method was
too elaborate to be practical for self-treatment, and that it would be impossible
to use on areas that were hard to reach.
Trying to get at the relatively small trigger points by stretching whole groups of
recalcitrant muscles seemed unnecessarily indirect and inefficient. The problem was
not with the generalized tension in the muscle, but rather with the trigger point,
a very specific, circumscribed place within the muscle. The trigger point's knotted
up muscle fibers obviously needed to relax and let go, but why not go straight to
the trouble spot and deal with it directly? Massage seemed to me the natural approach,
and it obviously worked with trigger points-that good massage therapist had proven
that much to me.
I wanted to find simple ways to use massage for self-treatment. I wanted to develop
a comprehensive method for dealing with trigger points anywhere in the body. I
wanted something that a regular person like me could immediately understand and
use. I was sure all this could be done.
Among the old-time piano men at Steinway, the highest compliment was to be called
"a pretty good mechanic." A good mechanic cared about the details and he stuck
with the job until he got it right; he could find the solution to a problem even
if it wasn't in the book. My life up to that point had been built around being
a good mechanic, and being able to find the simple solution. That's certainly
what I had to do in devising ways to self-treat trigger points. For the purposes
of treating trigger points, I felt the body was best thought of as a machine,
a mechanical system of levers, fulcrums and forces, especially in regard to the
bones and muscles. I could understand such a system. A lifetime of working with
my hands was about to begin to pay off in a new and unexpected way.
My first challenge was to learn the exact location of each muscle, to visualize
how it attached to the bones, and to understand the job the muscle did. Finding
the precise massage technique that a trigger point would respond to was where the
art would come in. The difficulty here was in figuring out how to reach unreachable
places and get effective leverage in awkward positions without hurting my hands
and fingers, which were already being overused in the course of an ordinary workday.
The project became an obsession. I studied Travell and Simons the first thing in
the morning and the last thing at night. I studied in the parking lot at McDonald's.
Using my own body as the laboratory, I discovered something new every day. I found
trigger points everywhere and became aware of pain that I didn't know I had. I only
wanted to talk about trigger points and often greeted family members excitedly with the
exclamation, "I found another one! I found another one!" Over a period of three
years, I learned how to find and deactivate trigger points in 120 pairs of muscles,
which enabled me to cope with every trigger point that Travell and Simons dealt
with in their books except those inside the pelvis.
A World of Pain
The misdiagnosis of pain is the most important issue taken up by Travell and Simons.
Referred pain from trigger points mimics the symptoms of a very long list of common
maladies; physicians, in weighing all the possible causes for a given condition,
have rarely even conceived of there being a myofascial source. The study of trigger
points has not historically been a part of medical education. Travell and Simons
hold that most of common everyday pain is caused by myofascial trigger points and
that ignorance of that basic concept could inevitably lead to false diagnoses and
the ultimate failure to deal effectively with pain. (Travell and Simons 1999: 12-14)
From the beginning, I had a sense that for some reason the great work of Janet Travell
and David Simons had fallen into a deep pit and was in danger of being buried and
forgotten. Surely, by now Travell's discoveries about pain should have swept the
country and changed the world of health care. The first volume of the Trigger Point
Manual had been published in 1983, but I couldn't find anything about trigger points
in the public library. None of the popular family medical guides even mentioned
trigger points. Nothing truly informative was to be found in bookstores. Doctors
were still using drugs as the primary treatment for pain. Many were actively hostile
to the concept of trigger points, discounting the idea as just more bogus medicine,
something purely imaginary.
Only massage therapists seemed to be informed about trigger points and referred pain,
and only exceptional individuals among them (in my own experience at least) were
treating trigger points effectively. What's more, the burgeoning variety of unproven
modalities offered by massage therapists gave the profession such an aura of flakiness
that the elegant science of myofascial pain treatment got unfairly confused with
treatments whose results could easily be attributed to the placebo effect. With
such an identity, how could the medical profession or the public at large ever take
it seriously?
Clearly, there was a world of pain out there in need of the simple and genuine
solutions I felt I had in hand. I despaired of doctors ever listening to me about
trigger point therapy. Taking the facts about myofascial pain directly to the public
seemed the more logical tack. I began to think about leaving the piano business
behind. There was something more important for me to do.
The first thing I wanted to do was to write about the self-treatment of pain for all
my ailing friends in the Piano Technicians Guild. Previous articles in the Piano
Technicians Journal had given me a following. I guessed that my ideas about pain
had a better chance of publication in this journal than almost anywhere else.
I also conceived of giving seminars and workshops about the self-treatment of pain,
and I thought that getting a massage school diploma might give me more credibility.
But I had an even better motive for going to massage school. My daughter Amber had
had chronic back pain ever since lifting a heavy chair during a scene change while
she was working in Summer Theater. Employing my new knowledge about trigger points,
I'd been trying to give her massage, but I just wasn't very good. I didn't know the
time-tested manual techniques used by massage therapists. It would be worth learning
to do massage right, if only to help my daughter; and anything I learned that benefited
my method of self-treatment would be a plus.
I applied to the biggest massage school I could find, one with a busy, well-managed
student clinic where I could get a great deal of experience in the shortest time
possible. At that moment, I couldn't imagine becoming a professional therapist, but
I definitely wanted the skills. With the help of my son-in-law, who I had trained
to take over my piano business, I plowed through a backlog of half a dozen rebuilding
jobs. We cleared my calendar in time for me to start a six-month clinical course
at the Utah College of Massage Therapy.
Massage School
There were forty-nine of us in the class: thirty-six women and thirteen men. We were
a greatly varied group of all backgrounds, from many states and foreign counties, and
ranging in age from seventeen to sixty. It soon became apparent that, although I was
the oldest in the class (and possibly prejudged by most of the others to be a creaking
fuddy-duddy), I was the only one who could claim to be free of pain. All the others
-young and old, male and female-had some kind of enduring problem with pain. I found
that it was almost a cliché that people go to massage school because they have chronic
pain and they're looking for the solution they haven't found elsewhere.
It seemed ironic to me that I arrived in Utah having read both volumes of Travell
and Simons' Trigger Point Manual and having gone a long way toward developing my
method of self-healing, yet I couldn't get anyone to listen. I had just left a
business where my word was taken as gospel. I had disciples. In the role of student,
my accustomed authority was reduced to nil. Nobody wanted to hear what I knew about
trigger points. I could only stand and watch as a fellow student would have a pain
crisis, usually bad neck pain or a back spasm, and run off to a chiropractor or to
the emergency room. I kept offering help and being turned down.
It was even harder to approach the instructors about do-it-yourself massage, but
the anatomy teacher apparently felt less threatened than the others. He was a big,
self-confident guy with a great sense of humor, who didn't fear losing his authority
with the students. During a break one day, he heard me talking to a classmate about
trigger points and asked if I knew how to fix pain. He said he often had pain that
shot diagonally across one side of his chest. He was having it again just that morning.
It wasn't his heart, he said; he'd had it checked. While he explained, I reached up
and began pressing on his neck just above his collarbone. He suddenly stopped talking
and winced, then exclaimed, "Hey, that's it! That's my pain! How did you do that?"
A trigger point in a scalene muscle was causing the pain in his chest. I showed him
how to work the trigger point himself and he told me later that the pain had gone
away and hadn't come back.
I couldn't get over it. This man was a registered nurse and a gifted teacher of
anatomy that knew his muscles but didn't know about his own trigger points. He was
a product of the same system that turns out physicians with the same astounding gap
in their knowledge.
After my classmates saw me go hands-on with our anatomy teacher's trigger points,
they began letting me show them some of my tricks. I showed one student how to kill
her sinus pain by working on her jaw muscles, another how to stop his feet from
hurting by massaging his calves, and another how to get rid of her dizzy spells
with attention to trigger points in the front of her neck. Several eventually came
to me for back pain of various kinds. Near the end of the course, I got to show the
whole class my techniques for getting rid of arm and hand pain, something we all
experienced working in the clinic. Several classes of budding massage therapists
worked in the weekend clinic where it was not unusual for us to give 1200 massages
on a Saturday and Sunday.
I saw the same pain patterns in the clinic that I had seen with my fellow students:
lots of back trouble, plus a broad selection of every other kind of pain you could
think of. I saw pain in every part of the body and every joint: shoulders, elbows,
wrists, knuckles, hips, knees, and ankles. Typically, the client had already been
the rounds of doctors, chiropractors, physical therapists, and so on, looking for
the magician in the white coat. They'd tried yoga, magnets, and pain diets, herbal
therapies, and acupuncture. Some had had their problem for ten years and more.
Many guessed they were just getting arthritis and so were habitually popping pills
They felt older than their years, handicapped by pain. They felt their careers
in danger. Depression due to constant pain was a prevailing theme.
It was exasperating to hear the same stories repeatedly, to know both how simple
their problems were and just what to do for them, and to know many clients were
coming for massage only as a last resort. In my view, massage is the only thing
that works for these kinds of pain, and should be the first thing tried, not the
last. I consistently found trigger points to be the cause of my clients' problems,
and clients nearly always got off my table feeling better. Many left my booth
feeling they'd finally found something that worked. I felt more and more that
I also had found something that worked. I liked giving massage a great deal-I
was surprised at how much. I asked for extra shifts and accumulated twice as
many hours as were required.
Until I was working regularly in clinic, I hadn't seen that giving massage to
others were a way of taking care of me. I'd only been thinking of getting a
diploma from a good school so I would have a bit of credibility when I went on
to teach self-massage. Unexpectedly, I got as much from the massages as my clients
did, maybe more. I felt myself becoming kinder and more empathic. Knowing how to
take care of my own pain had made me more fit for taking care of others, which
made me more fit for taking care of myself. My six months at the Utah College
of Massage Therapy was transformational. I regretted I hadn't done it sooner.
Recurrent Themes
While in massage school I finished writing my series of eight articles on self-applied
trigger point massage for the Piano Technicians Journal. Publication began two months
after I graduated. When the first article appeared, desperate piano tuners began
calling me for advice from all over the United States and Canada. They didn't want
to wait until the article on their particular problem came out. Many were on the
verge of quitting piano work because of chronic pain. Some had been in pain for
as long as twenty years, repeatedly going the rounds of the health-care community
just like I had, with the same frustrating results.
One tuner from New England had been afflicted with severe recurrent pain in both
knees since climbing Mount Katahdin, the highest point in Maine, twelve years
earlier. The pain had started as he descended the mountain and his friends had
had to carry him most of the way to the bottom. Now he couldn't even go out and
mow his lawn without being crippled for days by the effort. Working with me over
the phone, he was able to find and massage the horribly painful trigger points in
his thigh muscles that were causing the pain in his knees. Before we hung up, the
pain was gone. There had been no way for him to know that his trouble was not in
his knees but in his thigh muscles, strained by the unaccustomed mountain climbing:
his doctors, physical therapists, and chiropractors hadn't known. At the Piano
Technicians Guild National Convention a couple of months later, he happily told
me he'd continued working on his trigger points and hadn't had any more trouble
with his knees. I was as pleased as he was.
I was scheduled to give a workshop on the self-treatment of pain at that convention
and was worried that nobody would come. From the number of sufferers who had called
me on the phone, I should've known better. One hundred and ten people showed up,
and it was standing room only in the modest-sized meeting room. I knew at least
one thing about every person in the room before we even began: they all hurt.
Piano technicians are the most diverse, intelligent, creative group of people I've
ever had the privilege to know, and at the same time they're the most assertively
independent. Some literally would rather die than ask for help. If I could tell
them something about the treatment of pain that they could do themselves, they
wanted to hear it. They were all in such need that no one so much as looked away
throughout the whole program. I was very encouraged.
That was the first convention I went to not as a piano tuner, but as a massage
therapist. I didn't go to classes at all that week. I didn't go to committee
meetings. I didn't even party at night. I had something better to do. I spent
every day, from eight in the morning until ten at night, troubleshooting trigger
points and giving massage, only leaving my room to get a quick meal. They weren't
all piano tuners who came to me; spouses needed help too. Although there were some
recurrent themes, like shoulder pain, they brought me all kinds of problems-back
pain, neck pain, headaches, numb hands-just like in the massage school clinic.
People at the convention had come from all over North America, even from several
foreign countries. No matter where these people lived, they all had the same story:
they'd had trouble getting effective treatment. Nobody seemed to know what caused
their pain and nobody could help.
Back in Kentucky, as I began my private practice, again I saw all the by now
familiar patterns. All the people who came for massage had already been to a
physician or a pain clinic. Almost all had experimented with chiropractic. Many
had been to the emergency room for their pain. Most had been through physical
therapy. They had tried everything, including various forms of alternative medicine.
Some had even tried massage but hadn't been impressed. It had been "feel-good"
massage: it had been relaxing but hadn't put a dent in their pain.
Interestingly, almost all the people who came to me had some kind of back pain
along with whatever other pain complaint they had. Their previous treatments for
back pain had always focused on the spine. I heard about injections of papaya or
cortisone. People had usually been told they had arthritis or bad disks, or that
their cartilage had been worn away. They'd been shown X-rays that purported to
prove it. One woman was on her doctor's schedule to have her vertebrae fused. Some
had already had surgery, and frequently had as much pain after surgery as before.
Typically, the surgeon's last word was always that he was sorry but he'd done all
he could. Then he'd renew their prescription for painkillers and dump them off on
a physical therapist. I heard these stories over and over again. And over and over,
I found that trigger point therapy gave them the relief they'd been seeking for so
long. Had trigger points been the problem in the first place? Arthritis? Bad disks?
In Travell and Simons' Trigger Point Manual, I had read that you can have herniated
disks and arthritis of the spine and still find that myofascial trigger points are
the primary cause of your back pain.
One client said her doctor confided sympathetically that he had back pain too. He
wore magnets under his clothing just like she did. Many of my clients had tried
magnets and were often a little embarrassed to say so. Yes, the magnets did seem
to help, they said, but the pain always came back. It was the same with TENS units:
when you took them off, you still had your problem. (A transcutaneous electrical
nerve stimulation [TENS] unit gives you little shocks that interfere with pain
signals, but has no effect on the cause of the pain.)
Nearly everyone I treated was on pain medication of some kind, although few had
the illusion that painkillers were a real cure. People seem to know intuitively
that throwing a cloak over the pain only keeps you from seeing the real problem.
When you hide the problem, you never get the opportunity to address it. Looked at
in this way, painkillers actually perpetuate pain. People want real solutions;
they don't want to dope the problem away.
Another common theme among the people who came to me was numbness and pain in the
hands and fingers. I began to get the impression that the computer keyboard was
crippling the country. I saw wrist braces of all kinds. A doctor had wanted to
put one woman's wrists in casts to heal her numb hands. While many clients feared
they had carpal tunnel syndrome or had even been given the diagnosis, massage of
trigger point in the forearms, shoulder, and neck always took the pain and numbness
away. This outcome was usually a surprise to the client. It soon ceased to be a
surprise to me. Good results were so consistent with "carpal tunnel" symptoms that
I began to wonder whether true carpal tunnel syndrome really existed.
What did all this mean for me? I knew how to help myself and it was clear I
could help other people, but what was the best use of my newfound skills? There
was indeed a world of pain out there, but I'd started too late as a massage
therapist to hope to help very many people one on one. At my age, I wasn't going
to have a long career as a healer. What could I do for the world of pain with
the time and energy I had left? It became increasingly clear that I had to write
a book about trigger point therapy and get this information out to as many
people as possible.
Casting a Wider Net
A doctor should have written this book. It should've been written by a bona
fide, credentialed expert in a white coat with years and years of experience
and scores of articles published in medical journals. If "M.D." followed my name
on the cover of this book, I wouldn't have had to write this chapter. This chapter
is meant to give you some reason to trust what I have to say about pain, some
reason to suspend your disbelief long enough to give my methods a fair try. The
best evidence of whether my method is a good one for you will come from your own
personal experience with it. Trying it is the only way you can truly validate my
claims about its success.
I don't claim to be an authority on pain. Travell and Simons are the pain experts.
In writing this book, my job has primarily been to put their vast knowledge into
more understandable form and transmit it to you. Having figured out how to fix my
own pain counts for something, though. Being a massage therapist counts too, because
I've proven to myself and to my clients that I know how to fix pain for other people.
I thought you might be interested in my shoulder story. I thought you might be
interested in how the wisdom of Janet Travell and David Simons got me through my
difficulties and how they truly gave me a new life. From my success in defeating
pain, I thought you might gain a smidgen of hope: my new life offering the possibility
of a new life for you. My own hope is that this book will be a useful one. It's
you who will prove me right or wrong.
=============================================================================
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain Link
Self-Treatment Examples from
The Trigger Point Therapy Workbook
Original Doctors who found these techniques: Doctors Janet Travell and David Simons
=============================================================================
This is a splendid self-help book for people with persistent musculoskeletal
pain. It tells you how to identify the problem and carefully guides you
through the process of self-treatment. The principles of treating myofascial
pain and myofascial trigger points developed by Doctors Janet Travell and
David Simons form the basis of this book, and are well presented for use
by individuals with pain." Link
--ROBERT D. GERWIN, M.D., Neurologist, Assistant Professor, Johns Hopkin
s School of Medicine; author, Myofascial Pain: An Integrated Approach to
Diagnosis and Treatment (video series)
=============================================================================
Low Back Pain
The reason there are so many differing opinions about the cause of back pain
is that it's mostly referred pain. You may never find back pain's real cause
if you look for it only in the back muscles or the spine. Back pain very often
comes from trigger points in stomach muscles, for instance. The illustration
shows a gluteus medius trigger point that is one of the most common causes of
low back pain:
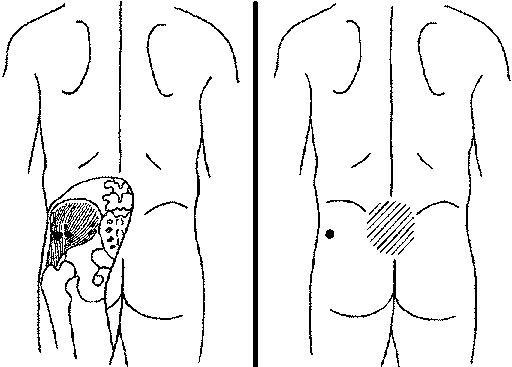 Piriformis Gluteus Medius Trigger Point - Massage with Tennis Ball or Lacrosse Ball
Question: Why use the Lacrosse Ball with the piriformis muscle while you are
against a wall instead of the tennis ball?
The reason is because you get a (deeper) rolling Massage into the painful trigger
points when using the Harder Lacrosse Ball, therefore, breaking up the tight painful
trigger areas that are similar to knotts that need to be softened and loosened
in order to get full elasticity of the muscle and surrounding area, making you
pain free in the long run.
Self-applied trigger point massage breaks into the chemical and neurological
feedback loop that maintains the muscle contractions so that you will have
increased circulation which has been resticted by knotts in the contracted tissue
and the massage will cause the contracted knotts to stretch out, releiving
pressure.
Piriformis Gluteus Medius Trigger Point - Massage with Tennis Ball or Lacrosse Ball
Question: Why use the Lacrosse Ball with the piriformis muscle while you are
against a wall instead of the tennis ball?
The reason is because you get a (deeper) rolling Massage into the painful trigger
points when using the Harder Lacrosse Ball, therefore, breaking up the tight painful
trigger areas that are similar to knotts that need to be softened and loosened
in order to get full elasticity of the muscle and surrounding area, making you
pain free in the long run.
Self-applied trigger point massage breaks into the chemical and neurological
feedback loop that maintains the muscle contractions so that you will have
increased circulation which has been resticted by knotts in the contracted tissue
and the massage will cause the contracted knotts to stretch out, releiving
pressure.
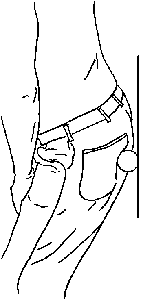 Piriformis Gluteus Medius Trigger Point Ball Massage
The illustration shows treatment of low back pain with massage of the buttocks
muscles using a tennis ball or lacrosse ball against a wall:
(See the Trigger Point Therapy Workbook for more details on how to massage
all the muscles in this important but often neglected area
=============================================================================
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain Link
Reviews by Medical Doctors
of The Trigger Point Therapy Workbook
=============================================================================
The Trigger Point Therapy Workbook is a well-organized, easy-to-use handbook
that will indeed help sufferers of myofascial pain learn to treat themselves
with effective self-massage techniques. The detail and clarity of the books
format will also make it invaluable to pain physicians who want to be able
to teach their patients useful, simple strategies to manage soft tissue pain
problems."
--JOSEPH F. AUDETTE, M.D., Instructor, Harvard Medical School; Director of
Outpatient Pain Services, Spaulding Rehabilitation Hospital, Medford,
Massachusetts
"This is a useful book for anyone in chronic pain. There are few resources
like this one, which empowers the reader to understand the problem and offers
the tools to manage it. The approach to managing pain described in this book
will help many take control of a significant part of their health and will
become a valuable lifelong reference."
--SCOTT M. FISHMAN, M.D., Chief of Pain Medicine, University of California
School of Medicine, Davis, California; author, The War on Pain
=============================================================================
Reviews by Readers
of The Trigger Point Therapy Workbook Link
=============================================================================
Five-Star Amazon Review: Andy from Kansas, August 6, 2003
"Great Book for Anyone with Myofascial Pain Syndrome!
This book can help people with MPS, sprained ankle, tennis elbow, & chronic
back, knee, & neck pain because they are all the same thing! That back pain
or sore wrist that reoccurs often can get worse & even spread. I had pain in
my back after a couple of years it moved up to my neck. Then I got hurt at
work & have been unable to work for a year. I got hurt because my body mechanics
were messed up by trigger points which shorten muscles & put stress on the wrong
areas of your body. Then I spent a year in incredible pain misdiagnosed as
having sciatica.
After getting a proper diagnosis I have used this book to relieve much of my
pain. It does have some short comings, but it has a lot of good info & is easy
to use, plus it's cheap compared to chiropractor & doctor visits. It shows the
source of pain & has detailed info about symptoms & causes. I have been amazed
at how many of lives aches & pains are caused by muscles & can be self treated."
------
ANOTHER REVIEW:
Five-Star Amazon Review: a reader from San Francisco, California, July 28, 2003
"Trigger book worked better than accu/chiro/PT/prescrip/etc.!
I have four "bulged" low back disks. Other than surgery, I've tried everything,
and the approach I found in this book worked best. Hard to believe, but the
simple massage of trigger points is for me a bigger help than acupuncture,
acupressure, chiropractic, PT, yoga, Pilates, Flexeril, NSAIDs, Prednisone, etc.
My wife has plantar fasciitis (a runners' foot injury), and it's helped her, too.
You don't even have to read the book, just look for a picture that locates your
pain, and rub that set of trigger points (although the book is worth a read)."
ANOTHER REVIEW:
Five-Star Amazon Review: John Tinkler from Maryland, March 29, 2002
"I was in so much pain that I couldn't sleep at night. I was diagnosed with
arthritis (hip, back, etc), but I was not satisfied that this explained my pain.
Then I found Davies' book and started to work on trigger points with the rubber
ball he recommends. It didn't solve all my problems, but it reduced my pain to
the point where I could sleep without pills (and demonstrated that my pain was
at least partly muscular)--and all for the cost of a ... little ball! And now
(several other therapies later), I still keep the book and the rubber ball by
my bed, and still follow its directions to massage key areas on a daily basis.
------
ANOTHER REVIEW:
Five-Star Barnes & Noble Review: Elma Johnson, Ph.D., September 25, 2002
"Saved from Disability!
I want to share my enthusiasm for this book. Following the self-treatment methods
in Clair Davies www.triggerpointbook.com book
has saved me from a future of pain and disability and has
also helped several of my friends. About a year and a half ago a terrible fall
strained and tore the muscles and ligaments in my groin and hips and also the medial
meniscus in my left knee. After an orthopedic surgeon restored the knee, he prescribed
physical therapy. However, this made my muscles more painful.
Last winter, after little improvement, I consulted a "Pain Management Specialist"
MD who injected cortisone into my back and prescribed hydrotherapy. Again the exercises
made my legs and hips more painful. So he told me to get a hip replacement or I would
end up in a wheelchair. Unfortunately there are no medical specialists dealing with
muscles and ligaments.
Looking for help at Barnes & Noble, I ran across Clair Davies
www.triggerpointbook.com book. It was easy to locate my trigger points because
of their electric-shock tingle. After I massaged them, I felt much less pain and
was immediately able to sleep on my left side for the first time since the accident.
And improvement has continued. Now I'm painting my condo--without a wheelchair.
Both doctors did their best, as did the physical therapists who tried to help
me--but all in vain. The work of Doctors Travell and Simons on trigger points
seems to have been largely ignored by the medical profession, possibly because
he recommended treatment is cumbersome.
Clair Davies www.triggerpointbook.com book, with its practical suggestions,
is a godsend. Obviously physicians and physical therapists could better help their
patients if they studied it. I have excitedly told others about the book, and a
ripple effect has ensued. For instance, a neighbor, faced with selling her cherished
second-floor condo because she could not take the stairs, has now canceled the sale
and is recommending the book to her friends who are in turn recommending it to
others. And a cousin, whose life had been circumscribed by dizziness that her
doctors could not explain, recovered during one evening's massage, startling her
visiting daughters and causing them to buy their own copies of the book.
I think others will benefit, too. I highly recommend it."
=============================================================================
Trigger Point Therapy Workshops Link
for Massage Therapists
Continuing Education in the Self-Treatment
and Clinical Treatment of Pain
Trigger point therapy is one of the most intriguing and fastest-growing bodywork
styles in the world. Medical doctors, chiropractors, physical therapists, and
massage therapists are all beginning to use this technique to relieve formerly
undiagnosable muscle and joint pain.
The technique involves applying short, repeated massage strokes to trigger points,
tiny contraction knots in muscle tissue where restricted circulation and lack
of oxygen cause referred pain.
Trigger point massage increases circulation and oxygenation in the area and
often produces instant relief.
==============================================================================
A unique massage therapy seminar, presented by father and daughter team,
Clair and Amber Davies, both Nationally Certified in Therapeutic Massage
and Bodywork (NCTMB) from Lexington, Kentucky.
A hands-on pain management seminar, appropriate for all healthcare practitioners
who are interested in simplified diagnosis and practical treatment of myofascial
pain. In addition to massage therapists, we encourage osteopaths, chiropractors,
physical therapists, occupational therapists, nurses and medical doctors to
participate.
Clair Davies www.triggerpointbook.com is approved by the National Certification
Board for Therapeutic Massage and Bodywork (NCBTMB) as a continuing education
provider under Category A.
If you need treatment or instruction in self-treatment,
Amber is seeing clients in her Louisville office.
For an appointment, contact her at 502-895-6833
or at adavies@iglou.com.
--------------------------------------------------------------------------------
What will you gain from this myofascial trigger points workshop?
The massage therapist class starts with pain charts that everybody fills
out at the beginning of class.
During the first part of the day, you are shown how you how to find and treat
your own trigger points with the help of diagrams and with a trained technician
available to walk you through it. The goal is to give you solutions to your pain
problems before the end of the workshop, giving you the benefit of knowing you
can cure yourself of myofascial trigger point pains.
Self treatment is the best way of learning this system. The better skilled
you are at treating yourself the better you will be at finding the
finding and trigger points on others.
Intuition plays a major role in telling you what to do when troubleshooting and
treating your clients' pain problems. In mastering self-treatment, you
learn what works and what does not. The insight learned about pain therapy
is that it can't be gained only by treating someone else.
After each demonstration, you go hands-on with the other participants as they
are now your patients for the day and you practice what you have learned in
class.
There are safe and sure techniques that are more effective in treating pain
in both self-treatment and in your clinical work.
There are always new treatments and ideas coming fourth as the community
gets smarter on the solution for myofascial trigger point pain.
"The Trigger Point Therapy Workbook; Your
Self-Treatment Guide For Pain Relief", by Clair Davies www.triggerpointbook.com.
The book offers a very simple, easy-to-use method for self-treating myofascial
pain in all parts of the body. This new concept is based on deep stroking massage
of trigger points, instead of the old techniques of pressing and holding
which were originally taught in school. The old method is to hard on the
therapists arms, hands and fingers causing problems as the therapist becomes
worn out.
Short, deep strokes are preferred for specific trigger points are easier to
apply to the patient than the old hold and press down techniques.
Deep strokes flush the tissue more thoroughly and accomplish a very beneficial
"microstretch" to the trigger point itself.
It is said that trigger point pains are responsible for up to 80% of common pain
symptoms, and that includes joint pain as well -- according to Doctors Janet
Travell and David Simons.
It's not "tendinitis." It's not "bursitis." It's not "carpal tunnel syndrome."
It's not "adhesive capsulitis." It's not "plantar fasciitis." It's not "loss of joint
cartilage." It's just trigger points in a knott which are affecting the
injured muscles. The challenge is to find those trigger points and treat them
with a successful strategy.
It is hard to realize the fact that most pain is of the myofascial origin.
Misdiagnosis characterize the treatment of pain in all branches of healthcare
and pain management, unfortunately even in the field of therapeutic massage.
Trigger point massage is the most appropriate treatment for common pain,
and yet very few massage therapists have truly understood or
mastered trigger point therapy.
Most massage therapists and other practitioners (even physicians and physical
therapists) are overwhelmed by the technical difficulty of the primary resource
on myofascial pain, Travell and Simons' Myofascial Pain and Dysfunction; The
Trigger Point Manual.This is why widespread myofascial management is now being
spread to every Doctor out there.
The Trigger Point Therapy Workbook gets down to the bassics of trigger point
science. Using 376 illustrations,
It shows how to self-treat trigger points in all 120 pairs of accessible muscles
discussed in Travell and Simons, even such difficult muscles as the subscapularis,
scalenes and psoas.
The new clinical chapter shows you how to adapt the techniques to the massage
studio. The Trigger Point Therapy Workbook is Travell and Simons made easy,
and Dr. David Simons believes in the new workbook as consise material.
The Trigger Point Therapy Workbook is the study guide for those painful knotts
and myofascial pain. The book is $19.95 and is at the Barnes & Noble, Borders Books.
Please bring the workbook to the workshop.
Clair And Amber Davies, Trigger Point Therapists
Piriformis Gluteus Medius Trigger Point Ball Massage
The illustration shows treatment of low back pain with massage of the buttocks
muscles using a tennis ball or lacrosse ball against a wall:
(See the Trigger Point Therapy Workbook for more details on how to massage
all the muscles in this important but often neglected area
=============================================================================
Clair Davies www.triggerpointbook.com talks about
Trigger Points and Referred Pain Link
Reviews by Medical Doctors
of The Trigger Point Therapy Workbook
=============================================================================
The Trigger Point Therapy Workbook is a well-organized, easy-to-use handbook
that will indeed help sufferers of myofascial pain learn to treat themselves
with effective self-massage techniques. The detail and clarity of the books
format will also make it invaluable to pain physicians who want to be able
to teach their patients useful, simple strategies to manage soft tissue pain
problems."
--JOSEPH F. AUDETTE, M.D., Instructor, Harvard Medical School; Director of
Outpatient Pain Services, Spaulding Rehabilitation Hospital, Medford,
Massachusetts
"This is a useful book for anyone in chronic pain. There are few resources
like this one, which empowers the reader to understand the problem and offers
the tools to manage it. The approach to managing pain described in this book
will help many take control of a significant part of their health and will
become a valuable lifelong reference."
--SCOTT M. FISHMAN, M.D., Chief of Pain Medicine, University of California
School of Medicine, Davis, California; author, The War on Pain
=============================================================================
Reviews by Readers
of The Trigger Point Therapy Workbook Link
=============================================================================
Five-Star Amazon Review: Andy from Kansas, August 6, 2003
"Great Book for Anyone with Myofascial Pain Syndrome!
This book can help people with MPS, sprained ankle, tennis elbow, & chronic
back, knee, & neck pain because they are all the same thing! That back pain
or sore wrist that reoccurs often can get worse & even spread. I had pain in
my back after a couple of years it moved up to my neck. Then I got hurt at
work & have been unable to work for a year. I got hurt because my body mechanics
were messed up by trigger points which shorten muscles & put stress on the wrong
areas of your body. Then I spent a year in incredible pain misdiagnosed as
having sciatica.
After getting a proper diagnosis I have used this book to relieve much of my
pain. It does have some short comings, but it has a lot of good info & is easy
to use, plus it's cheap compared to chiropractor & doctor visits. It shows the
source of pain & has detailed info about symptoms & causes. I have been amazed
at how many of lives aches & pains are caused by muscles & can be self treated."
------
ANOTHER REVIEW:
Five-Star Amazon Review: a reader from San Francisco, California, July 28, 2003
"Trigger book worked better than accu/chiro/PT/prescrip/etc.!
I have four "bulged" low back disks. Other than surgery, I've tried everything,
and the approach I found in this book worked best. Hard to believe, but the
simple massage of trigger points is for me a bigger help than acupuncture,
acupressure, chiropractic, PT, yoga, Pilates, Flexeril, NSAIDs, Prednisone, etc.
My wife has plantar fasciitis (a runners' foot injury), and it's helped her, too.
You don't even have to read the book, just look for a picture that locates your
pain, and rub that set of trigger points (although the book is worth a read)."
ANOTHER REVIEW:
Five-Star Amazon Review: John Tinkler from Maryland, March 29, 2002
"I was in so much pain that I couldn't sleep at night. I was diagnosed with
arthritis (hip, back, etc), but I was not satisfied that this explained my pain.
Then I found Davies' book and started to work on trigger points with the rubber
ball he recommends. It didn't solve all my problems, but it reduced my pain to
the point where I could sleep without pills (and demonstrated that my pain was
at least partly muscular)--and all for the cost of a ... little ball! And now
(several other therapies later), I still keep the book and the rubber ball by
my bed, and still follow its directions to massage key areas on a daily basis.
------
ANOTHER REVIEW:
Five-Star Barnes & Noble Review: Elma Johnson, Ph.D., September 25, 2002
"Saved from Disability!
I want to share my enthusiasm for this book. Following the self-treatment methods
in Clair Davies www.triggerpointbook.com book
has saved me from a future of pain and disability and has
also helped several of my friends. About a year and a half ago a terrible fall
strained and tore the muscles and ligaments in my groin and hips and also the medial
meniscus in my left knee. After an orthopedic surgeon restored the knee, he prescribed
physical therapy. However, this made my muscles more painful.
Last winter, after little improvement, I consulted a "Pain Management Specialist"
MD who injected cortisone into my back and prescribed hydrotherapy. Again the exercises
made my legs and hips more painful. So he told me to get a hip replacement or I would
end up in a wheelchair. Unfortunately there are no medical specialists dealing with
muscles and ligaments.
Looking for help at Barnes & Noble, I ran across Clair Davies
www.triggerpointbook.com book. It was easy to locate my trigger points because
of their electric-shock tingle. After I massaged them, I felt much less pain and
was immediately able to sleep on my left side for the first time since the accident.
And improvement has continued. Now I'm painting my condo--without a wheelchair.
Both doctors did their best, as did the physical therapists who tried to help
me--but all in vain. The work of Doctors Travell and Simons on trigger points
seems to have been largely ignored by the medical profession, possibly because
he recommended treatment is cumbersome.
Clair Davies www.triggerpointbook.com book, with its practical suggestions,
is a godsend. Obviously physicians and physical therapists could better help their
patients if they studied it. I have excitedly told others about the book, and a
ripple effect has ensued. For instance, a neighbor, faced with selling her cherished
second-floor condo because she could not take the stairs, has now canceled the sale
and is recommending the book to her friends who are in turn recommending it to
others. And a cousin, whose life had been circumscribed by dizziness that her
doctors could not explain, recovered during one evening's massage, startling her
visiting daughters and causing them to buy their own copies of the book.
I think others will benefit, too. I highly recommend it."
=============================================================================
Trigger Point Therapy Workshops Link
for Massage Therapists
Continuing Education in the Self-Treatment
and Clinical Treatment of Pain
Trigger point therapy is one of the most intriguing and fastest-growing bodywork
styles in the world. Medical doctors, chiropractors, physical therapists, and
massage therapists are all beginning to use this technique to relieve formerly
undiagnosable muscle and joint pain.
The technique involves applying short, repeated massage strokes to trigger points,
tiny contraction knots in muscle tissue where restricted circulation and lack
of oxygen cause referred pain.
Trigger point massage increases circulation and oxygenation in the area and
often produces instant relief.
==============================================================================
A unique massage therapy seminar, presented by father and daughter team,
Clair and Amber Davies, both Nationally Certified in Therapeutic Massage
and Bodywork (NCTMB) from Lexington, Kentucky.
A hands-on pain management seminar, appropriate for all healthcare practitioners
who are interested in simplified diagnosis and practical treatment of myofascial
pain. In addition to massage therapists, we encourage osteopaths, chiropractors,
physical therapists, occupational therapists, nurses and medical doctors to
participate.
Clair Davies www.triggerpointbook.com is approved by the National Certification
Board for Therapeutic Massage and Bodywork (NCBTMB) as a continuing education
provider under Category A.
If you need treatment or instruction in self-treatment,
Amber is seeing clients in her Louisville office.
For an appointment, contact her at 502-895-6833
or at adavies@iglou.com.
--------------------------------------------------------------------------------
What will you gain from this myofascial trigger points workshop?
The massage therapist class starts with pain charts that everybody fills
out at the beginning of class.
During the first part of the day, you are shown how you how to find and treat
your own trigger points with the help of diagrams and with a trained technician
available to walk you through it. The goal is to give you solutions to your pain
problems before the end of the workshop, giving you the benefit of knowing you
can cure yourself of myofascial trigger point pains.
Self treatment is the best way of learning this system. The better skilled
you are at treating yourself the better you will be at finding the
finding and trigger points on others.
Intuition plays a major role in telling you what to do when troubleshooting and
treating your clients' pain problems. In mastering self-treatment, you
learn what works and what does not. The insight learned about pain therapy
is that it can't be gained only by treating someone else.
After each demonstration, you go hands-on with the other participants as they
are now your patients for the day and you practice what you have learned in
class.
There are safe and sure techniques that are more effective in treating pain
in both self-treatment and in your clinical work.
There are always new treatments and ideas coming fourth as the community
gets smarter on the solution for myofascial trigger point pain.
"The Trigger Point Therapy Workbook; Your
Self-Treatment Guide For Pain Relief", by Clair Davies www.triggerpointbook.com.
The book offers a very simple, easy-to-use method for self-treating myofascial
pain in all parts of the body. This new concept is based on deep stroking massage
of trigger points, instead of the old techniques of pressing and holding
which were originally taught in school. The old method is to hard on the
therapists arms, hands and fingers causing problems as the therapist becomes
worn out.
Short, deep strokes are preferred for specific trigger points are easier to
apply to the patient than the old hold and press down techniques.
Deep strokes flush the tissue more thoroughly and accomplish a very beneficial
"microstretch" to the trigger point itself.
It is said that trigger point pains are responsible for up to 80% of common pain
symptoms, and that includes joint pain as well -- according to Doctors Janet
Travell and David Simons.
It's not "tendinitis." It's not "bursitis." It's not "carpal tunnel syndrome."
It's not "adhesive capsulitis." It's not "plantar fasciitis." It's not "loss of joint
cartilage." It's just trigger points in a knott which are affecting the
injured muscles. The challenge is to find those trigger points and treat them
with a successful strategy.
It is hard to realize the fact that most pain is of the myofascial origin.
Misdiagnosis characterize the treatment of pain in all branches of healthcare
and pain management, unfortunately even in the field of therapeutic massage.
Trigger point massage is the most appropriate treatment for common pain,
and yet very few massage therapists have truly understood or
mastered trigger point therapy.
Most massage therapists and other practitioners (even physicians and physical
therapists) are overwhelmed by the technical difficulty of the primary resource
on myofascial pain, Travell and Simons' Myofascial Pain and Dysfunction; The
Trigger Point Manual.This is why widespread myofascial management is now being
spread to every Doctor out there.
The Trigger Point Therapy Workbook gets down to the bassics of trigger point
science. Using 376 illustrations,
It shows how to self-treat trigger points in all 120 pairs of accessible muscles
discussed in Travell and Simons, even such difficult muscles as the subscapularis,
scalenes and psoas.
The new clinical chapter shows you how to adapt the techniques to the massage
studio. The Trigger Point Therapy Workbook is Travell and Simons made easy,
and Dr. David Simons believes in the new workbook as consise material.
The Trigger Point Therapy Workbook is the study guide for those painful knotts
and myofascial pain. The book is $19.95 and is at the Barnes & Noble, Borders Books.
Please bring the workbook to the workshop.
Clair And Amber Davies, Trigger Point Therapists
 Trigger Point Therapy
==============================================================================
Note from this page web designer: I must look at all available options in order
to get the cure for chronic pain of Piriformis Syndrome, and why not try it if
it does not require surgery? I do know I will definitely give it a chance.
An observation: Most Doctors just know about one type of specialty and do
not study the others so they cannot speak to you about a variety of cures
for a given disease or injury. This is where the problem lies. The layman
must do his own research or suffer injury forever. That is why I have
compiled the above information about Piriformis Syndrome and possible
treatments that are available.
I have not tried The Trigger Point Therapy technique with the tennis ball,
or acupuncture or acupressure but have tried back surgery, piriformis surgery,
aqua therapy, physical therapy, stretching, weights, walking, traction, steroids,
cortisone shots and lidocaine shots and lidocaine pain patches.
=============================================================================
* December 28, 2004 - Lidocaine Patch Works! Knocks the pain down some what in
leg. Numbs the area so that the pain is decreased giving me some relief...
I am using the Lidoderm patches, (Active Ingredient: 5% Lidocaine), once a day
for 11 hours per day which is the maximum usage amount of time. I am getting
some relief from this treatment.
Link
Lidocaine Patch Home Page Link
Lidoderm® Patch - Home www.lidoderm.com
The Lidderm® patch is the first FDA-approved therapy indicated to relieve
the pain of postherpetic neuralgia, which is a form of neuropathic pain. ...
The Lidoderm® patch provides targeted peripheral analgesia for the neuropathic
pain.
Trigger Point Therapy
==============================================================================
Note from this page web designer: I must look at all available options in order
to get the cure for chronic pain of Piriformis Syndrome, and why not try it if
it does not require surgery? I do know I will definitely give it a chance.
An observation: Most Doctors just know about one type of specialty and do
not study the others so they cannot speak to you about a variety of cures
for a given disease or injury. This is where the problem lies. The layman
must do his own research or suffer injury forever. That is why I have
compiled the above information about Piriformis Syndrome and possible
treatments that are available.
I have not tried The Trigger Point Therapy technique with the tennis ball,
or acupuncture or acupressure but have tried back surgery, piriformis surgery,
aqua therapy, physical therapy, stretching, weights, walking, traction, steroids,
cortisone shots and lidocaine shots and lidocaine pain patches.
=============================================================================
* December 28, 2004 - Lidocaine Patch Works! Knocks the pain down some what in
leg. Numbs the area so that the pain is decreased giving me some relief...
I am using the Lidoderm patches, (Active Ingredient: 5% Lidocaine), once a day
for 11 hours per day which is the maximum usage amount of time. I am getting
some relief from this treatment.
Link
Lidocaine Patch Home Page Link
Lidoderm® Patch - Home www.lidoderm.com
The Lidderm® patch is the first FDA-approved therapy indicated to relieve
the pain of postherpetic neuralgia, which is a form of neuropathic pain. ...
The Lidoderm® patch provides targeted peripheral analgesia for the neuropathic
pain.
 Lidocaine Patch
The Lidoderm® patch contains lidocaine and is applied directly to intact
skin to treat the neuropathic pain associated with postherpetic neuralgia
(PHN). Learn more about postherpetic neuralgia, shingles, and instructions
=============================================================================
The Lidoderm® patch provides targeted peripheral analgesia for the neuropathic
pain associated with postherpetic neuralgia. Learn more about Lidoderm® patch
clinical studies, its site of action, postherpetic neuralgia, and our patient
education tools.
Here are the results to the new Lidoderm patch with 5% Lidocaine which I am
told is the way of the future for pain relief.
Lidoderm
lidocaine topical (LYE doe cane)
Anestacon, Bactine, Dermaflex, Ela-Max, Ela-Max 5, Ela-Max Plus, Lida Mantle,
Lidocaine Viscous, Lidoderm, Lidomar, Medi-Quik Spray, Protech First Aid Stik,
Solarcaine, Xylocaine 10% Oral, Xylocaine Jelly, Xylocaine Topical, Xylocaine
Viscous, Zilactin-L
What is the most important information I should know about Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
What is Lidoderm?
o Lidocaine causes loss of feeling (numbness) of skin and mucous membranes.
o Lidoderm is used to relieve pain associated with sunburn; insect bites;
poison ivy; poison oak; poison sumac; minor cuts; scratches; and burns; sores
in the mouth; dental procedures; hemorrhoids; and shingles (herpes infection).
o Lidoderm may also be used for purposes other than those listed here.
What should I discuss with my healthcare provider before using Lidoderm?
o Before using Lidoderm, talk to your healthcare provider if you have
· liver problems;
· other serious medical conditions; or
· broken, inflamed, or damaged skin (lidocaine patches).
o You may not be able to use Lidoderm, or you may require a dosage adjustment
or special monitoring during treatment.
o Lidoderm is in the FDA pregnancy category B. This means that it is unlikely
to be harmful to an unborn baby. Do not use Lidoderm without first talking to
your doctor if you are pregnant or could become pregnant during treatment.
o Lidoderm passes into breast milk and may affect a nursing baby. Do not use
Lidoderm without first talking to your doctor if you are breast-feeding.
How should I use Lidoderm?
o Use Lidoderm exactly as directed. If you do not understand these instructions,
ask your doctor, nurse, or pharmacist to explain them to you.
o Lidoderm is intended for external use on the skin only. Do not swallow the
medication (unless specifically directed to do so by your doctor if treating a
throat condition).
o Lidoderm may be applied using the finger tips or a cotton swab. Apply the
medication as directed by your healthcare provider.
o Lidocaine oral cavity patches are applied to the gums by a dentist or a
dental assistant before a dental procedure.
o Lidocaine solution can be swished around the mouth or gargled, and then
spat out. Use a dose-measuring spoon or cup to measure the solution. Ask your
pharmacist if you do not have one.
o Shake the oral spray well before use. Do not inhale the spray.
o Apply the lidocaine patches as directed by your doctor. Make sure the skin
does not have any open sores or rashes. You may apply up to 3 patches at one
time. Leave the patches on for only 12 hours during a 24-hour period. Patches
may be cut into smaller sizes with scissors before removing the adhesive liner.
Clothing may be worn over the patches. If irritation or burning occurs due to
the patch, remove it and do not reapply until the irritation subsides. Dispose
of used lidocaine topical patches where they cannot be reached by children or pets.
o Do not use Lidoderm more often or for longer than is directed. Talk to your
healthcare provider if your symptoms do not improve or if they worsen.
o Store Lidoderm at room temperature away from moisture and heat, out of the
reach of children and pets.
What happens if I miss a dose?
o Apply the missed dose as soon as you remember. If it is almost time for the
next dose, skip the missed dose and use the next regularly scheduled dose as
directed. Do not apply a double dose of this medication.
What happens if I overdose?
o Seek emergency medical attention if an overdose is suspected or if the
medication has been ingested.
o Symptoms of a Lidoderm overdose may include dizziness, drowsiness, confusion,
nervousness, ringing in the ears, blurred or double vision, sensation of heat
or cold, numbness, twitching, seizures, unconsciousness, decreased breathing,
and heart attack.
What should I avoid while using Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
o Since there will be decreased sensation of the skin where Lidoderm is
applied, use caution to avoid injury of the area during treatment.
What are the possible side effects of Lidoderm?
o Stop using Lidoderm and seek emergency medical attention or contact your
doctor immediately if you experience any of the following rare but serious
side effects:
· an allergic reaction (difficulty breathing; closing of the throat;
swelling of the lips, tongue, or face; or hives);;
· chest pain or irregular heartbeats;
· dizziness or drowsiness;
· nausea or vomiting;
· trembling, shaking, or seizures (convulsions); or
· blurred or double vision.
o Other less serious side effects may be more likely to occur. Continue to
use Lidoderm and talk to your healthcare provider if you experience
· mild irritation, redness, or swelling at the application site.
o Side effects other than those listed here may also occur. Continue to use
Lidoderm and talk to your doctor about any side effect that seems unusual or
that is especially bothersome.
What other drugs will affect Lidoderm?
o Although Lidoderm is unlikely to affect medicines taken by mouth, talk
to your doctor before using Lidoderm if you are taking digoxin (Lanoxin)
or any medicine to control irregular heartbeats. You may not be able to use
Lidoderm, or you may require a dosage adjustment or special monitoring.
o Avoid using other topical medications on the affected area without first
talking to your doctor.
o Drugs other than those listed here may also interact with Lidoderm. Talk
to your doctor and pharmacist before taking or using any other prescription or
over-the-counter medicines, including vitamins, minerals, and herbal products.
Where can I get more information?
o Your pharmacist has additional information about Lidoderm written for
health professionals that you may read.
--------------------------------------------------------------------------------
o Remember, keep this and all other medicines out of the reach of children,
never share your medicines with others, and use this medication only for the
indication prescribed.
o Every effort has been made to ensure that the information provided by
Cerner Multum, Inc. ('Multum') is accurate, up-to-date, and complete, but
no guarantee is made to that effect. Drug information contained herein may
be time sensitive. Multum information has been compiled for use by healthcare
practitioners and consumers in the United States and therefore Multum does not
warrant that uses outside of the United States are appropriate, unless specifically
indicated otherwise. Multum's drug information does not endorse drugs, diagnose
patients or recommend therapy. Multum's drug information is an informational
resource designed to assist licensed healthcare practitioners in caring for
their patients and/or to serve consumers viewing this service as a supplement
to, and not a substitute for, the expertise, skill, knowledge and judgment
of healthcare practitioners. The absence of a warning for a given drug or
drug combination in no way should be construed to indicate that the drug or
drug combination is safe, effective or appropriate for any given patient.
Multum does not assume any responsibility for any aspect of healthcare
administered with the aid of information Multum provides. The information
contained herein is not intended to cover all possible uses, directions,
precautions, warnings, drug interactions, allergic reactions, or adverse
effects. If you have questions about the drugs you are taking, check with
your doctor, nurse or pharmacist.
=============================================================================
Directions of Lidoderm within Lidocaine Patch Box:
* ENDO Pharmaceuticals
Lidoderm
(Lidocaine Patch 5%)
Rx only
Description:
LIDODERM (lidocaine patch 5%) is comprised of an adhesive material containing 5%
lidocaine, which is applied to non-woven polyester felt backing and covered with
polyethylene terephthalate (PET) film release liner. The release liner is removed
prior to application to the skin. The size of the patch is 10 cm x 14 cm.
Lidocaine is chemically designated as acetamide, 2-(diethylamino)-N-(2,2-dimethylphenyl),
has an octanol: water partition ratio 43 at pH 7.4, and has the following structure:
CH
/ 3 C H
--- / 2 5
/ \_____NH-CO-CH--N
\ / 2 \
--- C H
\ 2 5
CH
3
Each adhesive patch contains 700 mg of lidocaine (50 mg per ram adhesive) in an
aqueous base. It also contains the following inactive ingredients: dihydroxyaluminim
aminoacetate, disodium edetate, gelatin, glycerin, kaolin, methylparaben, polyacrylic
acid, polyvinyl alcohol, propylene glycol, propylparaben, sodium carboxymethylcellulose,
sodium polyacrylate, D-sorbitol, tartaric acid, and urea.
CLINAL PHARMACOLOGY
Pharmacodynamics:
Lidocaine is an amide-type local anesthetic agent and is suggested to stabilize neuronal
membranes by inhibiting the ionic fluxes required for the initiation and conduction of
impulses.
The penetration of lidocaine into intact skin after application of LIDODERM
is sufficient to produce an analgesic effect, unless than the amount necessary
to produce a complete sensory block.
Pharmacokinetics:
Absorption: The amount of lidocaine systemically absorbed from LIDODERM is directly
related to both the duration of application and the surface area over which it is
applied. In a pharmacokinetic study, three LIDODERM patches were applied over an
area of 420 cm2 of intact skin on the back of normal volunteers for 12 hours. Blood
samples were withdrawn for determination of lidocaine concentration during the
application and for 12 hours after removal of patches. The results are summarized
in Table 1.
CAUTION: This table is incorrect because certain math symbols and notations
are not available in my word processing application. Not to be used for any
medical concerns. Speak to a Doctor before doing anything with Lidocaine.
Lidoderm Application Area Dose C(max) T(max)
Patch Site (cm2) Absorbed (mg) (ug/mL) (hr)
3 patches Back 420 64 + 32 0.3 + 0.06 11 hr
(2100 mg)
When LIDODERM is used according to the recommendation dosing instructions, only
3 + 2% of the dose applied is expected to be absorbed. At least 95% (665 mg)
of lidocaine will remain in a used patch. Mean peak blood concentration of
lidocaine is about 0.13 ug/mL (about 1/10 of the therapeutic concentration
required to treat cardiac arrhythmias). Repeated application of three
patches simultaneously for 12 hours (recommended maximum daily dose), once
per day for three days, indicated that the lidocaine concentration does not
increase with daily use. The mean plasma pharmacokinetic profile for the
15 healthy volunteers are shown in Figure 1.
Figure 1
Mean lidocaine blood concentration after three consecutive daily applications
of three IDODERM patches simultaneously for 12 hours per day in healthy volunteers
(n=15).
=============================================================================
120 . .
. . . . .
100 . . .. . . .
. . . . . .
80 . . . . . .
. . . . . .
60 . . . . . .
. . . . . .
40 . .. . .. . .
. . . . ..
20 .
.
0 .
.
0 6 12 18 24 30 36 42 48 54 60 66 72
HOURS
=============================================================================
DISTRIBUTION:
When lidocaine is administered intravenously to healthy volunteers,
the volume of distribution is 0.7 to 2.7 L/kg (mean 1.5 + 0.6 SD, n=15) At
concentrations produced by application of LIDODEERM, lidocaine is approximately
70% bound to plasma proteins, primarily alpha-1-acid glycoprotein. At much
higher plasma concentrations (1 to 4 ug/mL of free base), the plasma protein
binding of lidocaine is concentration dependent. Lidocaine crosses the
placental and blood brain barriers, presumably by passive diffusion.
METABOLISM:
It is not known if lidocaine is metabolized in the skin. Lidocaine is
metabolized rapidly by the liver to a number of metabolites, including
monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have
pharmacologic activity similar to, but less potent than that of lidocaine.
A minor metabolite, 2,6-xylidine, has unknown pharmacologic activity but is
carcinogenic in rats. The blood concentration of this metabolite is
negligible following ap0plication of LIDODERM (lidocaine patch 5%). Following
intravenous administration, MEGX and GX concentrations in serum range from
11 to 36% and from 5 to 11% of lidocaine concentrations, respectively.
Excretion: Lidocaine and its metabolites are excreted by the kidneys. Less
than 10% of lidocaine is excreted unchanged. The half-life of lidocaine
elimination from the plasma following IV administration is 81 to 149 minutes
(mean 107 + 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min
(mean 0.64 + 0.18 SD, n = 15).
CLINICAL STUDIES
Single-dose treatment with LIDODERM was compared to treatment with vehicle patch
(without lidocaine), and to no treatment (observation only) in a double-blind,
crossover clinical trial with 35 post-herpetic neuralgia patients. Pain
intensity and pain relief scores were evaluated periodically for 12 hours.
LIDODERM performed statistically better than vehicle patch in terms of pain
intensity from 4 to 12 hours.
Multiple-dose, two-week treatment with LIDODERM was compared to vehicle patch
(without lidocaine) in a double-blind, crossover clinical trial of withdrawal type
design conducted in 32 patients, who were considered as responders to the open-
label use of LIDODERM prior to the study. The constant type of pain was
evaluated but not the pain induced by sensory stimuli (dysesthesia). Statistically
significant difference favoring LIDODERM were observed in terms of time to
exit from the trial (14 versus 3.8 days at p-value 0.001), daily average pain
relief, and patient's preference of treatment. About half of the patients also
took oral medications commonly used in the treatment of post-herpetic neuralgia.
The extent of use of concomitant me3dication was similar in the two treatment
groups.
INDICATION AND USAGE
LIDODERM is indicated for relief of pain associated with post-herpetic neuralgia.
It should be applied only to intact skin.
CONTRAINDICATIONS:
LIDODERM is contraindicated in patients with a known history of sensitivity to
local anesthetics of the amide type, or to any other component of the product.
WARNINGS:
Accidental Exposure to Children:
Even a used LIDODERM patch contains a large amount of lidocaine (at least 665 mg).
The potential exists for a small child or a pet to suffer serious adverse effects
from chewing or ingesting a new or used LIDODERM patch, although the risk with this
formulation has not been evaluated. It is important for patients to store and dispose
of LIDODERM out of the reach of children and pets.
Excessive Dosing:
Excessive dosing by applying LIDODERM to larger areas or for longer than the
recommended wearing time could result in increased absorption of lidocaine and
high blood concentrations, leading to serious adverse effects (see ADVERSE REACTIONS,
Systemic Reactions). Lidocaine toxicity could be expected at lidocaine blood
concentrations above 5 ug/mL. The blood application of more than the recommended
number of patches, small patients, or impaired elimination may all contribute to
increasing the blood concentration of lidocaine. With recommended dosing of LIDODERM,
the average peak blood concentration is about 0.13 ug/mL, but concentrations
higher than 0.25 ug/mL have been observed in some individuals.
PRECAUTIONS:
General
Hepatic Disease: Patients with severe hepatic disease are at greater risk of developing
toxic blood concentrations of lidocaine because of their inability to metabolize
lidocaine normally.
Allergic Reactions: Patients allergic to para-aminobenzoic acid derivatives (procaine,
tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
However, LIDODERM should be used with caution in patients with a history of drug
sensitivities, especially if the etiologic agent is uncertain.
Non-Intact Skin: Application to broken or inflamed skin, although not tested, may
result in higher blood concentration of lidocaine from increased absorption.
LIDODERM is only recommended for use on intact skin.
Eye Exposure: The contact of LIDODERM with eyes, although not studied, should be
avoided based on the findings of severe eye irritation with the use of similar
products in animals. If eye contact occurs, immediately wash out the eye with water
or saline and protect the eye until sensation returns.
There are many more precautions: Please read your Prescription label and text of
directions and usage.
Drug Interactions
Antiarrhythmic Drugs: LIDODERM should be used with caution in patients receiving
Class I antiarrhymthmic drugs (such as tocainide and mexiletine) since the toxic
effects are additive and potentially synergistic.
Local Anesthetics
When LIDODERM is used concomitantly with other products containing local anesthetic
agents, the amount absorbed from all formulations must be considered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogensis: A minor metabolite, 2.6-xylidine, has been found to be carcinogenic
in rats. The blood concentration of this metabolite is negligible following
application of LIDODERM.
Mutagenesis: Lidocaine HCI is not mutagenic in Salmonella/mammalian microsome test
nor clastogenic in chromosome aberration assay with human lymphocytes and mouse
micronucleus test.
Impairment of Fertility:
The effect of LIDODERM on fertility as not been studied.
Pregnancy
Teratogenic Effects: Pregnancy Category B.
LIDODERM (lidocaine patch 5%) has not been studied in pregnancy, Reproduction studies
with lidocaine have been performed in rats at doses up to 30 mg/kg subcutaneously
and have revealed no evidence of harm to the fetus due to lidocaine. There are,
however, no adequate and well-controlled studies in pregnant women. Because
animal reproduction studies are not always predictive of human response, LIDODERM
should be use during pregnancy only if clearly needed.
Labor and Delivery
LIDODERM has not been studied in Labor and delivery. Licocaine is not contraindicated
in labor and delivery. Should LIDODERM be used concomitantly with other products
containing lidocaine, total doses contributed by all formulations must be
considered.
Nursing Mothers:
LIDODERM has not been studied in nursing mothers. Lidocaine is excreted in human
mild, and the milk: plasma ratio of lidocaine is 0.45 Caution should be exercised
when LIDODERM is admistered to a nursing woman.
Pediatric USE
Safety and effectiveness in pediatric patients have not been established.
ADVERSE REACTIONS
Localized Reactions
During or immediately after treatment with LIDODERM (lidocaine patch 5%), the skin at
the stie of treatment may develop erythema or edema or may be the locus of abnormal
sensation. These reactions are generally mild and transient, resolving
spontaneously within a few minutes to hours. In clinical studies with LIDODERM,
there were no serious reactions reported. One out of 150 subjects in a three-
week study was discontinued from treatment because of a skin reaction
(erythema and hives).
Allergic Reactions:
Allergic and anaphylactoid reactions associated with lidocaine, although rare, can
occur. They are characterized by urticaria, angioedema, bronchospasm, and shock.
If they occur, they should be managed by conventional means. The detection of
sensitivity by skin testing is of doubtful value.
Systemic (Dose-Related) Reactions
Systemic adverse reactions following appropriate use of LIDODERM are likely, due to
the small dose absorbed (See CLINICAL PHARMACOLOGY, Pharmacokinetics), Systemic
adverse effects of lidocaine are similar in nature to those observed with other
PHARMACOLOGY, Pharmacokinetics). Systemic adverse effects oflidocaieare similar in
nature to those observed with other amide local anesthetic agents, including CNS
excitation and/or depression (light-headedness, nervousness, apprehension, twitching,
tremors, convulsions, unconsciousness, respiratory depression and arrest).
Excitatory CNS reactions may be brief or not occur at all, in which case the
first manifestation may be drowsiness merging into unconsciousness. Cardiovascular
manifestations may include bradycardia, hypotension and cardiovascular collapse
leading to arrest.
OVERDOSAGE:
Lidocaine overdose from cutaneous absorption is rare, but could occur. If there is
any suspicion of lidocaine overdose (see ADVERSE REACTIONS, Systemic Reactions), drug
blood concentration should be checked. The management of overdose includes close
monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible
value in the treatment of acute overdose with lidocaine.
In the absence of massive topical overdose or oral ingestion, evaluation of symptoms
of toxicity should include consideration of other etiologies for the clinical effects,
or over dosage from other sources of lidocaine or other local anesthetics.
The oral LD50 of lidocaine HCI is 459 (346-773) mg/kg (as the salt) in non-fasted
female rats and 214 (159-324) mg/kg (as the salt) in fasted female rats, which are
equivalent to roughly 4000 mg, respectively, in a 60 to 70 kg man based on the
equivalent surface area dosage conversion factors between species.
DOSAGE AND ADMINISTRATION:
Apply LIDODERM to intact skin to cover the most painful areas. Apply up to three
patches, only once for up to 12 hours within a 24-hour period. Patches may be cut
into smaller sizes with scissors prior to removal of the release liner. Clothing
may be worn over the area of application. Smaller areas of treatment are recommended
in a debilitated patient, or a patient with impaired elimination.
If irritated or a burning sensation occurs during application, remove the patch(es)
and do not reapply until the irritation subsides.
When LIDODERM is used concomitantly with other products containing local enesthetic
agents, the amount absorbed from all formulations must be considered.
HANDLING AND DISPOSAL:
Hands should be washed after the handling of LIDODERM, and eye contact with LIDODERM
should be avoided. The used patch should be immediately disposed of in such a way
as to prevent its access by children and pets.
HOW SUPPLIED:
LIDODERM (Lidocaine patch 5%) is available as the following:
Carton of 30 patches, packaged into individual child-resistant envelopes
Store at 25C (77 degrees) excursions permitted to 15 to 30 Celsius (59 degree to
86 degree farenheight) See USP Controlled Room Temperature).
Manufactured for:
Endo Pharmaceutical Inc. ENDO
Chadds Ford, Pennsylvania 19317
LIDODERM is a Registered Trademark of Hind Health Care, INC.
=============================================================================
A pressure point procedure found on the internet to help another patient
of piriformis problems in which the Piriformis Muscle needed to be stretched
out back to its original length -- Here is the therapy for that below:
=============================================================================
Sciatica? Piriformis? This helped me
Link
This article submitted by Larry Swain on 1/20/99.
Email Address: swainl@vitrex.net
http://neuro-www.mgh.harvard.edu/forum/ChronicPainF/1.20.992.58AMSciaticaPiriformi/
I would like to pass along something that has worked very well for me and I hope
that it will help some of you out there suffering from lower back problems and
sciatica as I was.
I have had very bad back problems for the past 15 years that have nearly
incapacitated me. I was diagnosed with degenerative disk disease, 4 herniated
disks and a badly bulged disk which made life unbearable. I had sciatic pain so
bad that many days I couldn't walk without a cane and at night I would get a
numbness and tingling in my legs that nearly drove me crazy.
I went to many doctors, neurosurgeons etc. and they tried all kinds of pain killers,
direct injections into the muscles, etc. with no help at all. A few years ago I tried
deep tissue massage therapy and that has really helped keep the pain to a level that
I can tolerate.
About 7 months ago I learned about some techniques they are using in a pain clinic
in England and I had my therapist try some of them on me with great results. I found
out that a lot of my lower back pain came from a compressed piriformis muscle.
I would like to pass one of these treatments along to you sciatica and piriformis
sufferers and hope that it will help some of you out there. If you have a spouse or
friend that can apply it to you it doesn't cost anything, it's non-invasive and if
it doesn't work you won't be any worse off than you were. My therapist has tried it
on a number of people and it has helped most all of them.
This treatment is so simple that I thought that it was a joke and I didn't try it
until I was in such pain that I would try anything to relieve it. It needs another
person to apply the treatment and it can be a spouse, friend or therapist. There are
two treatments for the piriformis release and I will try to describe them as best and
simply as I can.
The piriformis muscle is a small muscle not much larger than your thumb and it
runs from the top of the leg bone across the buttock to the sacrum which is at the
base of the spinal column. When this little muscle gets irritated due to over use
from sitting, bending or whatever it can compress and pinch the sciatic nerve and
the attachment points are stretched to the limit causing a great deal of pain.
Sometimes it is very difficult to get this muscle to relax and resume its normal
length and that is what this treatment will help with.
Sciatica is a fairly common disorder and approximately 40% of the population
experiences it at some point in their lives. However, only about 1% has coexisting
sensory or motor deficits. Sciatic pain has several root causes and treatment may
hinge upon the underlying problem.
Chronic pain may arise from more than just compression on the nerve. According
to some pain researchers, physical damage to a nerve is only half of the equation.
A developing theory proposes that some nerve injuries result in a release of
neurotransmitters and immune system chemicals that enhance and sustain a pain
message. Even after the injury has healed, or the damage has been repaired, the
pain continues. Control of this abnormal type of pain is difficult.
You will need a firm padded surface to lay the patient on. A table or the floor
with a 3" or 4" foam pad works well. A bed has too much give to it.
Treatment #1
Have the patient lay on their side facing away from you with their legs pulled up to
a comfortable position and one on top of the other.
(optional) Hot moist towels placed on the buttock and hip muscles for about 15 minutes
sure feels good and helps to relax the muscles. Moist heat seems to penetrate deeper
into the muscles. Be careful not to get it hot enough to burn the skin or be
uncomfortable.
If the patient is laying on their right side, facing away from you, place the heel of
your right hand in the middle of the buttock muscle and lean into it and hold it. With
your left hand grasp their foot or ankle and lift it straight up about 12"" rotating
the leg . This will probably be painful so be careful of your patient's pain threshold.
Gently lay the foot and leg back down and release the pressure with the right hand.
Apply the pressure with the right hand , lift the leg , gently lower it, release the
pressure.
Go through this same sequence for about 15 minutes working your hand up and down the
hip and buttock muscles then turn the patient over on the other side and repeat the
steps. If this length of time is too much for the patient just do it for a couple of
minutes to start and try to work up to a longer time.
Treatment #2
Working the right side
Have patient lay on stomach.
Move to the right side of patient.
Grasp the ankle and lift the lower part of the leg so that the bottom of the foot is
pointing straight up.
Push the foot away from you as if you were trying to touch the heel to the left buttock
muscle to rotate the leg. Be sure to monitor the patient's pain level and not overdue
it.
Place the heel of the hand in the middle of the buttock muscle as in treatment #1 and
lean into it to apply pressure.
While applying pressure with the right hand, pull the leg back toward you to the
starting position.
Release the pressure with the right hand.
Push the leg away from you, apply pressure with the right hand, and pull leg toward you,
release the pressure with the right hand.
Continue this sequence for the same time as in treatment #1 and then move to the other
side of the body and work it in the same way.
You can work each of these treatments as an individual treatment or you can work both
of them in a single session. The total time should be about 30 minutes for the whole
treatment.
Some effects of it may show up after the treatment but the real effects take about 11
to 12 hours to really set in. After the first 3 or 4 rotations the muscle will try to
return to its compressed state but after 10 or 12 rotations it will gradually start to
lengthen out little by little until it reaches its normal length. This treatment may
need to be done for 3 or 4 sessions a couple of days apart for the maximum effect.
I hope this treatment will help some of you as much as it has helped me. Good luck to
you all in finding cure for your ailments. God Bless.
=============================================================================
FULL DISCLAIMER
=============================================================================
Sciatica Org Site: Link
Functional Entrapments: What are they?
Functional entrapment syndromes are defined as significant neurological compression
resulting from positional or kinesiological considerations, not solely structural
or inflammatory conditions.
For this reason, imaging studies such as MRI, CT, bone and gallium scans and
diagnostic ultrasound is of limited value in detecting these conditions. Even
conventional EMG is often negative. Rather, it is in comparing nerve conductions
in the anatomical position with nerve conductions in the symptomatic position that
turns up the pathology, and the pathogenetic mechanism. This offers both guidance
on effective treatment, and a means of assessing the efficacy of treatment through
repeated serial testing of the same nerve conductions.
Rehabilitation Medicine is well-suited to work with these common causes of pain,
since PM&R knows anatomy and kinesiology, does electro diagnostic testing as an
extension of the physical exam, is functionally oriented, and is comfortable using
both injection and physical therapeutic techniques in treatment.
Examples:
Piriformis syndrome comprises approximately 6 to 8 percent of sciatica and low back
pain. (1) While herniated nucleus pulpous and spinal stenosis are more common,
piriformis syndrome is under diagnosed, (2). Therefore, its prevalence is significantly
higher than its incidence (3).
The syndrome is due to the piriformis muscle compressing the sciatic nerve in the
buttock, and, like pronator syndrome or carpal tunnel, causing damage to the peripheral
nerve through excessive pressure. (4) The nerve is pressed backward against the sharp
tendinous edges of other muscles such as the gemellus superior and obturator internus,
(5-6) and the condition may easily become chronic, and debilitating.
History
Discovered in Florence ca. 1580. After Mixter and Barr's paper in 1932 (7), people
recognized spinal and intramedullary pathology as the chief cause of sciatica. It
is foraminal and intramedullary conditions that come to mind when patients present
with sciatica. However, pain along the course of the sciatic nerve at times is caused
by pathological involvement of the nerve itself, and rational diagnosis and treatment
then should focus on the site of the pathology.
Epidemiology
Since an estimated 80 million Americans suffer low back pain and sciatica annually,
(8) 4.8 to 6.4 million people contract piriformis syndrome annually. One reason for
Under diagnosis is that MRI, myelogram, CT, are unlikely to turn up any evidence of
piriformis syndrome. (9-11) It is a functional syndrome: only certain positions and
pressures bring out the pain, paresthesias, and weakness that come with it. Structure
imaging studies are of minimal value here. (12-15)
Since it is sometimes considered a diagnosis of exclusion, many patients receive
painful and pointless surgical and other procedures based on limited inquiries and
faulty diagnosis.
Piriformis Syndrome is commonest among very active people such as athletes, health
club users, joggers, and performers, and those who sit a great deal such as members
of the financial community, lawyers, psychotherapists, secretaries and vehicular drivers
. After occupational causes, trauma is the second greatest cause of piriformis syndrome.
Lifting and other back strain related activities are third, with many other initiating
events including misplaced gluteal injections, lipomas, and unusual furniture.
Diagnosis
Modern methods of diagnosis began with the work of Fishman and Zybert (14) using the
H-reflex and EMG in 1992. By timing the H-reflex in the position of Flexion Adduction
and Internal Rotation, (the FAIR-test) in which the piriformis muscle tightly presses
the sciatic nerve against the underlying structures, and comparing the timing with
the H-reflex in the anatomical position, the amount of delay was measured in normals.
These values were then compared to those seen in patients meeting clinical criteria
for piriformis syndrome. Patients with piriformis syndrome had FAIR-test values which
were, on the average, more than three standard deviations beyond the mean seen in
normals and in contra lateral lower extremities. More than 80 percent of patients so
diagnosed improved 50 percent or more with conservative therapy aimed at loosening
the piriformis muscle in the buttock. The recovery rate of patients identified by
the FAIR-test is much greater than the recovery rate seen in patients selected by
any other known means. (15)
Because of the nature of the syndrome, the test for piriformis syndrome is functional
in nature, comparing nerve conduction values when the nerve is compressed, with values
seen in a resting position. The discrepancy between normal values and those seen in
piriformis syndrome is amplified by the fact that the H-reflex crosses the buttock
In order to determine these values, posterior tibial and peroneal H-reflexes are studied
both in the anatomical position and the flexed adducted internally rotated position
(FAIR-test). Thus the H-reflex is actually performed four times with each limb that
is studied. (15)
Clinical Experience
Treatment at first was simply physical therapy, informed and enriched by the generous
giving forth of experience from the international medical community. In essence, the
therapy lengthened the piriformis muscle, reducing spasm and pressure on the descending
sciatic nerve, and giving the nerve enough slack to remove itself from harm's way. See
the rest of the website for the specific program. The therapy was helpful, but progress
was slow. On the suggestion of Dr. Janet Travell, we began injecting Triamcinolone
Acetonide 20mg with 1.5cc of 2% lidocaine into the motor point of the piriformis muscle,
just medial to its musculotendinous junction in the lateral buttock.
This had only rare minor and transient side-effects on non-diabetics, and shortened
the recovery time considerably.
On average 10.2 month follow-up time of 1014 cases of piriformis syndrome, more than
hat these patients had suffered from piriformis syndrome for an average of 6.2 years,
Probably due to piriformis syndrome being considered a diagnosis of exclusion, other,
less important diagnostic entities had received undue attention in these patients.
Among these1014 cases there had been over 400 spinal, trochanteric and gynecological
surgeries, none of which was definitive, more than 1500 imaging studies, of which
less than 1/5 were relevant, and more than 10,000 appointments with clinicians for
diagnostics, epidurals, physical therapy, and alternative methods of pain relief.
More recently we have conducted several IRB-approved studies of more specific nerve
blocks, using the toxin of the botulinum bacterium. In the latest and most successful
of these, we have found that 12,500 units of botulinum B toxin has well above 85%
efficacy, and fewer side effects than Triamcinolone and Lidocaine, giving more relief
faster, and appearing in early studies to last longer. Containing no steroid, this
preparation is also suitable for diabetics. Showing a much more rapid decline in pain
levels, and normalization of the FAIR-test, it obviates physical therapy sessions that
surpass the cost of the injection.
In summary, there are four reasons that botulinum toxin helps in the treatment of
piriformis syndrome.
A reliable correlation between diagnosis and effective treatment exists.
More than 5,000,000 currently improperly treated patients will continue to suffer, and
continue to consume health care resources in vain unless and until adequate treatment
is afforded them. In clinical experience, injection of botulinum toxin has proven the
most effective treatment.
Cost-benefit analysis of current data strongly supports injection of botulinum toxin
in the treatment of piriformis syndrome.
Two other considerations are relevant:
Wider applicability. While the anti-insulinemic effect of steroids strongly
contraindicates their use in diabetic patients, there are virtually no documented
allergic reactions to botulinum toxins.
Longer efficacy. Steroid injection without physical therapy is generally effective for
1-3 weeks. Botulinum toxin injections without physical therapy are effective for at
least three months. In the past, approximately 15% of patients treated without botulinum
toxin injections have had recurrence of piriformis syndrome within three years. As of
today, (14 months after our first injection) we have seen 3 relapses following botulinum
toxin injections in 61 patients.
A Patients Success Story: Link
Cindy W., IT manager from NC.
Successful ADR, but I was still completely disabled.
The first time I met Mark was on September 19, 2002. We were in the waiting room at
the Alpha Klinik and we both had surgery scheduled for the next day. After we chatted
for a while, I realized that I was speaking to someone who had written a great deal on
the internet about his research into ADR. I said, "Oh my gosh, you are RumorSlayer!
I used to look for you online. I'd call my husband over. Ed, Ed, he's here again!!!
Come read this!"
I was in Munich for surgery because I had disabling back pain, hip pain and foot pain.
I was very relieved after my discogram because it so clearly reproduced all my pain.
That made me an excellent candidate and gave me every reason to be hopeful.
My first week post-op was incredible. I felt sorry for Mark because he was having such
a tough post-op experience, while I was walking many miles a day and sightseeing around
Munich just 5 or 6 days after my surgery. I knew just a few days after my surgery that
my back pain and my foot pain were GONE!
Fast forward about a year and Mark's in great shape, but I was still functionally
disabled. Although my disc replacement solved my back and foot pain, my disabling
hip pain still had me unable to function. I was still on large doses of OxyContin.
I'd been to doctor after doctor, but none of them had any good ideas. I had been
referred to pain management. I was ready to give up.
One day Mark called me up and told me about someone he met on the Internet forum he'd
started for people who want to discuss non-fusion technologies. He told me that I there
was a man he'd spoken with, who described disabling hip pain EXACTLY like I described
mine. I took Mark's advice and called Brian. Brian had a similar story, but had
found his way to a Dr. in Cincinnati who specialized in Piriformis syndrome. I
called the Dr. but he warned me that Piriformis syndrome is very rare and that I
shouldn't get my hopes up.
Fast forward another 6 or 7 months! It turned out that I had profound PS.
Out of 80 cases this doctor had seen, he said that my case was certainly one of
the worst. I had the piriformis release surgery in October of 2003 and by mid-2004,
I was riding my mountain bike with my husband, camping, hiking, working full time,
back to a rewarding workout regimen (I was an athlete before my disability). I
can't believe it, I'm living a NORMAL LIFE! I was ready to give up. I don't know
where I'd be now if it wasn't for Mark and his Patient Network. I suppose that I'd
still be in pain management, on large doses of opiates and completely disabled.
Instead, I have a new lease on life and can live every day to the fullest. With
the perspective that you gain from being reborn after such a painful disability,
life is even better than it was before I could truly appreciate what it means to
enjoy a day without pain!
Thanks
==================================================================================
Sciatic Notch lesser sciatic notch
Lidocaine Patch
The Lidoderm® patch contains lidocaine and is applied directly to intact
skin to treat the neuropathic pain associated with postherpetic neuralgia
(PHN). Learn more about postherpetic neuralgia, shingles, and instructions
=============================================================================
The Lidoderm® patch provides targeted peripheral analgesia for the neuropathic
pain associated with postherpetic neuralgia. Learn more about Lidoderm® patch
clinical studies, its site of action, postherpetic neuralgia, and our patient
education tools.
Here are the results to the new Lidoderm patch with 5% Lidocaine which I am
told is the way of the future for pain relief.
Lidoderm
lidocaine topical (LYE doe cane)
Anestacon, Bactine, Dermaflex, Ela-Max, Ela-Max 5, Ela-Max Plus, Lida Mantle,
Lidocaine Viscous, Lidoderm, Lidomar, Medi-Quik Spray, Protech First Aid Stik,
Solarcaine, Xylocaine 10% Oral, Xylocaine Jelly, Xylocaine Topical, Xylocaine
Viscous, Zilactin-L
What is the most important information I should know about Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
What is Lidoderm?
o Lidocaine causes loss of feeling (numbness) of skin and mucous membranes.
o Lidoderm is used to relieve pain associated with sunburn; insect bites;
poison ivy; poison oak; poison sumac; minor cuts; scratches; and burns; sores
in the mouth; dental procedures; hemorrhoids; and shingles (herpes infection).
o Lidoderm may also be used for purposes other than those listed here.
What should I discuss with my healthcare provider before using Lidoderm?
o Before using Lidoderm, talk to your healthcare provider if you have
· liver problems;
· other serious medical conditions; or
· broken, inflamed, or damaged skin (lidocaine patches).
o You may not be able to use Lidoderm, or you may require a dosage adjustment
or special monitoring during treatment.
o Lidoderm is in the FDA pregnancy category B. This means that it is unlikely
to be harmful to an unborn baby. Do not use Lidoderm without first talking to
your doctor if you are pregnant or could become pregnant during treatment.
o Lidoderm passes into breast milk and may affect a nursing baby. Do not use
Lidoderm without first talking to your doctor if you are breast-feeding.
How should I use Lidoderm?
o Use Lidoderm exactly as directed. If you do not understand these instructions,
ask your doctor, nurse, or pharmacist to explain them to you.
o Lidoderm is intended for external use on the skin only. Do not swallow the
medication (unless specifically directed to do so by your doctor if treating a
throat condition).
o Lidoderm may be applied using the finger tips or a cotton swab. Apply the
medication as directed by your healthcare provider.
o Lidocaine oral cavity patches are applied to the gums by a dentist or a
dental assistant before a dental procedure.
o Lidocaine solution can be swished around the mouth or gargled, and then
spat out. Use a dose-measuring spoon or cup to measure the solution. Ask your
pharmacist if you do not have one.
o Shake the oral spray well before use. Do not inhale the spray.
o Apply the lidocaine patches as directed by your doctor. Make sure the skin
does not have any open sores or rashes. You may apply up to 3 patches at one
time. Leave the patches on for only 12 hours during a 24-hour period. Patches
may be cut into smaller sizes with scissors before removing the adhesive liner.
Clothing may be worn over the patches. If irritation or burning occurs due to
the patch, remove it and do not reapply until the irritation subsides. Dispose
of used lidocaine topical patches where they cannot be reached by children or pets.
o Do not use Lidoderm more often or for longer than is directed. Talk to your
healthcare provider if your symptoms do not improve or if they worsen.
o Store Lidoderm at room temperature away from moisture and heat, out of the
reach of children and pets.
What happens if I miss a dose?
o Apply the missed dose as soon as you remember. If it is almost time for the
next dose, skip the missed dose and use the next regularly scheduled dose as
directed. Do not apply a double dose of this medication.
What happens if I overdose?
o Seek emergency medical attention if an overdose is suspected or if the
medication has been ingested.
o Symptoms of a Lidoderm overdose may include dizziness, drowsiness, confusion,
nervousness, ringing in the ears, blurred or double vision, sensation of heat
or cold, numbness, twitching, seizures, unconsciousness, decreased breathing,
and heart attack.
What should I avoid while using Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
o Since there will be decreased sensation of the skin where Lidoderm is
applied, use caution to avoid injury of the area during treatment.
What are the possible side effects of Lidoderm?
o Stop using Lidoderm and seek emergency medical attention or contact your
doctor immediately if you experience any of the following rare but serious
side effects:
· an allergic reaction (difficulty breathing; closing of the throat;
swelling of the lips, tongue, or face; or hives);;
· chest pain or irregular heartbeats;
· dizziness or drowsiness;
· nausea or vomiting;
· trembling, shaking, or seizures (convulsions); or
· blurred or double vision.
o Other less serious side effects may be more likely to occur. Continue to
use Lidoderm and talk to your healthcare provider if you experience
· mild irritation, redness, or swelling at the application site.
o Side effects other than those listed here may also occur. Continue to use
Lidoderm and talk to your doctor about any side effect that seems unusual or
that is especially bothersome.
What other drugs will affect Lidoderm?
o Although Lidoderm is unlikely to affect medicines taken by mouth, talk
to your doctor before using Lidoderm if you are taking digoxin (Lanoxin)
or any medicine to control irregular heartbeats. You may not be able to use
Lidoderm, or you may require a dosage adjustment or special monitoring.
o Avoid using other topical medications on the affected area without first
talking to your doctor.
o Drugs other than those listed here may also interact with Lidoderm. Talk
to your doctor and pharmacist before taking or using any other prescription or
over-the-counter medicines, including vitamins, minerals, and herbal products.
Where can I get more information?
o Your pharmacist has additional information about Lidoderm written for
health professionals that you may read.
--------------------------------------------------------------------------------
o Remember, keep this and all other medicines out of the reach of children,
never share your medicines with others, and use this medication only for the
indication prescribed.
o Every effort has been made to ensure that the information provided by
Cerner Multum, Inc. ('Multum') is accurate, up-to-date, and complete, but
no guarantee is made to that effect. Drug information contained herein may
be time sensitive. Multum information has been compiled for use by healthcare
practitioners and consumers in the United States and therefore Multum does not
warrant that uses outside of the United States are appropriate, unless specifically
indicated otherwise. Multum's drug information does not endorse drugs, diagnose
patients or recommend therapy. Multum's drug information is an informational
resource designed to assist licensed healthcare practitioners in caring for
their patients and/or to serve consumers viewing this service as a supplement
to, and not a substitute for, the expertise, skill, knowledge and judgment
of healthcare practitioners. The absence of a warning for a given drug or
drug combination in no way should be construed to indicate that the drug or
drug combination is safe, effective or appropriate for any given patient.
Multum does not assume any responsibility for any aspect of healthcare
administered with the aid of information Multum provides. The information
contained herein is not intended to cover all possible uses, directions,
precautions, warnings, drug interactions, allergic reactions, or adverse
effects. If you have questions about the drugs you are taking, check with
your doctor, nurse or pharmacist.
=============================================================================
Directions of Lidoderm within Lidocaine Patch Box:
* ENDO Pharmaceuticals
Lidoderm
(Lidocaine Patch 5%)
Rx only
Description:
LIDODERM (lidocaine patch 5%) is comprised of an adhesive material containing 5%
lidocaine, which is applied to non-woven polyester felt backing and covered with
polyethylene terephthalate (PET) film release liner. The release liner is removed
prior to application to the skin. The size of the patch is 10 cm x 14 cm.
Lidocaine is chemically designated as acetamide, 2-(diethylamino)-N-(2,2-dimethylphenyl),
has an octanol: water partition ratio 43 at pH 7.4, and has the following structure:
CH
/ 3 C H
--- / 2 5
/ \_____NH-CO-CH--N
\ / 2 \
--- C H
\ 2 5
CH
3
Each adhesive patch contains 700 mg of lidocaine (50 mg per ram adhesive) in an
aqueous base. It also contains the following inactive ingredients: dihydroxyaluminim
aminoacetate, disodium edetate, gelatin, glycerin, kaolin, methylparaben, polyacrylic
acid, polyvinyl alcohol, propylene glycol, propylparaben, sodium carboxymethylcellulose,
sodium polyacrylate, D-sorbitol, tartaric acid, and urea.
CLINAL PHARMACOLOGY
Pharmacodynamics:
Lidocaine is an amide-type local anesthetic agent and is suggested to stabilize neuronal
membranes by inhibiting the ionic fluxes required for the initiation and conduction of
impulses.
The penetration of lidocaine into intact skin after application of LIDODERM
is sufficient to produce an analgesic effect, unless than the amount necessary
to produce a complete sensory block.
Pharmacokinetics:
Absorption: The amount of lidocaine systemically absorbed from LIDODERM is directly
related to both the duration of application and the surface area over which it is
applied. In a pharmacokinetic study, three LIDODERM patches were applied over an
area of 420 cm2 of intact skin on the back of normal volunteers for 12 hours. Blood
samples were withdrawn for determination of lidocaine concentration during the
application and for 12 hours after removal of patches. The results are summarized
in Table 1.
CAUTION: This table is incorrect because certain math symbols and notations
are not available in my word processing application. Not to be used for any
medical concerns. Speak to a Doctor before doing anything with Lidocaine.
Lidoderm Application Area Dose C(max) T(max)
Patch Site (cm2) Absorbed (mg) (ug/mL) (hr)
3 patches Back 420 64 + 32 0.3 + 0.06 11 hr
(2100 mg)
When LIDODERM is used according to the recommendation dosing instructions, only
3 + 2% of the dose applied is expected to be absorbed. At least 95% (665 mg)
of lidocaine will remain in a used patch. Mean peak blood concentration of
lidocaine is about 0.13 ug/mL (about 1/10 of the therapeutic concentration
required to treat cardiac arrhythmias). Repeated application of three
patches simultaneously for 12 hours (recommended maximum daily dose), once
per day for three days, indicated that the lidocaine concentration does not
increase with daily use. The mean plasma pharmacokinetic profile for the
15 healthy volunteers are shown in Figure 1.
Figure 1
Mean lidocaine blood concentration after three consecutive daily applications
of three IDODERM patches simultaneously for 12 hours per day in healthy volunteers
(n=15).
=============================================================================
120 . .
. . . . .
100 . . .. . . .
. . . . . .
80 . . . . . .
. . . . . .
60 . . . . . .
. . . . . .
40 . .. . .. . .
. . . . ..
20 .
.
0 .
.
0 6 12 18 24 30 36 42 48 54 60 66 72
HOURS
=============================================================================
DISTRIBUTION:
When lidocaine is administered intravenously to healthy volunteers,
the volume of distribution is 0.7 to 2.7 L/kg (mean 1.5 + 0.6 SD, n=15) At
concentrations produced by application of LIDODEERM, lidocaine is approximately
70% bound to plasma proteins, primarily alpha-1-acid glycoprotein. At much
higher plasma concentrations (1 to 4 ug/mL of free base), the plasma protein
binding of lidocaine is concentration dependent. Lidocaine crosses the
placental and blood brain barriers, presumably by passive diffusion.
METABOLISM:
It is not known if lidocaine is metabolized in the skin. Lidocaine is
metabolized rapidly by the liver to a number of metabolites, including
monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have
pharmacologic activity similar to, but less potent than that of lidocaine.
A minor metabolite, 2,6-xylidine, has unknown pharmacologic activity but is
carcinogenic in rats. The blood concentration of this metabolite is
negligible following ap0plication of LIDODERM (lidocaine patch 5%). Following
intravenous administration, MEGX and GX concentrations in serum range from
11 to 36% and from 5 to 11% of lidocaine concentrations, respectively.
Excretion: Lidocaine and its metabolites are excreted by the kidneys. Less
than 10% of lidocaine is excreted unchanged. The half-life of lidocaine
elimination from the plasma following IV administration is 81 to 149 minutes
(mean 107 + 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min
(mean 0.64 + 0.18 SD, n = 15).
CLINICAL STUDIES
Single-dose treatment with LIDODERM was compared to treatment with vehicle patch
(without lidocaine), and to no treatment (observation only) in a double-blind,
crossover clinical trial with 35 post-herpetic neuralgia patients. Pain
intensity and pain relief scores were evaluated periodically for 12 hours.
LIDODERM performed statistically better than vehicle patch in terms of pain
intensity from 4 to 12 hours.
Multiple-dose, two-week treatment with LIDODERM was compared to vehicle patch
(without lidocaine) in a double-blind, crossover clinical trial of withdrawal type
design conducted in 32 patients, who were considered as responders to the open-
label use of LIDODERM prior to the study. The constant type of pain was
evaluated but not the pain induced by sensory stimuli (dysesthesia). Statistically
significant difference favoring LIDODERM were observed in terms of time to
exit from the trial (14 versus 3.8 days at p-value 0.001), daily average pain
relief, and patient's preference of treatment. About half of the patients also
took oral medications commonly used in the treatment of post-herpetic neuralgia.
The extent of use of concomitant me3dication was similar in the two treatment
groups.
INDICATION AND USAGE
LIDODERM is indicated for relief of pain associated with post-herpetic neuralgia.
It should be applied only to intact skin.
CONTRAINDICATIONS:
LIDODERM is contraindicated in patients with a known history of sensitivity to
local anesthetics of the amide type, or to any other component of the product.
WARNINGS:
Accidental Exposure to Children:
Even a used LIDODERM patch contains a large amount of lidocaine (at least 665 mg).
The potential exists for a small child or a pet to suffer serious adverse effects
from chewing or ingesting a new or used LIDODERM patch, although the risk with this
formulation has not been evaluated. It is important for patients to store and dispose
of LIDODERM out of the reach of children and pets.
Excessive Dosing:
Excessive dosing by applying LIDODERM to larger areas or for longer than the
recommended wearing time could result in increased absorption of lidocaine and
high blood concentrations, leading to serious adverse effects (see ADVERSE REACTIONS,
Systemic Reactions). Lidocaine toxicity could be expected at lidocaine blood
concentrations above 5 ug/mL. The blood application of more than the recommended
number of patches, small patients, or impaired elimination may all contribute to
increasing the blood concentration of lidocaine. With recommended dosing of LIDODERM,
the average peak blood concentration is about 0.13 ug/mL, but concentrations
higher than 0.25 ug/mL have been observed in some individuals.
PRECAUTIONS:
General
Hepatic Disease: Patients with severe hepatic disease are at greater risk of developing
toxic blood concentrations of lidocaine because of their inability to metabolize
lidocaine normally.
Allergic Reactions: Patients allergic to para-aminobenzoic acid derivatives (procaine,
tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
However, LIDODERM should be used with caution in patients with a history of drug
sensitivities, especially if the etiologic agent is uncertain.
Non-Intact Skin: Application to broken or inflamed skin, although not tested, may
result in higher blood concentration of lidocaine from increased absorption.
LIDODERM is only recommended for use on intact skin.
Eye Exposure: The contact of LIDODERM with eyes, although not studied, should be
avoided based on the findings of severe eye irritation with the use of similar
products in animals. If eye contact occurs, immediately wash out the eye with water
or saline and protect the eye until sensation returns.
There are many more precautions: Please read your Prescription label and text of
directions and usage.
Drug Interactions
Antiarrhythmic Drugs: LIDODERM should be used with caution in patients receiving
Class I antiarrhymthmic drugs (such as tocainide and mexiletine) since the toxic
effects are additive and potentially synergistic.
Local Anesthetics
When LIDODERM is used concomitantly with other products containing local anesthetic
agents, the amount absorbed from all formulations must be considered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogensis: A minor metabolite, 2.6-xylidine, has been found to be carcinogenic
in rats. The blood concentration of this metabolite is negligible following
application of LIDODERM.
Mutagenesis: Lidocaine HCI is not mutagenic in Salmonella/mammalian microsome test
nor clastogenic in chromosome aberration assay with human lymphocytes and mouse
micronucleus test.
Impairment of Fertility:
The effect of LIDODERM on fertility as not been studied.
Pregnancy
Teratogenic Effects: Pregnancy Category B.
LIDODERM (lidocaine patch 5%) has not been studied in pregnancy, Reproduction studies
with lidocaine have been performed in rats at doses up to 30 mg/kg subcutaneously
and have revealed no evidence of harm to the fetus due to lidocaine. There are,
however, no adequate and well-controlled studies in pregnant women. Because
animal reproduction studies are not always predictive of human response, LIDODERM
should be use during pregnancy only if clearly needed.
Labor and Delivery
LIDODERM has not been studied in Labor and delivery. Licocaine is not contraindicated
in labor and delivery. Should LIDODERM be used concomitantly with other products
containing lidocaine, total doses contributed by all formulations must be
considered.
Nursing Mothers:
LIDODERM has not been studied in nursing mothers. Lidocaine is excreted in human
mild, and the milk: plasma ratio of lidocaine is 0.45 Caution should be exercised
when LIDODERM is admistered to a nursing woman.
Pediatric USE
Safety and effectiveness in pediatric patients have not been established.
ADVERSE REACTIONS
Localized Reactions
During or immediately after treatment with LIDODERM (lidocaine patch 5%), the skin at
the stie of treatment may develop erythema or edema or may be the locus of abnormal
sensation. These reactions are generally mild and transient, resolving
spontaneously within a few minutes to hours. In clinical studies with LIDODERM,
there were no serious reactions reported. One out of 150 subjects in a three-
week study was discontinued from treatment because of a skin reaction
(erythema and hives).
Allergic Reactions:
Allergic and anaphylactoid reactions associated with lidocaine, although rare, can
occur. They are characterized by urticaria, angioedema, bronchospasm, and shock.
If they occur, they should be managed by conventional means. The detection of
sensitivity by skin testing is of doubtful value.
Systemic (Dose-Related) Reactions
Systemic adverse reactions following appropriate use of LIDODERM are likely, due to
the small dose absorbed (See CLINICAL PHARMACOLOGY, Pharmacokinetics), Systemic
adverse effects of lidocaine are similar in nature to those observed with other
PHARMACOLOGY, Pharmacokinetics). Systemic adverse effects oflidocaieare similar in
nature to those observed with other amide local anesthetic agents, including CNS
excitation and/or depression (light-headedness, nervousness, apprehension, twitching,
tremors, convulsions, unconsciousness, respiratory depression and arrest).
Excitatory CNS reactions may be brief or not occur at all, in which case the
first manifestation may be drowsiness merging into unconsciousness. Cardiovascular
manifestations may include bradycardia, hypotension and cardiovascular collapse
leading to arrest.
OVERDOSAGE:
Lidocaine overdose from cutaneous absorption is rare, but could occur. If there is
any suspicion of lidocaine overdose (see ADVERSE REACTIONS, Systemic Reactions), drug
blood concentration should be checked. The management of overdose includes close
monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible
value in the treatment of acute overdose with lidocaine.
In the absence of massive topical overdose or oral ingestion, evaluation of symptoms
of toxicity should include consideration of other etiologies for the clinical effects,
or over dosage from other sources of lidocaine or other local anesthetics.
The oral LD50 of lidocaine HCI is 459 (346-773) mg/kg (as the salt) in non-fasted
female rats and 214 (159-324) mg/kg (as the salt) in fasted female rats, which are
equivalent to roughly 4000 mg, respectively, in a 60 to 70 kg man based on the
equivalent surface area dosage conversion factors between species.
DOSAGE AND ADMINISTRATION:
Apply LIDODERM to intact skin to cover the most painful areas. Apply up to three
patches, only once for up to 12 hours within a 24-hour period. Patches may be cut
into smaller sizes with scissors prior to removal of the release liner. Clothing
may be worn over the area of application. Smaller areas of treatment are recommended
in a debilitated patient, or a patient with impaired elimination.
If irritated or a burning sensation occurs during application, remove the patch(es)
and do not reapply until the irritation subsides.
When LIDODERM is used concomitantly with other products containing local enesthetic
agents, the amount absorbed from all formulations must be considered.
HANDLING AND DISPOSAL:
Hands should be washed after the handling of LIDODERM, and eye contact with LIDODERM
should be avoided. The used patch should be immediately disposed of in such a way
as to prevent its access by children and pets.
HOW SUPPLIED:
LIDODERM (Lidocaine patch 5%) is available as the following:
Carton of 30 patches, packaged into individual child-resistant envelopes
Store at 25C (77 degrees) excursions permitted to 15 to 30 Celsius (59 degree to
86 degree farenheight) See USP Controlled Room Temperature).
Manufactured for:
Endo Pharmaceutical Inc. ENDO
Chadds Ford, Pennsylvania 19317
LIDODERM is a Registered Trademark of Hind Health Care, INC.
=============================================================================
A pressure point procedure found on the internet to help another patient
of piriformis problems in which the Piriformis Muscle needed to be stretched
out back to its original length -- Here is the therapy for that below:
=============================================================================
Sciatica? Piriformis? This helped me
Link
This article submitted by Larry Swain on 1/20/99.
Email Address: swainl@vitrex.net
http://neuro-www.mgh.harvard.edu/forum/ChronicPainF/1.20.992.58AMSciaticaPiriformi/
I would like to pass along something that has worked very well for me and I hope
that it will help some of you out there suffering from lower back problems and
sciatica as I was.
I have had very bad back problems for the past 15 years that have nearly
incapacitated me. I was diagnosed with degenerative disk disease, 4 herniated
disks and a badly bulged disk which made life unbearable. I had sciatic pain so
bad that many days I couldn't walk without a cane and at night I would get a
numbness and tingling in my legs that nearly drove me crazy.
I went to many doctors, neurosurgeons etc. and they tried all kinds of pain killers,
direct injections into the muscles, etc. with no help at all. A few years ago I tried
deep tissue massage therapy and that has really helped keep the pain to a level that
I can tolerate.
About 7 months ago I learned about some techniques they are using in a pain clinic
in England and I had my therapist try some of them on me with great results. I found
out that a lot of my lower back pain came from a compressed piriformis muscle.
I would like to pass one of these treatments along to you sciatica and piriformis
sufferers and hope that it will help some of you out there. If you have a spouse or
friend that can apply it to you it doesn't cost anything, it's non-invasive and if
it doesn't work you won't be any worse off than you were. My therapist has tried it
on a number of people and it has helped most all of them.
This treatment is so simple that I thought that it was a joke and I didn't try it
until I was in such pain that I would try anything to relieve it. It needs another
person to apply the treatment and it can be a spouse, friend or therapist. There are
two treatments for the piriformis release and I will try to describe them as best and
simply as I can.
The piriformis muscle is a small muscle not much larger than your thumb and it
runs from the top of the leg bone across the buttock to the sacrum which is at the
base of the spinal column. When this little muscle gets irritated due to over use
from sitting, bending or whatever it can compress and pinch the sciatic nerve and
the attachment points are stretched to the limit causing a great deal of pain.
Sometimes it is very difficult to get this muscle to relax and resume its normal
length and that is what this treatment will help with.
Sciatica is a fairly common disorder and approximately 40% of the population
experiences it at some point in their lives. However, only about 1% has coexisting
sensory or motor deficits. Sciatic pain has several root causes and treatment may
hinge upon the underlying problem.
Chronic pain may arise from more than just compression on the nerve. According
to some pain researchers, physical damage to a nerve is only half of the equation.
A developing theory proposes that some nerve injuries result in a release of
neurotransmitters and immune system chemicals that enhance and sustain a pain
message. Even after the injury has healed, or the damage has been repaired, the
pain continues. Control of this abnormal type of pain is difficult.
You will need a firm padded surface to lay the patient on. A table or the floor
with a 3" or 4" foam pad works well. A bed has too much give to it.
Treatment #1
Have the patient lay on their side facing away from you with their legs pulled up to
a comfortable position and one on top of the other.
(optional) Hot moist towels placed on the buttock and hip muscles for about 15 minutes
sure feels good and helps to relax the muscles. Moist heat seems to penetrate deeper
into the muscles. Be careful not to get it hot enough to burn the skin or be
uncomfortable.
If the patient is laying on their right side, facing away from you, place the heel of
your right hand in the middle of the buttock muscle and lean into it and hold it. With
your left hand grasp their foot or ankle and lift it straight up about 12"" rotating
the leg . This will probably be painful so be careful of your patient's pain threshold.
Gently lay the foot and leg back down and release the pressure with the right hand.
Apply the pressure with the right hand , lift the leg , gently lower it, release the
pressure.
Go through this same sequence for about 15 minutes working your hand up and down the
hip and buttock muscles then turn the patient over on the other side and repeat the
steps. If this length of time is too much for the patient just do it for a couple of
minutes to start and try to work up to a longer time.
Treatment #2
Working the right side
Have patient lay on stomach.
Move to the right side of patient.
Grasp the ankle and lift the lower part of the leg so that the bottom of the foot is
pointing straight up.
Push the foot away from you as if you were trying to touch the heel to the left buttock
muscle to rotate the leg. Be sure to monitor the patient's pain level and not overdue
it.
Place the heel of the hand in the middle of the buttock muscle as in treatment #1 and
lean into it to apply pressure.
While applying pressure with the right hand, pull the leg back toward you to the
starting position.
Release the pressure with the right hand.
Push the leg away from you, apply pressure with the right hand, and pull leg toward you,
release the pressure with the right hand.
Continue this sequence for the same time as in treatment #1 and then move to the other
side of the body and work it in the same way.
You can work each of these treatments as an individual treatment or you can work both
of them in a single session. The total time should be about 30 minutes for the whole
treatment.
Some effects of it may show up after the treatment but the real effects take about 11
to 12 hours to really set in. After the first 3 or 4 rotations the muscle will try to
return to its compressed state but after 10 or 12 rotations it will gradually start to
lengthen out little by little until it reaches its normal length. This treatment may
need to be done for 3 or 4 sessions a couple of days apart for the maximum effect.
I hope this treatment will help some of you as much as it has helped me. Good luck to
you all in finding cure for your ailments. God Bless.
=============================================================================
FULL DISCLAIMER
=============================================================================
Sciatica Org Site: Link
Functional Entrapments: What are they?
Functional entrapment syndromes are defined as significant neurological compression
resulting from positional or kinesiological considerations, not solely structural
or inflammatory conditions.
For this reason, imaging studies such as MRI, CT, bone and gallium scans and
diagnostic ultrasound is of limited value in detecting these conditions. Even
conventional EMG is often negative. Rather, it is in comparing nerve conductions
in the anatomical position with nerve conductions in the symptomatic position that
turns up the pathology, and the pathogenetic mechanism. This offers both guidance
on effective treatment, and a means of assessing the efficacy of treatment through
repeated serial testing of the same nerve conductions.
Rehabilitation Medicine is well-suited to work with these common causes of pain,
since PM&R knows anatomy and kinesiology, does electro diagnostic testing as an
extension of the physical exam, is functionally oriented, and is comfortable using
both injection and physical therapeutic techniques in treatment.
Examples:
Piriformis syndrome comprises approximately 6 to 8 percent of sciatica and low back
pain. (1) While herniated nucleus pulpous and spinal stenosis are more common,
piriformis syndrome is under diagnosed, (2). Therefore, its prevalence is significantly
higher than its incidence (3).
The syndrome is due to the piriformis muscle compressing the sciatic nerve in the
buttock, and, like pronator syndrome or carpal tunnel, causing damage to the peripheral
nerve through excessive pressure. (4) The nerve is pressed backward against the sharp
tendinous edges of other muscles such as the gemellus superior and obturator internus,
(5-6) and the condition may easily become chronic, and debilitating.
History
Discovered in Florence ca. 1580. After Mixter and Barr's paper in 1932 (7), people
recognized spinal and intramedullary pathology as the chief cause of sciatica. It
is foraminal and intramedullary conditions that come to mind when patients present
with sciatica. However, pain along the course of the sciatic nerve at times is caused
by pathological involvement of the nerve itself, and rational diagnosis and treatment
then should focus on the site of the pathology.
Epidemiology
Since an estimated 80 million Americans suffer low back pain and sciatica annually,
(8) 4.8 to 6.4 million people contract piriformis syndrome annually. One reason for
Under diagnosis is that MRI, myelogram, CT, are unlikely to turn up any evidence of
piriformis syndrome. (9-11) It is a functional syndrome: only certain positions and
pressures bring out the pain, paresthesias, and weakness that come with it. Structure
imaging studies are of minimal value here. (12-15)
Since it is sometimes considered a diagnosis of exclusion, many patients receive
painful and pointless surgical and other procedures based on limited inquiries and
faulty diagnosis.
Piriformis Syndrome is commonest among very active people such as athletes, health
club users, joggers, and performers, and those who sit a great deal such as members
of the financial community, lawyers, psychotherapists, secretaries and vehicular drivers
. After occupational causes, trauma is the second greatest cause of piriformis syndrome.
Lifting and other back strain related activities are third, with many other initiating
events including misplaced gluteal injections, lipomas, and unusual furniture.
Diagnosis
Modern methods of diagnosis began with the work of Fishman and Zybert (14) using the
H-reflex and EMG in 1992. By timing the H-reflex in the position of Flexion Adduction
and Internal Rotation, (the FAIR-test) in which the piriformis muscle tightly presses
the sciatic nerve against the underlying structures, and comparing the timing with
the H-reflex in the anatomical position, the amount of delay was measured in normals.
These values were then compared to those seen in patients meeting clinical criteria
for piriformis syndrome. Patients with piriformis syndrome had FAIR-test values which
were, on the average, more than three standard deviations beyond the mean seen in
normals and in contra lateral lower extremities. More than 80 percent of patients so
diagnosed improved 50 percent or more with conservative therapy aimed at loosening
the piriformis muscle in the buttock. The recovery rate of patients identified by
the FAIR-test is much greater than the recovery rate seen in patients selected by
any other known means. (15)
Because of the nature of the syndrome, the test for piriformis syndrome is functional
in nature, comparing nerve conduction values when the nerve is compressed, with values
seen in a resting position. The discrepancy between normal values and those seen in
piriformis syndrome is amplified by the fact that the H-reflex crosses the buttock
In order to determine these values, posterior tibial and peroneal H-reflexes are studied
both in the anatomical position and the flexed adducted internally rotated position
(FAIR-test). Thus the H-reflex is actually performed four times with each limb that
is studied. (15)
Clinical Experience
Treatment at first was simply physical therapy, informed and enriched by the generous
giving forth of experience from the international medical community. In essence, the
therapy lengthened the piriformis muscle, reducing spasm and pressure on the descending
sciatic nerve, and giving the nerve enough slack to remove itself from harm's way. See
the rest of the website for the specific program. The therapy was helpful, but progress
was slow. On the suggestion of Dr. Janet Travell, we began injecting Triamcinolone
Acetonide 20mg with 1.5cc of 2% lidocaine into the motor point of the piriformis muscle,
just medial to its musculotendinous junction in the lateral buttock.
This had only rare minor and transient side-effects on non-diabetics, and shortened
the recovery time considerably.
On average 10.2 month follow-up time of 1014 cases of piriformis syndrome, more than
hat these patients had suffered from piriformis syndrome for an average of 6.2 years,
Probably due to piriformis syndrome being considered a diagnosis of exclusion, other,
less important diagnostic entities had received undue attention in these patients.
Among these1014 cases there had been over 400 spinal, trochanteric and gynecological
surgeries, none of which was definitive, more than 1500 imaging studies, of which
less than 1/5 were relevant, and more than 10,000 appointments with clinicians for
diagnostics, epidurals, physical therapy, and alternative methods of pain relief.
More recently we have conducted several IRB-approved studies of more specific nerve
blocks, using the toxin of the botulinum bacterium. In the latest and most successful
of these, we have found that 12,500 units of botulinum B toxin has well above 85%
efficacy, and fewer side effects than Triamcinolone and Lidocaine, giving more relief
faster, and appearing in early studies to last longer. Containing no steroid, this
preparation is also suitable for diabetics. Showing a much more rapid decline in pain
levels, and normalization of the FAIR-test, it obviates physical therapy sessions that
surpass the cost of the injection.
In summary, there are four reasons that botulinum toxin helps in the treatment of
piriformis syndrome.
A reliable correlation between diagnosis and effective treatment exists.
More than 5,000,000 currently improperly treated patients will continue to suffer, and
continue to consume health care resources in vain unless and until adequate treatment
is afforded them. In clinical experience, injection of botulinum toxin has proven the
most effective treatment.
Cost-benefit analysis of current data strongly supports injection of botulinum toxin
in the treatment of piriformis syndrome.
Two other considerations are relevant:
Wider applicability. While the anti-insulinemic effect of steroids strongly
contraindicates their use in diabetic patients, there are virtually no documented
allergic reactions to botulinum toxins.
Longer efficacy. Steroid injection without physical therapy is generally effective for
1-3 weeks. Botulinum toxin injections without physical therapy are effective for at
least three months. In the past, approximately 15% of patients treated without botulinum
toxin injections have had recurrence of piriformis syndrome within three years. As of
today, (14 months after our first injection) we have seen 3 relapses following botulinum
toxin injections in 61 patients.
A Patients Success Story: Link
Cindy W., IT manager from NC.
Successful ADR, but I was still completely disabled.
The first time I met Mark was on September 19, 2002. We were in the waiting room at
the Alpha Klinik and we both had surgery scheduled for the next day. After we chatted
for a while, I realized that I was speaking to someone who had written a great deal on
the internet about his research into ADR. I said, "Oh my gosh, you are RumorSlayer!
I used to look for you online. I'd call my husband over. Ed, Ed, he's here again!!!
Come read this!"
I was in Munich for surgery because I had disabling back pain, hip pain and foot pain.
I was very relieved after my discogram because it so clearly reproduced all my pain.
That made me an excellent candidate and gave me every reason to be hopeful.
My first week post-op was incredible. I felt sorry for Mark because he was having such
a tough post-op experience, while I was walking many miles a day and sightseeing around
Munich just 5 or 6 days after my surgery. I knew just a few days after my surgery that
my back pain and my foot pain were GONE!
Fast forward about a year and Mark's in great shape, but I was still functionally
disabled. Although my disc replacement solved my back and foot pain, my disabling
hip pain still had me unable to function. I was still on large doses of OxyContin.
I'd been to doctor after doctor, but none of them had any good ideas. I had been
referred to pain management. I was ready to give up.
One day Mark called me up and told me about someone he met on the Internet forum he'd
started for people who want to discuss non-fusion technologies. He told me that I there
was a man he'd spoken with, who described disabling hip pain EXACTLY like I described
mine. I took Mark's advice and called Brian. Brian had a similar story, but had
found his way to a Dr. in Cincinnati who specialized in Piriformis syndrome. I
called the Dr. but he warned me that Piriformis syndrome is very rare and that I
shouldn't get my hopes up.
Fast forward another 6 or 7 months! It turned out that I had profound PS.
Out of 80 cases this doctor had seen, he said that my case was certainly one of
the worst. I had the piriformis release surgery in October of 2003 and by mid-2004,
I was riding my mountain bike with my husband, camping, hiking, working full time,
back to a rewarding workout regimen (I was an athlete before my disability). I
can't believe it, I'm living a NORMAL LIFE! I was ready to give up. I don't know
where I'd be now if it wasn't for Mark and his Patient Network. I suppose that I'd
still be in pain management, on large doses of opiates and completely disabled.
Instead, I have a new lease on life and can live every day to the fullest. With
the perspective that you gain from being reborn after such a painful disability,
life is even better than it was before I could truly appreciate what it means to
enjoy a day without pain!
Thanks
==================================================================================
Sciatic Notch lesser sciatic notch
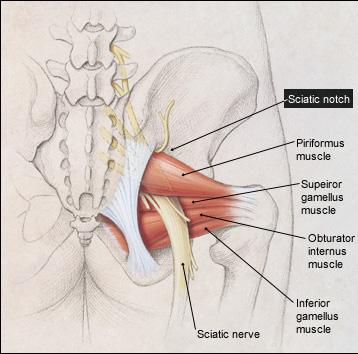
 =================================================================================
(April 8, 2005)
Email to Paul Dean from Northern California Sufferer:
hi,
I have had a neurogram and it shows that both my sciatic nerves are being pinched
at the sciatic notch. Is their any advise you could give me. I live in Northern
California and the doctors up here pretty much suck and really don't believe
piriformis syndrome exists. who did you do to and what tests did you do to determine
you had piriformis syndrome.
THANKS
==================================================================================
Piriformis Surgery Incision (Site)
Of a Patient Suffering from Left Side
Piriformis Syndrome and Sciatica
=================================================================================
(April 8, 2005)
Email to Paul Dean from Northern California Sufferer:
hi,
I have had a neurogram and it shows that both my sciatic nerves are being pinched
at the sciatic notch. Is their any advise you could give me. I live in Northern
California and the doctors up here pretty much suck and really don't believe
piriformis syndrome exists. who did you do to and what tests did you do to determine
you had piriformis syndrome.
THANKS
==================================================================================
Piriformis Surgery Incision (Site)
Of a Patient Suffering from Left Side
Piriformis Syndrome and Sciatica
 The incision is to the Buttock
(April 8, 2005)
Email Reply From Paul Dean to Northern California Sufferer:
The nerve narrowing at the sciatic notch is a different part of the body and
is near the spinal cord and structure which (IS NOT) Piriformis Syndrome, which
lies deep underneith the Buttock underneith your gluteal muscles. Your Sciatic
notch may need to be enlargened because it should not be pinching any of the
nerves. Nerves need to move freely as they are stretched in walking, etc. If
they cannot move or if they are pinched, you will be in great pain.
It is very hard to find a doctor who knows where your pain is coming from. Especially
in Piriformis Syndrome. A Orthopaedic doctor can go an entire career without
seeing more than one or two cases of Piriformis Syndrome in his career.
Call Dr. Chambi, (Neurosurgeon) (714)-973-0810 and explain your situation to him.
He is the only one who could find my problem of many, doctors who had seen me.
In my case, the Piriformis muscle had scar tissue wrapped around the sciatic nerve,
entrapping that nerve and giving me pain. That scar tissue has been removed by
Dr. Chambi and I am getting good results, but it takes time for a sciatic nerve to
get back to normal.
Good luck, I feel for all of those who have had the intense pain that I have had!
As a final comment. I chose the Doctor that the Pro Athletes prefer, because you
need the best of the best for good results.
I am a patient recovering like yourself and every situation will be different and
your exact situation sounds a little bit different than mine.
The diagnosis of Piriformis Syndrome is a situation of exclusion of any Spinal
problems. Also, if your pain lies in the middle of your buttock and comes about
when you are sitting, this is one sign that you may have Piriformis Syndrome.
You could have numbess, Sharp stabbing Pain, burning pain, or Aching Pain, along
with sciatica.
When it is found that your problem is not coming from the spine, then the surgeon
will look else where for the problem. The situation becomes confusing when the
spine has exactly the same symptoms of the Piriformis entrapment, (In my case,
sciatica down the right leg). This is when the MRI will exclude any type of
abnormal discs that may have ruptured or narrowed or had entrapped the nerve.
I am post disc surgery and post Piriformis Release surgery at this time. As
long as you have entrapment, no amount of exercise or stretches are going to
change that entrapment. It is after these failed exercises and stretches that
one may go for a release surgery.
As a last note, find the very best neurosurgeon that you can, (even if it means flying
to that doctor) who is familiar with your diagnosis and possible surgery solutions.
Different Doctors specialize in different things and they don't know much about
other conditions and they only look at what they know. A spine surgeon only
likes to give spine surgeries... etc. etc. So you really need a specialist who
deals with your type of problem all day long and I think you are on the right
track. Your age and type of fall that you might of had would also help in diagnosis
of your injury. Family history and many other questions are needed to be
answered to get to the bottom of your situation. Your body will give you
an idea of where the pain is coming from which is helpful in the diagnosis.
Hope some of the above helps you! See a good Neurosurgeon to confirm
any of the above I have mentioned. Of course I cannot prescribe or give advice
because I am not a Doctor. But I guess everybody has an opinion.
Thanks,
Paul, Recovering Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
=============================================================================
Piriformis Surgery Questions and Answers:
The incision is to the Buttock
(April 8, 2005)
Email Reply From Paul Dean to Northern California Sufferer:
The nerve narrowing at the sciatic notch is a different part of the body and
is near the spinal cord and structure which (IS NOT) Piriformis Syndrome, which
lies deep underneith the Buttock underneith your gluteal muscles. Your Sciatic
notch may need to be enlargened because it should not be pinching any of the
nerves. Nerves need to move freely as they are stretched in walking, etc. If
they cannot move or if they are pinched, you will be in great pain.
It is very hard to find a doctor who knows where your pain is coming from. Especially
in Piriformis Syndrome. A Orthopaedic doctor can go an entire career without
seeing more than one or two cases of Piriformis Syndrome in his career.
Call Dr. Chambi, (Neurosurgeon) (714)-973-0810 and explain your situation to him.
He is the only one who could find my problem of many, doctors who had seen me.
In my case, the Piriformis muscle had scar tissue wrapped around the sciatic nerve,
entrapping that nerve and giving me pain. That scar tissue has been removed by
Dr. Chambi and I am getting good results, but it takes time for a sciatic nerve to
get back to normal.
Good luck, I feel for all of those who have had the intense pain that I have had!
As a final comment. I chose the Doctor that the Pro Athletes prefer, because you
need the best of the best for good results.
I am a patient recovering like yourself and every situation will be different and
your exact situation sounds a little bit different than mine.
The diagnosis of Piriformis Syndrome is a situation of exclusion of any Spinal
problems. Also, if your pain lies in the middle of your buttock and comes about
when you are sitting, this is one sign that you may have Piriformis Syndrome.
You could have numbess, Sharp stabbing Pain, burning pain, or Aching Pain, along
with sciatica.
When it is found that your problem is not coming from the spine, then the surgeon
will look else where for the problem. The situation becomes confusing when the
spine has exactly the same symptoms of the Piriformis entrapment, (In my case,
sciatica down the right leg). This is when the MRI will exclude any type of
abnormal discs that may have ruptured or narrowed or had entrapped the nerve.
I am post disc surgery and post Piriformis Release surgery at this time. As
long as you have entrapment, no amount of exercise or stretches are going to
change that entrapment. It is after these failed exercises and stretches that
one may go for a release surgery.
As a last note, find the very best neurosurgeon that you can, (even if it means flying
to that doctor) who is familiar with your diagnosis and possible surgery solutions.
Different Doctors specialize in different things and they don't know much about
other conditions and they only look at what they know. A spine surgeon only
likes to give spine surgeries... etc. etc. So you really need a specialist who
deals with your type of problem all day long and I think you are on the right
track. Your age and type of fall that you might of had would also help in diagnosis
of your injury. Family history and many other questions are needed to be
answered to get to the bottom of your situation. Your body will give you
an idea of where the pain is coming from which is helpful in the diagnosis.
Hope some of the above helps you! See a good Neurosurgeon to confirm
any of the above I have mentioned. Of course I cannot prescribe or give advice
because I am not a Doctor. But I guess everybody has an opinion.
Thanks,
Paul, Recovering Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
=============================================================================
Piriformis Surgery Questions and Answers:
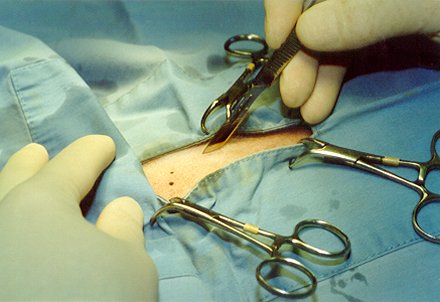 (April 8, 2005) Email Questions to Paul Dean
An Email to Paul Dean from another Person who is considering
Piriformis Release Surgery:
Hello Mr. Dean,
While researching piriformis syndrome on the internet, I ran across your account
of having release surgery done by Dr. Chambi.
My wife is having a great deal of sciatica pain and is currently seeing Dr. Chambi
for piriformis syndrome. After 2 injections with little relief of pain, Dr Chambi
has suggested that surgery might be in order.
Given what you know about this surgery, was it successful in relieving your pain
and would you have Dr Chambi perform it again?
I would be very interested in talking to you further about this subject if you
would consent.
==================================================================================
==================================================================================
Piriformis Surgery Steps:
(April 8, 2005) Email Questions to Paul Dean
An Email to Paul Dean from another Person who is considering
Piriformis Release Surgery:
Hello Mr. Dean,
While researching piriformis syndrome on the internet, I ran across your account
of having release surgery done by Dr. Chambi.
My wife is having a great deal of sciatica pain and is currently seeing Dr. Chambi
for piriformis syndrome. After 2 injections with little relief of pain, Dr Chambi
has suggested that surgery might be in order.
Given what you know about this surgery, was it successful in relieving your pain
and would you have Dr Chambi perform it again?
I would be very interested in talking to you further about this subject if you
would consent.
==================================================================================
==================================================================================
Piriformis Surgery Steps:
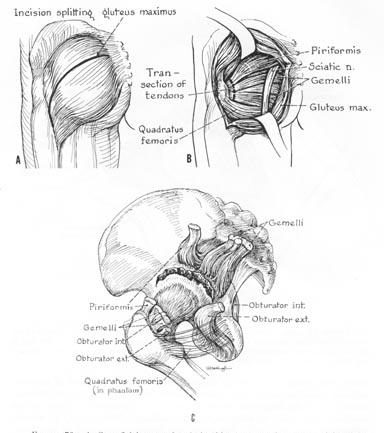 Email Answer from Paul Dean: (April 8, 2005)
Dear Sir,
Yes I did the Buttock Lidocaine shots and only the first of a series of three
helped me. I was still in a lot of pain and the only alternative at that point
was the actual Piriformis Release Surgery.
I had worn out the physical therapy option, and wasn't getting any better.
It was either have the pirifromis release surgery or always be in terrible pain.
I did not want to live the rest of my life in terrible pain so I went for the
piriformis release surgery.
Within two months after the surgery I was ALOT better. That alone helped me
very much, and my depression started to lift as well. When a person is injured
for a long time it is very hard to keep a positive frame of mind, but this
is essential in getting better.
Nerve
Email Answer from Paul Dean: (April 8, 2005)
Dear Sir,
Yes I did the Buttock Lidocaine shots and only the first of a series of three
helped me. I was still in a lot of pain and the only alternative at that point
was the actual Piriformis Release Surgery.
I had worn out the physical therapy option, and wasn't getting any better.
It was either have the pirifromis release surgery or always be in terrible pain.
I did not want to live the rest of my life in terrible pain so I went for the
piriformis release surgery.
Within two months after the surgery I was ALOT better. That alone helped me
very much, and my depression started to lift as well. When a person is injured
for a long time it is very hard to keep a positive frame of mind, but this
is essential in getting better.
Nerve
 Now 10 months later I continue to improve. I could not improve at all without the
piriformis release surgery. What happened is when I fell at work, a large amount
of scarring was attached to the piriformis muscle area and to the sciatic nerve
making it impossible for the nerve to move. If the sciatic nerve cannot move, you
will have terrible pain.
Yes, I was scared to have the release, but not as scared as when I had my
back surgery.
Would I do it again? Every day of the week, I would. Quality of life is very important
to me and I need to be able to be active as I once was and now I have the opportunity
to get back to being active.
Piriformis Syndrome is very rare and most Doctors know nothing about it. You have
a doctor, Dr. Chambi, who understands this condition, so you are very lucky to find
somebody who understands where your pain is actually coming from.
Post Op: I have lost a great deal of elasticity in the nerve so I must walk and
stretch every day to regain what I can in that sciatic nerve elasticity.
Rehab. is very important and takes a long time to get the nerve back into
shape. Stretching, Walking and Light water exercises.
Structure Of A Nerve
Now 10 months later I continue to improve. I could not improve at all without the
piriformis release surgery. What happened is when I fell at work, a large amount
of scarring was attached to the piriformis muscle area and to the sciatic nerve
making it impossible for the nerve to move. If the sciatic nerve cannot move, you
will have terrible pain.
Yes, I was scared to have the release, but not as scared as when I had my
back surgery.
Would I do it again? Every day of the week, I would. Quality of life is very important
to me and I need to be able to be active as I once was and now I have the opportunity
to get back to being active.
Piriformis Syndrome is very rare and most Doctors know nothing about it. You have
a doctor, Dr. Chambi, who understands this condition, so you are very lucky to find
somebody who understands where your pain is actually coming from.
Post Op: I have lost a great deal of elasticity in the nerve so I must walk and
stretch every day to regain what I can in that sciatic nerve elasticity.
Rehab. is very important and takes a long time to get the nerve back into
shape. Stretching, Walking and Light water exercises.
Structure Of A Nerve
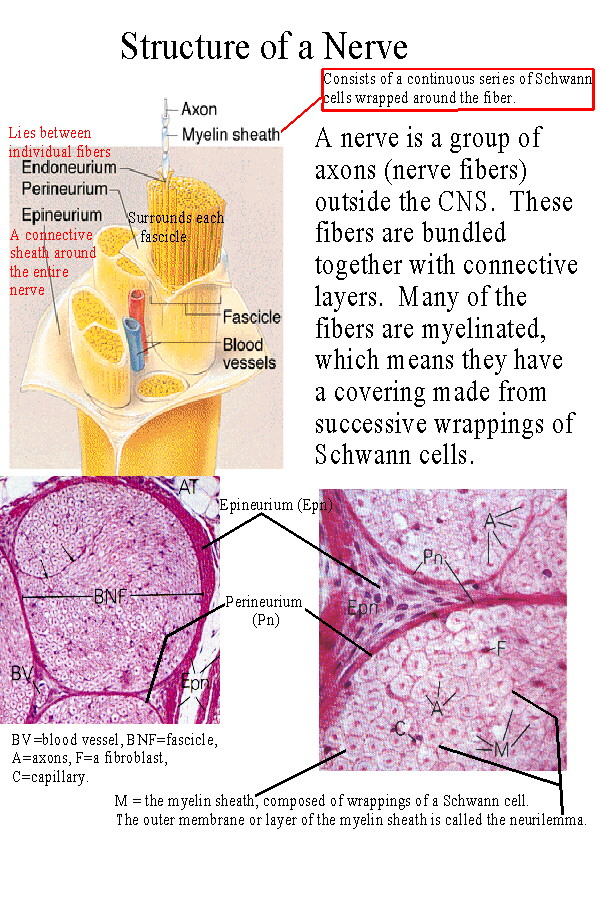 A final note:
I was at the point where I felt I had nothing to lose so I went ahead with the surgery,
and it helped a great deal. My L5 S1 Lower discectomy surgery also helped me very
much. (I had a 7mm Herniated Disk)
Good luck to you and your wife, and again, think of quality of life, and of getting
better because sometimes physical therapy will do you no good when the scarring is so
severe that your sciatic nerve cannot move.
I am up to walking an hour and the extreme edge of pain is gone!!!
Of course I am not a Doctor so I cannot give advise but only opinions as to my
unique situation, and every situation is different.
Dr. Chambi is the doctor that all the Pro Athletes choose and there must be a reason
for that.
Take care,
I hope that you recover soon!
Paul Dean, Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
==================================================================================
Side Note: July 23, 2005 - Paul Dean
I am continuing to recover at my own body's rate which seems to be a little bit
slow but you really can't recover at any pace faster than your own natural
pace of healing. Nerves take up to three years to have their full healing ability.
So do not be to impatient if the second you get off the operating table that you
are not completely healed. That just isn't how nerves work if they have been damaged
for a long time. The problem is that once your sciatic nerve in your hip has
been entrapped at the piriformis level for several years, the elasticy shrinks
and you will hurt every time you stretch until you get your nerve elasticy back.
This is the reason that you need to walk an hour or more every day to get that
elasticty back. It will hurt to walk long distances and that is why I use the
Lidocaine patch. This patch numbs the area that hurts in the back of the hip,
so you can walk further and stretch the sciatica nerve.
Rubber band Analogy:
I can imagine a rubber band that needs another inch or two in order to reach
its full potential of stretch. So every day I walk, and then I walk some more,
stretching that rubber band, which is the sciatic nerve. Once the nerve is used
to the stretch it doesn't hurt as much. Of course this is done after the
surgery because the sciatic nerve could not stretch at all when it was tethered
down from tissues wrapped around it from a fall accident I had from work. Now
that there is no entrapment of the nerve I am gently stretching that nerve
until it gets used to the stretch and stops hurting when I walk. The goal
is to have absolutely no pain no matter what I am doing and that is my eventual
goal.
Vitamins B1 and B12 and Antioxidants to build up the Immunity and Healing:
What about boosting the immunity system to have a faster healing process?
I am on a Vitamin Regiment of B1 Vitamin and B12 Vitamin in decent doses as
well as an Anti-oxidant supplement to get my system in good working order so
that I can heal as fast as possible.
I have tried to increase the rate of healing by getting toxins out of my
system by doing the following:
Do's:
Vitamin B (B1) (B12) Vitamin A,B,C,E Beta Carotene and Mineral Supplements.
Drink Six glasses of water a day
Drink as much Grapefruit juice (no Sugar) as possible
Eat as many raw fruits and vegetables as possible
Chicken and Fish
Dont's:
No Salt and No Sugar need to be eaten it is in your foods already.
No Greasy Processed Foods
No Fast-food
No Breads or rice or potatoes
Please see a Doctor before using these above techniques which I am
following as your medications may require that you do not follow
my above plan for getting your system back into shape for quicker healing.
Note: These above Do's and Don'ts can be found in the book of President Clintons
Doctor: Michael F. Roizen, MD. and Mehmet C. Oz, MD copyright 2005,
"YOU, THE OWNER'S MANUAL", The insider's guide to the body that will make
you healthier and younger. Harpercollins Publishers Inc, 10 East 53rd Street
New York, NY 10022.
I have no affiliation with any of these works and please take all information
as third party opinion and review options with your Doctors before doing
anything with your body. Thank you.
Above Updated: April 8, 2005
------------------------------------------------------------------------------
--------------------------------------------------------------------------------
New Entry: July 25, 2007 - Updated Medical Condition of Post Piriformis Syndrome
with Piriformis Release Surgery and Post Discectomy of L5 S1 Disc.
--------------------------------------------------------------------------------
Email Response to Susan:
--------------------------------------------------------------------------------
July 25, 2007
Hi Susan, (Disclaimer: I am a patient like yourself and am not a Doctor.)
Thank you for reading all of my postings, I'm sure it must have taken awhile to get
through it all. Pain is an interesting thing, in makes you want to read every single
thing you can find out about your pain hoping that you can some how stumble upon the
right information that can give you some pain relief. That is what I did and I am sure
that is also what you are seeking and I am wishing you the best of luck in advance, as
pain can control and ruin a good life that was before pain free.
Susan wrote:
The last update on your progress was quite some time ago. How is the sitting going
now?
Paul's reply:
Yes, the update was quite a while ago mostly because I have been busy back in the
Tradeshow business, which requires lifting heavy amounts of weight for a duration of
time. So, in part I have to say that I have gotten better, because it was unfathomable
before my piriformis surgery that I would be able to excel in either of my heavy lifting
jobs. Lifting in duration and for long periods of time was difficult to impossible
before my surgery. Now to answer the sitting question which is important because my
travel time to and from work is an hour and a half each way most of the time. I still
have pain, but not extreme pain and I can get out of it by putting my car on cruise
control and taking my right leg out of the stretch that is required to press down the
gas peddle. I use cruise control most of the time because my pain is elevated. So now
the next question is how much has my pain level improved since the surgery.
I would say it has gone from a 7 to 8 in pain level down to a 2 and 3 which has given
my life back to me in many ways as I enjoy physical activity with lifting and movies
which last up to 3 hours. I do have problems with movies over 2 hours and will take a
15 minute walk around the lobby during a movie in order to stop my pain. It seems that
almost instantly when the leg is no longer in a bad position of a stretch or just
sitting to long in the theater, the walking relieves the pain instantly. Where is the
pain in the first place, it seems that it is in the thigh area, but before the surgery
I had both buttock an thigh pain. Would I do the surgery over again? Definitely, yes as
my pain levels went down to a livable tolerance level. I am still cautious as to getting
back into tennis as that does a lot of thigh stretching but I will try to see if I can
slowly work back into this great sport that I have loved.
Susan wrote:
I'm at the "I need surgery" stage and am trying to find the best, most experienced
surgeon. I live in Florida and am having a difficult time finding someone in this
area who might be competent to do this specialized procedure. It seems that your
doctor and Dr. Filler are both in California and the thought of sitting on an airplane
for 5 hours, then spending several weeks in a hotel room after surgery is not the best
option. Sciatica and Piriformis Syndrome: Dr. Aaron Filler Santa Monica, CA:Preview Link Other
Dr. Aaron Filler Techniques: Link Link
Paul's reply:
It is hard to find an experienced Surgeon and I would recommend you pick somebody who
is doing this type of surgery day in and day out who has done more than anybody else
especially since you only get one shot at this surgery so you need to go to the best.
I went to Dr. Chambi in Santa Ana, CA, I have heard the name Dr. Filler and I have
also seen a Dr. Palmer In Mission Viejo, CA.
Would I fly 5 hours in order to be close to pain free with the proper surgery, after
having a correct diagnosis? Yes, I would do just about anything to get my previous
life back and feel good again, pain free or close to it. Luckily, my surgeon is only
40 minutes to an hour away.
As far as flying back after a surgery, you should be able to do this after three weeks
post surgery, with help. I was able to walk the day after the surgery but had problems
with Sitting and putting on my clothes and getting around because you are limited when
Recovering from this type of procedure.
Susan Wrote:
I went to NYC and saw Loren Fishman, went through Botox with him, and feel like a
human pin cushion with all of the various injections from various doctors. I even
wanted to try prolotherapy but at least that doctor was honest enough to tell me he
thought it wouldn't help. You're the only person that I've found who has actually had
this surgery so I'm very curious about your long term results. Some of the orthopedic
doc's that I've seen will do surgery but want to cut the entire buttocks to do it
(they all specialize in hip replacements around here). I obviously don't want an
invasive procedure when there are alternatives available. Also, as a curiosity, did
you have involvement of bursitis in the hip and thigh with this? I'm trying to figure
out if it's a side effect or a totally different problem.
Paul's reply:
My condition was that of a post herniated disc surgery called a Discectomy of the L5 S1
region of a previous herniated disk of 7 millimeters. The 7 millimeter herniation was
cut out so the nerve was then again free, which it showed that it was free in the post
MRI, however I still had some severe sciatica pain going from the buttock down the right
back side of thigh which is the area where the sciatic nerve travels.
I then had some steroid injections into the L5 S1 back to relieve any possible
inflammation that might be causing my pain and these injections did not help me with my
pain.
I then saw Dr. Chambi and had three Lidocaine injections to the buttocks where the
pain was at a precise location. The 5 inch needle was inserted and the first one
of the three different injections done on different weeks solved my pain temporarily
and so I thought this was quite a miracle to all of a sudden have no pain after a
buttock shot to the piriformis muscle. When the piriformis muscle was relaxed, I was
pain free. However the pain came back after the shot wore off. I also wore a lidocaine
patch which gave some relief to the area installed such as buttock and back of
leg, but was temporary.
It is at that point that Dr. Chambi said, you have piriformis syndrome because the
piriformis muscle has entrapped your sciatic nerve and there is only one permanent
solution which is a piriformis release. Piriformis Release is a way of cutting away the
piriformis from the sciatic nerve. Apparently, the sciatic nerve had somehow gotten
scarred down from a fall I had, and it was entrapped. After the piriformis was cut away
from the nerve, I had great relief, because the sciatic nerve could then move freely
again. It was no longer pinched down, and was not constricted any longer by the
piriformis muscle.
Susan wrote:
Some of the orthopedic doc's that I've seen will do surgery but want to cut the entire
buttocks
Paul's reply:
The actual cut that the surgeon does for piriformis release is similar to the cut
done in a hip replacement at about a 4 to 5 inch cut across the buttock. The
piriformis nerve is about 6 inches down and a lot of the Buttock area needs to
be moved away to be able to get to the piriformis muscle and underneath were the
sciatic nerve is located.
Susan wrote:
I obviously don't want an invasive procedure when there are alternatives available.
Paul's reply:
You first try all the physical therapy and water therapy and all the different shots
available but when they all fail, then you look to the surgery for a permanent cure,
and only after at least two experts agree with the same diagnosis, in this case,
piriformis syndrome, then you take the next step, if both doctors agree that this is
the next step to take after exhausting all other steps, and needing a permanent
solution. You should not be afraid of surgery when you are with an expert in the field.
Do not be afraid of the recovery pain as you are given strong pain killers to take this
pain away until you have finally recovered.
Finally, make sure that you have gotten relief with the Lidocaine injection which
relaxes the piriformis muscle and gives relief to the sciatic nerve, which pretty much
is the telling sign that the piriformis muscle is involved in your pain. Many
Orthopedic Doctors will say this is not the case because the do not understand that the
piriformis muscle and scarring can stop the sciatic nerve from functioning properly.
I suggest you see Doctors that study Nerves and not just bone doctors as your problem
May not be a bone or disc disease.
The most important thing to find is the right Doctor and the correct Diagnosis, and it
won't be easy to find this.
Susan Wrote;
Did you have involvement of bursitis in the hip and thigh with this? I'm trying to
figure out if it's a side effect or a totally different problem.
Paul's reply:
No I was not diagnosed with bursitis in the hip or thigh. That may very well be
something else. This is why it is important to get the proper diagnosis and to see
more than one specialist no narrow down where and what your pain is and what is causing
it. You can go to three different specialists and get three different expert opinions,
and this is a big problem in figuring out what to do next, so you'll have to find the
best of the best in specialists in order to get a correct diagnostics of your problem.
Even a phone consultation is better than nothing, so I suggest that you keep searching
for a correct diagnosis and then go forward with the proper treatment once this is
found.
Hope is one thing we all have even when things look bad. You keep on thinking
that you will wake up and be pain free. Maybe this sounds unrealistic but we
keep on holding on to this hope. Can nerves regrow themselves and straighten
themselves out so that signals are then properly sent to and from the body
to the brain? We hope that some how this will happen, however sometimes nerves
don't grow back so we are stuck with tollerating pain. Then, it is up to us to
figure out what we are going to do with this pain and how to tempoarily get out
of pain. To each person they have their own answers. My answer is to keep going.
My Disclaimer: I am not a Doctor and am not in a related medical field and am only a
patient looking for a solution to pain. Do not take anything I say as a fact, but
instead contact your local specialist and get the correct diagnosis from a professional.
I sincerely hope you are pain free soon, from one patient to another, Good luck with a
pain free life.
Thank you,
Paul
knowledge is Power
Thank you,
Paul Dean, Spy Hunter Video Game (Guinness Book) Champion - June 28, 1985 and
2007 Guinness Book
www.spyhunter007.com
Last Updated: April 8, 2005
A final note:
I was at the point where I felt I had nothing to lose so I went ahead with the surgery,
and it helped a great deal. My L5 S1 Lower discectomy surgery also helped me very
much. (I had a 7mm Herniated Disk)
Good luck to you and your wife, and again, think of quality of life, and of getting
better because sometimes physical therapy will do you no good when the scarring is so
severe that your sciatic nerve cannot move.
I am up to walking an hour and the extreme edge of pain is gone!!!
Of course I am not a Doctor so I cannot give advise but only opinions as to my
unique situation, and every situation is different.
Dr. Chambi is the doctor that all the Pro Athletes choose and there must be a reason
for that.
Take care,
I hope that you recover soon!
Paul Dean, Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
==================================================================================
Side Note: July 23, 2005 - Paul Dean
I am continuing to recover at my own body's rate which seems to be a little bit
slow but you really can't recover at any pace faster than your own natural
pace of healing. Nerves take up to three years to have their full healing ability.
So do not be to impatient if the second you get off the operating table that you
are not completely healed. That just isn't how nerves work if they have been damaged
for a long time. The problem is that once your sciatic nerve in your hip has
been entrapped at the piriformis level for several years, the elasticy shrinks
and you will hurt every time you stretch until you get your nerve elasticy back.
This is the reason that you need to walk an hour or more every day to get that
elasticty back. It will hurt to walk long distances and that is why I use the
Lidocaine patch. This patch numbs the area that hurts in the back of the hip,
so you can walk further and stretch the sciatica nerve.
Rubber band Analogy:
I can imagine a rubber band that needs another inch or two in order to reach
its full potential of stretch. So every day I walk, and then I walk some more,
stretching that rubber band, which is the sciatic nerve. Once the nerve is used
to the stretch it doesn't hurt as much. Of course this is done after the
surgery because the sciatic nerve could not stretch at all when it was tethered
down from tissues wrapped around it from a fall accident I had from work. Now
that there is no entrapment of the nerve I am gently stretching that nerve
until it gets used to the stretch and stops hurting when I walk. The goal
is to have absolutely no pain no matter what I am doing and that is my eventual
goal.
Vitamins B1 and B12 and Antioxidants to build up the Immunity and Healing:
What about boosting the immunity system to have a faster healing process?
I am on a Vitamin Regiment of B1 Vitamin and B12 Vitamin in decent doses as
well as an Anti-oxidant supplement to get my system in good working order so
that I can heal as fast as possible.
I have tried to increase the rate of healing by getting toxins out of my
system by doing the following:
Do's:
Vitamin B (B1) (B12) Vitamin A,B,C,E Beta Carotene and Mineral Supplements.
Drink Six glasses of water a day
Drink as much Grapefruit juice (no Sugar) as possible
Eat as many raw fruits and vegetables as possible
Chicken and Fish
Dont's:
No Salt and No Sugar need to be eaten it is in your foods already.
No Greasy Processed Foods
No Fast-food
No Breads or rice or potatoes
Please see a Doctor before using these above techniques which I am
following as your medications may require that you do not follow
my above plan for getting your system back into shape for quicker healing.
Note: These above Do's and Don'ts can be found in the book of President Clintons
Doctor: Michael F. Roizen, MD. and Mehmet C. Oz, MD copyright 2005,
"YOU, THE OWNER'S MANUAL", The insider's guide to the body that will make
you healthier and younger. Harpercollins Publishers Inc, 10 East 53rd Street
New York, NY 10022.
I have no affiliation with any of these works and please take all information
as third party opinion and review options with your Doctors before doing
anything with your body. Thank you.
Above Updated: April 8, 2005
------------------------------------------------------------------------------
--------------------------------------------------------------------------------
New Entry: July 25, 2007 - Updated Medical Condition of Post Piriformis Syndrome
with Piriformis Release Surgery and Post Discectomy of L5 S1 Disc.
--------------------------------------------------------------------------------
Email Response to Susan:
--------------------------------------------------------------------------------
July 25, 2007
Hi Susan, (Disclaimer: I am a patient like yourself and am not a Doctor.)
Thank you for reading all of my postings, I'm sure it must have taken awhile to get
through it all. Pain is an interesting thing, in makes you want to read every single
thing you can find out about your pain hoping that you can some how stumble upon the
right information that can give you some pain relief. That is what I did and I am sure
that is also what you are seeking and I am wishing you the best of luck in advance, as
pain can control and ruin a good life that was before pain free.
Susan wrote:
The last update on your progress was quite some time ago. How is the sitting going
now?
Paul's reply:
Yes, the update was quite a while ago mostly because I have been busy back in the
Tradeshow business, which requires lifting heavy amounts of weight for a duration of
time. So, in part I have to say that I have gotten better, because it was unfathomable
before my piriformis surgery that I would be able to excel in either of my heavy lifting
jobs. Lifting in duration and for long periods of time was difficult to impossible
before my surgery. Now to answer the sitting question which is important because my
travel time to and from work is an hour and a half each way most of the time. I still
have pain, but not extreme pain and I can get out of it by putting my car on cruise
control and taking my right leg out of the stretch that is required to press down the
gas peddle. I use cruise control most of the time because my pain is elevated. So now
the next question is how much has my pain level improved since the surgery.
I would say it has gone from a 7 to 8 in pain level down to a 2 and 3 which has given
my life back to me in many ways as I enjoy physical activity with lifting and movies
which last up to 3 hours. I do have problems with movies over 2 hours and will take a
15 minute walk around the lobby during a movie in order to stop my pain. It seems that
almost instantly when the leg is no longer in a bad position of a stretch or just
sitting to long in the theater, the walking relieves the pain instantly. Where is the
pain in the first place, it seems that it is in the thigh area, but before the surgery
I had both buttock an thigh pain. Would I do the surgery over again? Definitely, yes as
my pain levels went down to a livable tolerance level. I am still cautious as to getting
back into tennis as that does a lot of thigh stretching but I will try to see if I can
slowly work back into this great sport that I have loved.
Susan wrote:
I'm at the "I need surgery" stage and am trying to find the best, most experienced
surgeon. I live in Florida and am having a difficult time finding someone in this
area who might be competent to do this specialized procedure. It seems that your
doctor and Dr. Filler are both in California and the thought of sitting on an airplane
for 5 hours, then spending several weeks in a hotel room after surgery is not the best
option. Sciatica and Piriformis Syndrome: Dr. Aaron Filler Santa Monica, CA:Preview Link Other
Dr. Aaron Filler Techniques: Link Link
Paul's reply:
It is hard to find an experienced Surgeon and I would recommend you pick somebody who
is doing this type of surgery day in and day out who has done more than anybody else
especially since you only get one shot at this surgery so you need to go to the best.
I went to Dr. Chambi in Santa Ana, CA, I have heard the name Dr. Filler and I have
also seen a Dr. Palmer In Mission Viejo, CA.
Would I fly 5 hours in order to be close to pain free with the proper surgery, after
having a correct diagnosis? Yes, I would do just about anything to get my previous
life back and feel good again, pain free or close to it. Luckily, my surgeon is only
40 minutes to an hour away.
As far as flying back after a surgery, you should be able to do this after three weeks
post surgery, with help. I was able to walk the day after the surgery but had problems
with Sitting and putting on my clothes and getting around because you are limited when
Recovering from this type of procedure.
Susan Wrote:
I went to NYC and saw Loren Fishman, went through Botox with him, and feel like a
human pin cushion with all of the various injections from various doctors. I even
wanted to try prolotherapy but at least that doctor was honest enough to tell me he
thought it wouldn't help. You're the only person that I've found who has actually had
this surgery so I'm very curious about your long term results. Some of the orthopedic
doc's that I've seen will do surgery but want to cut the entire buttocks to do it
(they all specialize in hip replacements around here). I obviously don't want an
invasive procedure when there are alternatives available. Also, as a curiosity, did
you have involvement of bursitis in the hip and thigh with this? I'm trying to figure
out if it's a side effect or a totally different problem.
Paul's reply:
My condition was that of a post herniated disc surgery called a Discectomy of the L5 S1
region of a previous herniated disk of 7 millimeters. The 7 millimeter herniation was
cut out so the nerve was then again free, which it showed that it was free in the post
MRI, however I still had some severe sciatica pain going from the buttock down the right
back side of thigh which is the area where the sciatic nerve travels.
I then had some steroid injections into the L5 S1 back to relieve any possible
inflammation that might be causing my pain and these injections did not help me with my
pain.
I then saw Dr. Chambi and had three Lidocaine injections to the buttocks where the
pain was at a precise location. The 5 inch needle was inserted and the first one
of the three different injections done on different weeks solved my pain temporarily
and so I thought this was quite a miracle to all of a sudden have no pain after a
buttock shot to the piriformis muscle. When the piriformis muscle was relaxed, I was
pain free. However the pain came back after the shot wore off. I also wore a lidocaine
patch which gave some relief to the area installed such as buttock and back of
leg, but was temporary.
It is at that point that Dr. Chambi said, you have piriformis syndrome because the
piriformis muscle has entrapped your sciatic nerve and there is only one permanent
solution which is a piriformis release. Piriformis Release is a way of cutting away the
piriformis from the sciatic nerve. Apparently, the sciatic nerve had somehow gotten
scarred down from a fall I had, and it was entrapped. After the piriformis was cut away
from the nerve, I had great relief, because the sciatic nerve could then move freely
again. It was no longer pinched down, and was not constricted any longer by the
piriformis muscle.
Susan wrote:
Some of the orthopedic doc's that I've seen will do surgery but want to cut the entire
buttocks
Paul's reply:
The actual cut that the surgeon does for piriformis release is similar to the cut
done in a hip replacement at about a 4 to 5 inch cut across the buttock. The
piriformis nerve is about 6 inches down and a lot of the Buttock area needs to
be moved away to be able to get to the piriformis muscle and underneath were the
sciatic nerve is located.
Susan wrote:
I obviously don't want an invasive procedure when there are alternatives available.
Paul's reply:
You first try all the physical therapy and water therapy and all the different shots
available but when they all fail, then you look to the surgery for a permanent cure,
and only after at least two experts agree with the same diagnosis, in this case,
piriformis syndrome, then you take the next step, if both doctors agree that this is
the next step to take after exhausting all other steps, and needing a permanent
solution. You should not be afraid of surgery when you are with an expert in the field.
Do not be afraid of the recovery pain as you are given strong pain killers to take this
pain away until you have finally recovered.
Finally, make sure that you have gotten relief with the Lidocaine injection which
relaxes the piriformis muscle and gives relief to the sciatic nerve, which pretty much
is the telling sign that the piriformis muscle is involved in your pain. Many
Orthopedic Doctors will say this is not the case because the do not understand that the
piriformis muscle and scarring can stop the sciatic nerve from functioning properly.
I suggest you see Doctors that study Nerves and not just bone doctors as your problem
May not be a bone or disc disease.
The most important thing to find is the right Doctor and the correct Diagnosis, and it
won't be easy to find this.
Susan Wrote;
Did you have involvement of bursitis in the hip and thigh with this? I'm trying to
figure out if it's a side effect or a totally different problem.
Paul's reply:
No I was not diagnosed with bursitis in the hip or thigh. That may very well be
something else. This is why it is important to get the proper diagnosis and to see
more than one specialist no narrow down where and what your pain is and what is causing
it. You can go to three different specialists and get three different expert opinions,
and this is a big problem in figuring out what to do next, so you'll have to find the
best of the best in specialists in order to get a correct diagnostics of your problem.
Even a phone consultation is better than nothing, so I suggest that you keep searching
for a correct diagnosis and then go forward with the proper treatment once this is
found.
Hope is one thing we all have even when things look bad. You keep on thinking
that you will wake up and be pain free. Maybe this sounds unrealistic but we
keep on holding on to this hope. Can nerves regrow themselves and straighten
themselves out so that signals are then properly sent to and from the body
to the brain? We hope that some how this will happen, however sometimes nerves
don't grow back so we are stuck with tollerating pain. Then, it is up to us to
figure out what we are going to do with this pain and how to tempoarily get out
of pain. To each person they have their own answers. My answer is to keep going.
My Disclaimer: I am not a Doctor and am not in a related medical field and am only a
patient looking for a solution to pain. Do not take anything I say as a fact, but
instead contact your local specialist and get the correct diagnosis from a professional.
I sincerely hope you are pain free soon, from one patient to another, Good luck with a
pain free life.
Thank you,
Paul
knowledge is Power
Thank you,
Paul Dean, Spy Hunter Video Game (Guinness Book) Champion - June 28, 1985 and
2007 Guinness Book
www.spyhunter007.com
Last Updated: April 8, 2005
Click At Desired Graphic Text For Each Introduction
Biography Commentary Questions
Click On Below Graphic Text For Spy Hunter Introduction
Tournament and Guinness Book Results From 1983-2004
Click On Below Graphic Text For All Video High Scores thru 2004
The Golden Era
Click On Below Graphic Text For Material On The Golden Years Of Video Games 1980's
Click the Below Graphic Text to read my Conversations With Walter Day
June 9, 2004 Walter Day states, "No Replay Necessary" for Paul Dean
Find A Video Game Auction Near You

Home Page

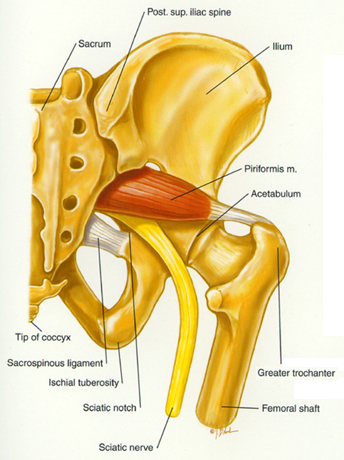
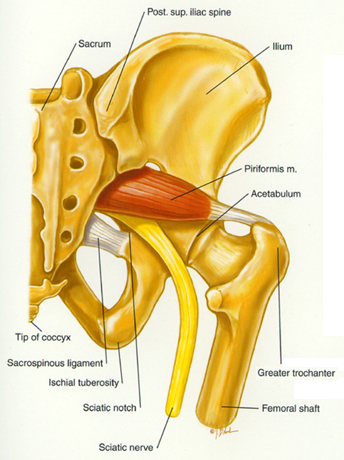
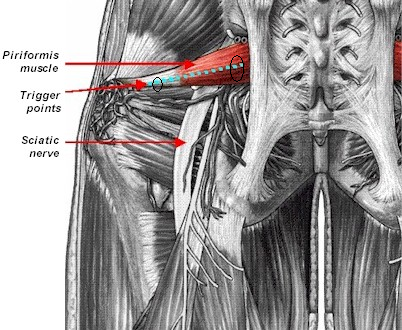 When the initial examination takes place, it is very common to see the patient
leaning toward the other side (when sitting or standing) in order to reduce the
compression of the sciatic nerve. The great majority of these patients are taking
medications - for example, 800 milligrams of ibuprofen (Motrin) three times a
day, or 500 milligrams of naproxen two times a day - with little or no improvement.
The examination of the affected area begins with moderate digital palpation of
GB 30 and moves toward the midline. A series of trigger points will be discovered
that, when palpated, will produce local and/or referred pain (referred pain/
tingling toward the buttock and/or leg [UB channel]).
Technique used: Chinese acupuncture needles (gauge #36), 1.5-2 inches long.
Micro-current device: Acutron Mentor, biphasic milliamp pads, with milliamp
stimulation for 20 minutes (milliamp stimulation is maintained as a noticeable,
mild tingling sensation). A second stage follows: a cooling period of five minutes
(micro amp stimulation, biphasic, 75-100 micro-amps).
Treatment points: GB 30 is connected to 2-4 trigger areas on top of the piriformis
muscle.
The treatment frequency is 1-3 times a week (depending on the pain level) for 4-6
weeks. The acupuncture needles are inserted with the stimulation pads on top of
the needles (the pads used are Zimmer, single use).
Within 6-8 treatments, the patient is able to feel improvement: pain/burning and
tingling is reduced; the range of motion of the hip is increased; and pain medication
reduced or discontinued.
As in almost all muscle disorders, the indication of the appropriate stretching
exercises for the muscles involved will assist in a speedy recovery. A course
of daily stretching exercises is recommended (part of the protocol) to patients
to assist in recovery of the muscles and tendons. Targeting the piriformis is
done with a single knee to the chest with painful side cross-over. The stretching
exercises are performed three times a day, five times each time, maintaining the
stretch between 5-10 seconds. It is convenient to apply heat for 15 to 20 minutes
before the stretching exercises are done in order to increase the elasticity of
the muscle, and ice for five minutes afterward in order to reduce the inflammation
produced by the stretching exercises.
Other treatments: Posture training is another pillar of patient rehabilitation.
In some cases, a cortisone injection is administered locally to reduce the inflammation
and edema of the muscle. Surgery is another resource (although rarely used): it
"cleans up" the fibrotic muscle.
If you have any questions about the treatment described in this article, please
contact me at the address below.
Alejandro J. Katz, MD, OMD, LAc, QME
Los Angeles, California
tvstardr@aol.com
www.drkatz.org
============================================================================
When the initial examination takes place, it is very common to see the patient
leaning toward the other side (when sitting or standing) in order to reduce the
compression of the sciatic nerve. The great majority of these patients are taking
medications - for example, 800 milligrams of ibuprofen (Motrin) three times a
day, or 500 milligrams of naproxen two times a day - with little or no improvement.
The examination of the affected area begins with moderate digital palpation of
GB 30 and moves toward the midline. A series of trigger points will be discovered
that, when palpated, will produce local and/or referred pain (referred pain/
tingling toward the buttock and/or leg [UB channel]).
Technique used: Chinese acupuncture needles (gauge #36), 1.5-2 inches long.
Micro-current device: Acutron Mentor, biphasic milliamp pads, with milliamp
stimulation for 20 minutes (milliamp stimulation is maintained as a noticeable,
mild tingling sensation). A second stage follows: a cooling period of five minutes
(micro amp stimulation, biphasic, 75-100 micro-amps).
Treatment points: GB 30 is connected to 2-4 trigger areas on top of the piriformis
muscle.
The treatment frequency is 1-3 times a week (depending on the pain level) for 4-6
weeks. The acupuncture needles are inserted with the stimulation pads on top of
the needles (the pads used are Zimmer, single use).
Within 6-8 treatments, the patient is able to feel improvement: pain/burning and
tingling is reduced; the range of motion of the hip is increased; and pain medication
reduced or discontinued.
As in almost all muscle disorders, the indication of the appropriate stretching
exercises for the muscles involved will assist in a speedy recovery. A course
of daily stretching exercises is recommended (part of the protocol) to patients
to assist in recovery of the muscles and tendons. Targeting the piriformis is
done with a single knee to the chest with painful side cross-over. The stretching
exercises are performed three times a day, five times each time, maintaining the
stretch between 5-10 seconds. It is convenient to apply heat for 15 to 20 minutes
before the stretching exercises are done in order to increase the elasticity of
the muscle, and ice for five minutes afterward in order to reduce the inflammation
produced by the stretching exercises.
Other treatments: Posture training is another pillar of patient rehabilitation.
In some cases, a cortisone injection is administered locally to reduce the inflammation
and edema of the muscle. Surgery is another resource (although rarely used): it
"cleans up" the fibrotic muscle.
If you have any questions about the treatment described in this article, please
contact me at the address below.
Alejandro J. Katz, MD, OMD, LAc, QME
Los Angeles, California
tvstardr@aol.com
www.drkatz.org
============================================================================
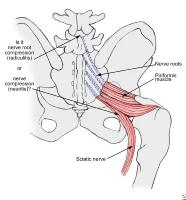 Barton PM.
Department of Physical Medicine and Rehabilitation, University of Western Ontario,
London, Canada.
Although rarely recognized, the piriformis syndrome appears to be a common cause of
buttock and leg pain as a result of injury to the piriformis muscle. Four cases
representing a broad spectrum of presentations are described here. The major findings
include buttock tenderness extending from the sacrum to the greater trochanter and
piriformis tenderness on rectal or pelvic examination. Symptoms are aggravated by
prolonged hip flexion, adduction, and internal rotation, in the absence of low back
or hip findings. Minor findings may include leg length discrepancy, weak hip abductors,
and pain on resisted hip abduction in the sitting position. Myofascial involvement of
related muscles and lumbar facet syndromes may occur concurrently. The diagnosis is
primarily clinical as no investigations have proved definitive. The role of MRI of the
piriformis muscle is assessed and other investigative tools are discussed. A rational
management schema is demonstrated: (1) underlying biomechanical factors and associated
conditions should be corrected; (2) the patient is instructed in a home program of
prolonged piriformis muscle stretching which may be augmented in physical therapy by
preceding ultrasound or Fluori-Methane (dichlorodifluoromethane and trichloromono
fluoromethane spray); (3) a trial of up to three steroid injections is attempted;
and (4) if all these measures fail, consideration should be given to surgical sciatic
nerve exploration and piriformis release.
Piriformis Muscle Injection:
Barton PM.
Department of Physical Medicine and Rehabilitation, University of Western Ontario,
London, Canada.
Although rarely recognized, the piriformis syndrome appears to be a common cause of
buttock and leg pain as a result of injury to the piriformis muscle. Four cases
representing a broad spectrum of presentations are described here. The major findings
include buttock tenderness extending from the sacrum to the greater trochanter and
piriformis tenderness on rectal or pelvic examination. Symptoms are aggravated by
prolonged hip flexion, adduction, and internal rotation, in the absence of low back
or hip findings. Minor findings may include leg length discrepancy, weak hip abductors,
and pain on resisted hip abduction in the sitting position. Myofascial involvement of
related muscles and lumbar facet syndromes may occur concurrently. The diagnosis is
primarily clinical as no investigations have proved definitive. The role of MRI of the
piriformis muscle is assessed and other investigative tools are discussed. A rational
management schema is demonstrated: (1) underlying biomechanical factors and associated
conditions should be corrected; (2) the patient is instructed in a home program of
prolonged piriformis muscle stretching which may be augmented in physical therapy by
preceding ultrasound or Fluori-Methane (dichlorodifluoromethane and trichloromono
fluoromethane spray); (3) a trial of up to three steroid injections is attempted;
and (4) if all these measures fail, consideration should be given to surgical sciatic
nerve exploration and piriformis release.
Piriformis Muscle Injection: 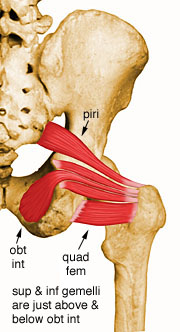 "...The existence of piriformis syndrome has been doubted for years."
Piriformis syndrome may overlap with a variety of other problems including what
McCrory et. al. have called a "deep buttock" syndrome. This includes pain in the
buttock region, possibly pain in the hamstrings, occasionally pain in the back
of the leg that is difficult to locate.
"...The existence of piriformis syndrome has been doubted for years."
Piriformis syndrome may overlap with a variety of other problems including what
McCrory et. al. have called a "deep buttock" syndrome. This includes pain in the
buttock region, possibly pain in the hamstrings, occasionally pain in the back
of the leg that is difficult to locate.  Piriformis Stretch
The gentle Piriformis Stretch:
Place the right knee on the ground roughly in line with your
left shoulder The right foot should be just in front of the
left knee Press your hips towards the ground so that your
bodyweight is on your right leg. As you move down the right
knee comes closer to the left shoulder.
You should feel a gentle pull deep in the right hip / buttocks.
-----------------------------------------------------------------------------------
A good sports medicine physician with experience in caring for athletes with the
piriformis syndrome can help direct appropriate management. With proper diagnosis
and treatment, there is no reason for this syndrome to be dreaded. Good luck and
good training.
last update - 2/97
Diagnosis:
The symptoms most often reported are pain when running or walking in the gluteal
region. Pain may go down the back of the leg. Dyspareunia is sometimes noted.
Having the patient lie down, flex the knee to 10 - 20 degrees and then have the
patient attempt to externally rotate the leg against resistance. Pain may occur
with piriformis tendonitis. Direct tenderness will be found in the region of the
piriformis tendon over the buttock region.
If there is a positive test to the straight leg lift (causing sciatica like pain),
externally rotate the leg to see if this lessens the pain. This could indicate
compression of the sciatic nerve by the piriformis.
Be certain to examine the sacroiliac joint also.
Treatment:
Rest is usually recommended. A two to three week break from the sports and activities
that cause pain can be very helpful. Relative rest, meaning less intense workouts,
and fewer miles is also helpful, and should be used during your return to activity.
Like Achilles tendonitis and iliopsoas tendonitis this is a very difficult problem
to eliminate.
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the course
of the sciatic nerve. This referred pain, called "sciatica", often goes down the
back of the thigh and/or into the lower back. Patients generally complain of pain
deep in the buttocks, which is made worse by sitting, climbing stairs, or performing
squats.
The anatomical position of the muscle leads one to conclude that it functions in
some ways similar to that of the gluteus medius. The major portion of origin of the
piriformis is the anterior lateral portion of the sacrum and the insertion is on the
upper portion of the femur.
It can be seen that the sciatic nerve passes immediately below the piriformis muscle.
The first places the sciatic nerve inferior (below) to the Piriformis muscle and
superior (above) the gemellus muscle. Entrapment in this area is likely due to a
myospasm or contracture (tightening or shortening respectively) of either of these
two muscles. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
This particular syndrome can often mimic its more notorious counterpart known as
sciatica, and that being the case, it is often misdiagnosed as sciatica. The main
difference between sciatica and piriformis syndrome is in the cause. Sciatica is
directly due to a lumbar disc pressing on the sciatic nerve as it exits the intervertebral
foramen in the lumbar spine. What both of these complaints have in common is that
both can produce pain, numbness and tingling below the knee and into the foot.
Piriformis Stretch
The gentle Piriformis Stretch:
Place the right knee on the ground roughly in line with your
left shoulder The right foot should be just in front of the
left knee Press your hips towards the ground so that your
bodyweight is on your right leg. As you move down the right
knee comes closer to the left shoulder.
You should feel a gentle pull deep in the right hip / buttocks.
-----------------------------------------------------------------------------------
A good sports medicine physician with experience in caring for athletes with the
piriformis syndrome can help direct appropriate management. With proper diagnosis
and treatment, there is no reason for this syndrome to be dreaded. Good luck and
good training.
last update - 2/97
Diagnosis:
The symptoms most often reported are pain when running or walking in the gluteal
region. Pain may go down the back of the leg. Dyspareunia is sometimes noted.
Having the patient lie down, flex the knee to 10 - 20 degrees and then have the
patient attempt to externally rotate the leg against resistance. Pain may occur
with piriformis tendonitis. Direct tenderness will be found in the region of the
piriformis tendon over the buttock region.
If there is a positive test to the straight leg lift (causing sciatica like pain),
externally rotate the leg to see if this lessens the pain. This could indicate
compression of the sciatic nerve by the piriformis.
Be certain to examine the sacroiliac joint also.
Treatment:
Rest is usually recommended. A two to three week break from the sports and activities
that cause pain can be very helpful. Relative rest, meaning less intense workouts,
and fewer miles is also helpful, and should be used during your return to activity.
Like Achilles tendonitis and iliopsoas tendonitis this is a very difficult problem
to eliminate.
The piriformis syndrome is a condition in which the piriformis muscle irritates
the sciatic nerve, causing pain in the buttocks and referring pain along the course
of the sciatic nerve. This referred pain, called "sciatica", often goes down the
back of the thigh and/or into the lower back. Patients generally complain of pain
deep in the buttocks, which is made worse by sitting, climbing stairs, or performing
squats.
The anatomical position of the muscle leads one to conclude that it functions in
some ways similar to that of the gluteus medius. The major portion of origin of the
piriformis is the anterior lateral portion of the sacrum and the insertion is on the
upper portion of the femur.
It can be seen that the sciatic nerve passes immediately below the piriformis muscle.
The first places the sciatic nerve inferior (below) to the Piriformis muscle and
superior (above) the gemellus muscle. Entrapment in this area is likely due to a
myospasm or contracture (tightening or shortening respectively) of either of these
two muscles. The athlete's cause is primarily due to improper stretching and warm-up
exercises as well as overuse during activity. In this case it is most likely that
the piriformis muscle is irritated and usually in spasm.
This particular syndrome can often mimic its more notorious counterpart known as
sciatica, and that being the case, it is often misdiagnosed as sciatica. The main
difference between sciatica and piriformis syndrome is in the cause. Sciatica is
directly due to a lumbar disc pressing on the sciatic nerve as it exits the intervertebral
foramen in the lumbar spine. What both of these complaints have in common is that
both can produce pain, numbness and tingling below the knee and into the foot.
 Stock Photo
Israel P. Chambi-Venero, MD
Neurosurgeons
Israel P. Chambi, M.D., FACS
801 N. Tustin Ave., Suite 406
Santa Ana, CA 92705
714 973 0810
FAX 714 973 0840
drisraelchambi@yahoo.com
Diplomat American Board of Neurological Surgery Brachial-Plexus & Peripheral
Nerve Institute
micro neural surgeon
- Santa Ana, California (CA) 92705
PRESCRIPTION
Stock Photo
Israel P. Chambi-Venero, MD
Neurosurgeons
Israel P. Chambi, M.D., FACS
801 N. Tustin Ave., Suite 406
Santa Ana, CA 92705
714 973 0810
FAX 714 973 0840
drisraelchambi@yahoo.com
Diplomat American Board of Neurological Surgery Brachial-Plexus & Peripheral
Nerve Institute
micro neural surgeon
- Santa Ana, California (CA) 92705
PRESCRIPTION Family practice Physician
Chapel Medical Clinic
9739 California Avenue
South Gate, CA 90280
Phone: 323-567-1212
-------------------------------------------------------------------------------
Ebenezer Chambi: Dialogue with an Adventist physician, health educator, and
community leader
Family practice Physician
Chapel Medical Clinic
9739 California Avenue
South Gate, CA 90280
Phone: 323-567-1212
-------------------------------------------------------------------------------
Ebenezer Chambi: Dialogue with an Adventist physician, health educator, and
community leader 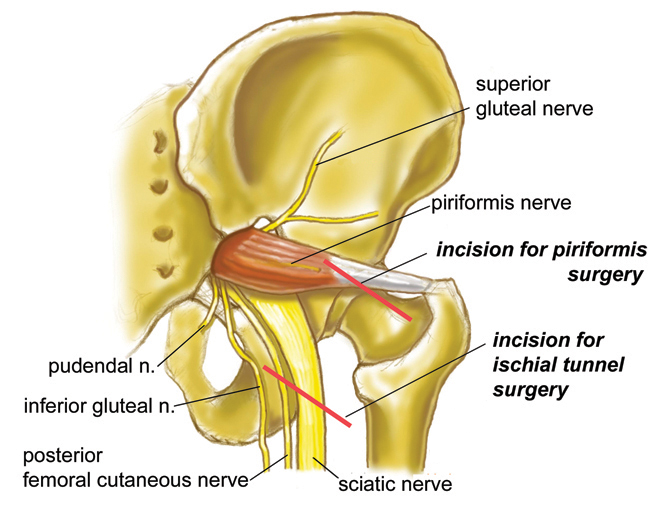 Piriformis Surgery Incision
Piriformis surgery is now a small procedure which can be carried out under local
anaesthetic as an outpatient. Traditional piriformis surgery is a large and debilitating
operation but no patient should be having these operations today. There were two types
of traditional piriformis surgery, one involves a large lateral hip incision similar
to the approach used for a hip replacement surgery. The second involves a very large
incision and involves completely detaching all of the gluteal muscles from the iliac
crest. Both of these types of surgery result in weeks of debilitation, walking on
crutches and pain, with only limited success treating the original problem.
The new type of "minimal access surgery" developed at the Institute for Nerve Medicine
by Dr. Aaron Filler involves only a small incision, and in most cases can be performed
on an outpatient basis. Large scale formal outcome trials involving hundreds of patients
with follow-up out to eight years show no detectable effect on normal walking in any
of the patients - this a great change from the traditional surgery that often leaves
permanent problems with gait. Recovery takes only a few days in most patients.
Those patients who have positive physical exam findings, positive MR neurography
findings and a clear positive response to MRI guided piriformis injection have had
a 85% to 90% good to excellent outcome.
---
Piriformis Syndrome & Sciatica
Piriformis Surgery Incision
Piriformis surgery is now a small procedure which can be carried out under local
anaesthetic as an outpatient. Traditional piriformis surgery is a large and debilitating
operation but no patient should be having these operations today. There were two types
of traditional piriformis surgery, one involves a large lateral hip incision similar
to the approach used for a hip replacement surgery. The second involves a very large
incision and involves completely detaching all of the gluteal muscles from the iliac
crest. Both of these types of surgery result in weeks of debilitation, walking on
crutches and pain, with only limited success treating the original problem.
The new type of "minimal access surgery" developed at the Institute for Nerve Medicine
by Dr. Aaron Filler involves only a small incision, and in most cases can be performed
on an outpatient basis. Large scale formal outcome trials involving hundreds of patients
with follow-up out to eight years show no detectable effect on normal walking in any
of the patients - this a great change from the traditional surgery that often leaves
permanent problems with gait. Recovery takes only a few days in most patients.
Those patients who have positive physical exam findings, positive MR neurography
findings and a clear positive response to MRI guided piriformis injection have had
a 85% to 90% good to excellent outcome.
---
Piriformis Syndrome & Sciatica 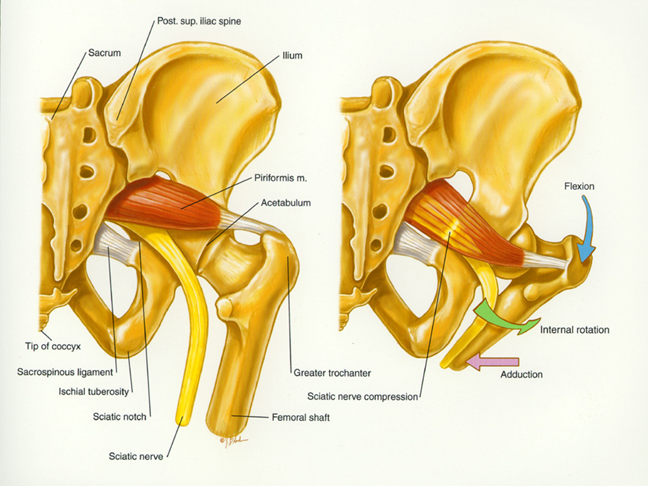 This drawing illustrates the important anatomy for piriformis syndrome and shows
how certain leg positions pull the piriformis muscle up against the sciatic nerve
causing buttock pain and radiating leg pain.
Piriformis Syndrome
Anatomy of the piriformis muscle and sciatic nerve
in a T1 weighted axial MRI scan
Piriformis Muscle Open MRI Anatomy Photo
This drawing illustrates the important anatomy for piriformis syndrome and shows
how certain leg positions pull the piriformis muscle up against the sciatic nerve
causing buttock pain and radiating leg pain.
Piriformis Syndrome
Anatomy of the piriformis muscle and sciatic nerve
in a T1 weighted axial MRI scan
Piriformis Muscle Open MRI Anatomy Photo 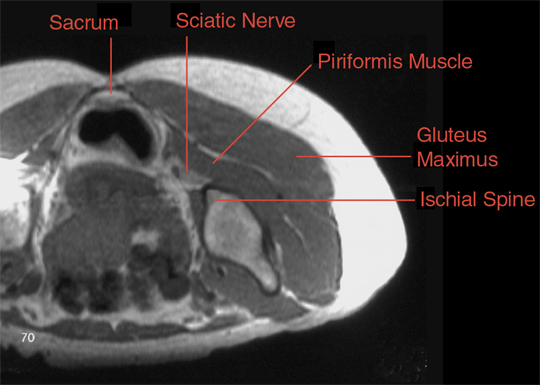 This T1 weighted axial MRI scan shows the anatomy used to guide the injection of the piriformis
muscle in an Open MRI scanner.
This T1 weighted axial MRI scan shows the anatomy used to guide the injection of the piriformis
muscle in an Open MRI scanner.
 Critical physical exam maneuver for muscle based piriformis syndrome: The patient's
foot is placed lateral to the contra lateral knee. Resisted abduction or adduction
against the examiner's hand may reproduce the symptoms. Straight leg rising is
typically negative. There is often relief obtained by traction on the involved leg,
particularly by pulling upwards at a ten to twenty degree angle and towards the
contra lateral side by a similar amount. The distribution of symptoms typically involves
both L5 (big toe) and S1 (small toe) components because this a pan-sciatic syndrome.
The symptoms often progress no further than the ankle in distinction to sciatica
from a lumbar disk which typically radiates into the toes.
Critical physical exam maneuver for muscle based piriformis syndrome: The patient's
foot is placed lateral to the contra lateral knee. Resisted abduction or adduction
against the examiner's hand may reproduce the symptoms. Straight leg rising is
typically negative. There is often relief obtained by traction on the involved leg,
particularly by pulling upwards at a ten to twenty degree angle and towards the
contra lateral side by a similar amount. The distribution of symptoms typically involves
both L5 (big toe) and S1 (small toe) components because this a pan-sciatic syndrome.
The symptoms often progress no further than the ankle in distinction to sciatica
from a lumbar disk which typically radiates into the toes. 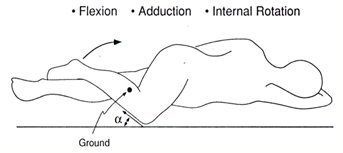 -----
PIRIFORMIS SYNDROME
-----
PIRIFORMIS SYNDROME 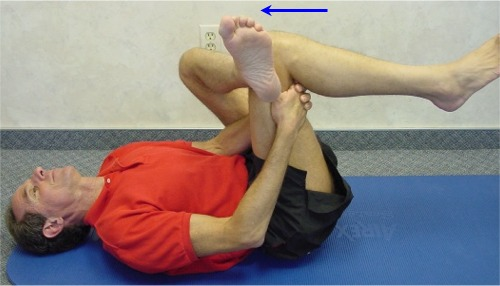 Piriformis Gluteus Stretch
Laying down on your back, bend your right knee, and place your left leg over the
right leg, resting the outside of the left ankle slightly above the right knee.
Place your right hand around the outside of your right thigh and place the left
hand around the inside of your right thigh. Lock the two hands together. Now pull
forward towards your chest to achieve a stretch in the left gluteus portion of you
buttocks. Do the exact opposite to achieve a stretch of the right gluteus portion
of the buttocks. Hold each stretch for a minimum of 30 seconds, any less than 15
seconds and the muscle will not conform to the new increase in length. Do 3 reps,
3-6 times a day. Any pain you feel with this exercise should only be a local
stretching sensation to the back of your thigh and buttocks area, without aggravating
your condition.
Piriformis Stretch
Piriformis Gluteus Stretch
Laying down on your back, bend your right knee, and place your left leg over the
right leg, resting the outside of the left ankle slightly above the right knee.
Place your right hand around the outside of your right thigh and place the left
hand around the inside of your right thigh. Lock the two hands together. Now pull
forward towards your chest to achieve a stretch in the left gluteus portion of you
buttocks. Do the exact opposite to achieve a stretch of the right gluteus portion
of the buttocks. Hold each stretch for a minimum of 30 seconds, any less than 15
seconds and the muscle will not conform to the new increase in length. Do 3 reps,
3-6 times a day. Any pain you feel with this exercise should only be a local
stretching sensation to the back of your thigh and buttocks area, without aggravating
your condition.
Piriformis Stretch
 Piriformis Stretch
Laying down on your back, bend your right leg and pull up your right knee towards
your opposite chest with your left hand. You should feel the stretch in the Piriformis
portion of the right buttocks. Do the exact opposite to achieve a stretch of the left
Piriformis portion of the buttocks. Hold each stretch for a minimum of 30 seconds,
any less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the back of your thigh and buttocks area, without
aggravating your condition.
TFL Stretch
Piriformis Stretch
Laying down on your back, bend your right leg and pull up your right knee towards
your opposite chest with your left hand. You should feel the stretch in the Piriformis
portion of the right buttocks. Do the exact opposite to achieve a stretch of the left
Piriformis portion of the buttocks. Hold each stretch for a minimum of 30 seconds,
any less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the back of your thigh and buttocks area, without
aggravating your condition.
TFL Stretch
 TFL Stretch
Start with stretching the TFL portion of the left hip and outside thigh. While
standing, hold your left hand securely on a solid surface to support your body
as you place your left leg past your right until you reach a maximum stretch.
Follow this with tilting your upper back to the right side while simultaneously
pushing the left side of the hip. Do the exact opposite to achieve a stretch of
the right TFL portion of the hip and outside thigh. Hold each stretch for a
minimum of 30 seconds, any less than 15 seconds and the muscle will not conform
to the new increase in length. Do 3 reps, 3-6 times a day. Any pain you feel
with this exercise should only be a local stretching sensation to the TFL portion
of the hip and outside thigh, without aggravating your condition.
Calf Stretch
TFL Stretch
Start with stretching the TFL portion of the left hip and outside thigh. While
standing, hold your left hand securely on a solid surface to support your body
as you place your left leg past your right until you reach a maximum stretch.
Follow this with tilting your upper back to the right side while simultaneously
pushing the left side of the hip. Do the exact opposite to achieve a stretch of
the right TFL portion of the hip and outside thigh. Hold each stretch for a
minimum of 30 seconds, any less than 15 seconds and the muscle will not conform
to the new increase in length. Do 3 reps, 3-6 times a day. Any pain you feel
with this exercise should only be a local stretching sensation to the TFL portion
of the hip and outside thigh, without aggravating your condition.
Calf Stretch
 Calf Stretch
Start with stretching the right Gastrocnemius portion of the right calf area.
While standing, place your right leg in front of you and your left foot directly
behind you. Place the toes of your right forefoot up against a door or other flat
wall surface, keeping your heel down to the floor. Lean your upper body forward
to place a stretch on the back of the calf. Do the exact opposite to achieve a
stretch of the left calf area. Hold each stretch for a minimum of 30 seconds. Any
less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the calf area of the leg, without aggravating your
condition.
Psoas Stretch
Calf Stretch
Start with stretching the right Gastrocnemius portion of the right calf area.
While standing, place your right leg in front of you and your left foot directly
behind you. Place the toes of your right forefoot up against a door or other flat
wall surface, keeping your heel down to the floor. Lean your upper body forward
to place a stretch on the back of the calf. Do the exact opposite to achieve a
stretch of the left calf area. Hold each stretch for a minimum of 30 seconds. Any
less than 15 seconds and the muscle will not conform to the new increase in length.
Do 3 reps, 3-6 times a day. Any pain you feel with this exercise should only be a
local stretching sensation to the calf area of the leg, without aggravating your
condition.
Psoas Stretch
 Psoas Stretch
Start with stretching the right Psoas muscle. While standing, place your right leg
in front of you and your left foot directly behind you as far as you can comfortably
stretch it. Shift your lower body forward, while simultaneously pushing your upper
body backwards with your arms. Do the exact opposite to achieve a stretch of the
right Psoas portion of your front upper thigh area. Hold each stretch for a minimum
of 30 seconds. Any less than 15 seconds and the muscle will not conform to the new
increase in length. Do 3 reps, 3-6 times a day. Any pain you feel with this exercise
should only be a local stretching sensation to the Psoas area of the upper thigh,
without aggravating your condition.
Quadriceps Stretch
Psoas Stretch
Start with stretching the right Psoas muscle. While standing, place your right leg
in front of you and your left foot directly behind you as far as you can comfortably
stretch it. Shift your lower body forward, while simultaneously pushing your upper
body backwards with your arms. Do the exact opposite to achieve a stretch of the
right Psoas portion of your front upper thigh area. Hold each stretch for a minimum
of 30 seconds. Any less than 15 seconds and the muscle will not conform to the new
increase in length. Do 3 reps, 3-6 times a day. Any pain you feel with this exercise
should only be a local stretching sensation to the Psoas area of the upper thigh,
without aggravating your condition.
Quadriceps Stretch
 Quadriceps Stretch
Yoga and Meditation to Relax the Back
Regardless of the current situation your back is in, relaxing could be key to helping
it heal. While meditation can always be useful for achieving this, Yoga can at times
be irritating if caution is not taken. Yoga is a series of slow movements combined
with stretches and meditation to allow for an increase in flexibility and relaxation
to the muscles and joints, as well as to help optimally integrate the connection
between the mind and body. However, what might seem to be easy maneuvers should
still be treated cautiously, as your individual situation may prohibit certain Yoga
moves. One simple meditation practice that is usually met with good success is to
close your eyes and visualize yourself in the most happy and relaxing place you know
of. Sometimes just taking the time to do this can be what you need to begin the
healing process.
Medical Practitioners
Quadriceps Stretch
Yoga and Meditation to Relax the Back
Regardless of the current situation your back is in, relaxing could be key to helping
it heal. While meditation can always be useful for achieving this, Yoga can at times
be irritating if caution is not taken. Yoga is a series of slow movements combined
with stretches and meditation to allow for an increase in flexibility and relaxation
to the muscles and joints, as well as to help optimally integrate the connection
between the mind and body. However, what might seem to be easy maneuvers should
still be treated cautiously, as your individual situation may prohibit certain Yoga
moves. One simple meditation practice that is usually met with good success is to
close your eyes and visualize yourself in the most happy and relaxing place you know
of. Sometimes just taking the time to do this can be what you need to begin the
healing process.
Medical Practitioners 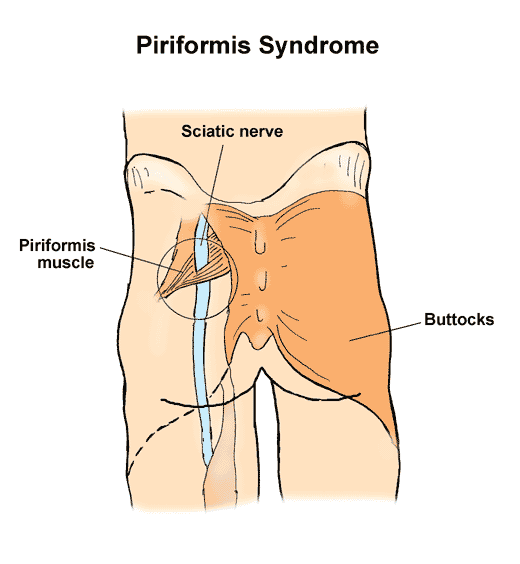 sciatic nerve passes through piriformis muscle
What is piriformis syndrome?
Piriformis syndrome refers to irritation of the sciatic nerve as it passes
through the piriformis muscle located deep in the buttock. Inflammation of
the sciatic nerve, called sciatica, causes pain in the back of the hip that
can often travel down into the leg.
How does it occur?
The piriformis muscle is located deep in the buttock and pelvis and allows
you to rotate your thigh outward. The sciatic nerve travels from your back
into your leg by passing through the piriformis muscle. If the piriformis
muscle is unusually tight or if it goes into spasm, the sciatic nerve can
become inflamed or irritated. Piriformis syndrome may also be related to
intense downhill running.
What are the symptoms?
sciatic nerve passes through piriformis muscle
What is piriformis syndrome?
Piriformis syndrome refers to irritation of the sciatic nerve as it passes
through the piriformis muscle located deep in the buttock. Inflammation of
the sciatic nerve, called sciatica, causes pain in the back of the hip that
can often travel down into the leg.
How does it occur?
The piriformis muscle is located deep in the buttock and pelvis and allows
you to rotate your thigh outward. The sciatic nerve travels from your back
into your leg by passing through the piriformis muscle. If the piriformis
muscle is unusually tight or if it goes into spasm, the sciatic nerve can
become inflamed or irritated. Piriformis syndrome may also be related to
intense downhill running.
What are the symptoms? 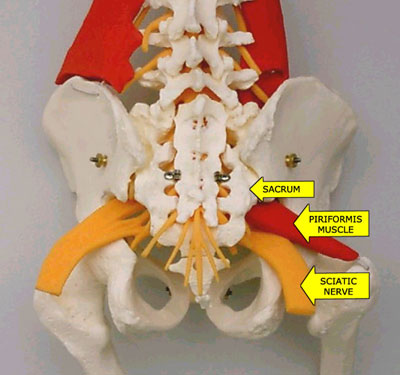 sciatic nerve runs below piriformis muscle
sciatic nerve runs below piriformis muscle
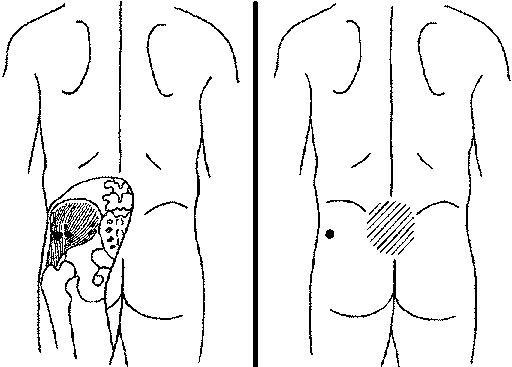 Piriformis Gluteus Medius Trigger Point - Massage with Tennis Ball or Lacrosse Ball
Question: Why use the Lacrosse Ball with the piriformis muscle while you are
against a wall instead of the tennis ball?
The reason is because you get a (deeper) rolling Massage into the painful trigger
points when using the Harder Lacrosse Ball, therefore, breaking up the tight painful
trigger areas that are similar to knotts that need to be softened and loosened
in order to get full elasticity of the muscle and surrounding area, making you
pain free in the long run.
Self-applied trigger point massage breaks into the chemical and neurological
feedback loop that maintains the muscle contractions so that you will have
increased circulation which has been resticted by knotts in the contracted tissue
and the massage will cause the contracted knotts to stretch out, releiving
pressure.
Piriformis Gluteus Medius Trigger Point - Massage with Tennis Ball or Lacrosse Ball
Question: Why use the Lacrosse Ball with the piriformis muscle while you are
against a wall instead of the tennis ball?
The reason is because you get a (deeper) rolling Massage into the painful trigger
points when using the Harder Lacrosse Ball, therefore, breaking up the tight painful
trigger areas that are similar to knotts that need to be softened and loosened
in order to get full elasticity of the muscle and surrounding area, making you
pain free in the long run.
Self-applied trigger point massage breaks into the chemical and neurological
feedback loop that maintains the muscle contractions so that you will have
increased circulation which has been resticted by knotts in the contracted tissue
and the massage will cause the contracted knotts to stretch out, releiving
pressure.
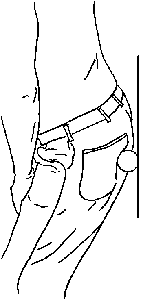 Piriformis Gluteus Medius Trigger Point Ball Massage
The illustration shows treatment of low back pain with massage of the buttocks
muscles using a
Piriformis Gluteus Medius Trigger Point Ball Massage
The illustration shows treatment of low back pain with massage of the buttocks
muscles using a  Trigger Point Therapy
==============================================================================
Note from this page web designer: I must look at all available options in order
to get the cure for chronic pain of Piriformis Syndrome, and why not try it if
it does not require surgery? I do know I will definitely give it a chance.
An observation: Most Doctors just know about one type of specialty and do
not study the others so they cannot speak to you about a variety of cures
for a given disease or injury. This is where the problem lies. The layman
must do his own research or suffer injury forever. That is why I have
compiled the above information about Piriformis Syndrome and possible
treatments that are available.
I have not tried The Trigger Point Therapy technique with the tennis ball,
or acupuncture or acupressure but have tried back surgery, piriformis surgery,
aqua therapy, physical therapy, stretching, weights, walking, traction, steroids,
cortisone shots and lidocaine shots and lidocaine pain patches.
=============================================================================
* December 28, 2004 - Lidocaine Patch Works! Knocks the pain down some what in
leg. Numbs the area so that the pain is decreased giving me some relief...
I am using the Lidoderm patches, (Active Ingredient: 5% Lidocaine), once a day
for 11 hours per day which is the maximum usage amount of time. I am getting
some relief from this treatment.
Trigger Point Therapy
==============================================================================
Note from this page web designer: I must look at all available options in order
to get the cure for chronic pain of Piriformis Syndrome, and why not try it if
it does not require surgery? I do know I will definitely give it a chance.
An observation: Most Doctors just know about one type of specialty and do
not study the others so they cannot speak to you about a variety of cures
for a given disease or injury. This is where the problem lies. The layman
must do his own research or suffer injury forever. That is why I have
compiled the above information about Piriformis Syndrome and possible
treatments that are available.
I have not tried The Trigger Point Therapy technique with the tennis ball,
or acupuncture or acupressure but have tried back surgery, piriformis surgery,
aqua therapy, physical therapy, stretching, weights, walking, traction, steroids,
cortisone shots and lidocaine shots and lidocaine pain patches.
=============================================================================
* December 28, 2004 - Lidocaine Patch Works! Knocks the pain down some what in
leg. Numbs the area so that the pain is decreased giving me some relief...
I am using the Lidoderm patches, (Active Ingredient: 5% Lidocaine), once a day
for 11 hours per day which is the maximum usage amount of time. I am getting
some relief from this treatment.
 Lidocaine Patch
The Lidoderm® patch contains lidocaine and is applied directly to intact
skin to treat the neuropathic pain associated with postherpetic neuralgia
(PHN). Learn more about postherpetic neuralgia, shingles, and instructions
=============================================================================
The Lidoderm® patch provides targeted peripheral analgesia for the neuropathic
pain associated with postherpetic neuralgia. Learn more about Lidoderm® patch
clinical studies, its site of action, postherpetic neuralgia, and our patient
education tools.
Here are the results to the new Lidoderm patch with 5% Lidocaine which I am
told is the way of the future for pain relief.
Lidoderm
lidocaine topical (LYE doe cane)
Anestacon, Bactine, Dermaflex, Ela-Max, Ela-Max 5, Ela-Max Plus, Lida Mantle,
Lidocaine Viscous, Lidoderm, Lidomar, Medi-Quik Spray, Protech First Aid Stik,
Solarcaine, Xylocaine 10% Oral, Xylocaine Jelly, Xylocaine Topical, Xylocaine
Viscous, Zilactin-L
What is the most important information I should know about Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
What is Lidoderm?
o Lidocaine causes loss of feeling (numbness) of skin and mucous membranes.
o Lidoderm is used to relieve pain associated with sunburn; insect bites;
poison ivy; poison oak; poison sumac; minor cuts; scratches; and burns; sores
in the mouth; dental procedures; hemorrhoids; and shingles (herpes infection).
o Lidoderm may also be used for purposes other than those listed here.
What should I discuss with my healthcare provider before using Lidoderm?
o Before using Lidoderm, talk to your healthcare provider if you have
· liver problems;
· other serious medical conditions; or
· broken, inflamed, or damaged skin (lidocaine patches).
o You may not be able to use Lidoderm, or you may require a dosage adjustment
or special monitoring during treatment.
o Lidoderm is in the FDA pregnancy category B. This means that it is unlikely
to be harmful to an unborn baby. Do not use Lidoderm without first talking to
your doctor if you are pregnant or could become pregnant during treatment.
o Lidoderm passes into breast milk and may affect a nursing baby. Do not use
Lidoderm without first talking to your doctor if you are breast-feeding.
How should I use Lidoderm?
o Use Lidoderm exactly as directed. If you do not understand these instructions,
ask your doctor, nurse, or pharmacist to explain them to you.
o Lidoderm is intended for external use on the skin only. Do not swallow the
medication (unless specifically directed to do so by your doctor if treating a
throat condition).
o Lidoderm may be applied using the finger tips or a cotton swab. Apply the
medication as directed by your healthcare provider.
o Lidocaine oral cavity patches are applied to the gums by a dentist or a
dental assistant before a dental procedure.
o Lidocaine solution can be swished around the mouth or gargled, and then
spat out. Use a dose-measuring spoon or cup to measure the solution. Ask your
pharmacist if you do not have one.
o Shake the oral spray well before use. Do not inhale the spray.
o Apply the lidocaine patches as directed by your doctor. Make sure the skin
does not have any open sores or rashes. You may apply up to 3 patches at one
time. Leave the patches on for only 12 hours during a 24-hour period. Patches
may be cut into smaller sizes with scissors before removing the adhesive liner.
Clothing may be worn over the patches. If irritation or burning occurs due to
the patch, remove it and do not reapply until the irritation subsides. Dispose
of used lidocaine topical patches where they cannot be reached by children or pets.
o Do not use Lidoderm more often or for longer than is directed. Talk to your
healthcare provider if your symptoms do not improve or if they worsen.
o Store Lidoderm at room temperature away from moisture and heat, out of the
reach of children and pets.
What happens if I miss a dose?
o Apply the missed dose as soon as you remember. If it is almost time for the
next dose, skip the missed dose and use the next regularly scheduled dose as
directed. Do not apply a double dose of this medication.
What happens if I overdose?
o Seek emergency medical attention if an overdose is suspected or if the
medication has been ingested.
o Symptoms of a Lidoderm overdose may include dizziness, drowsiness, confusion,
nervousness, ringing in the ears, blurred or double vision, sensation of heat
or cold, numbness, twitching, seizures, unconsciousness, decreased breathing,
and heart attack.
What should I avoid while using Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
o Since there will be decreased sensation of the skin where Lidoderm is
applied, use caution to avoid injury of the area during treatment.
What are the possible side effects of Lidoderm?
o Stop using Lidoderm and seek emergency medical attention or contact your
doctor immediately if you experience any of the following rare but serious
side effects:
· an allergic reaction (difficulty breathing; closing of the throat;
swelling of the lips, tongue, or face; or hives);;
· chest pain or irregular heartbeats;
· dizziness or drowsiness;
· nausea or vomiting;
· trembling, shaking, or seizures (convulsions); or
· blurred or double vision.
o Other less serious side effects may be more likely to occur. Continue to
use Lidoderm and talk to your healthcare provider if you experience
· mild irritation, redness, or swelling at the application site.
o Side effects other than those listed here may also occur. Continue to use
Lidoderm and talk to your doctor about any side effect that seems unusual or
that is especially bothersome.
What other drugs will affect Lidoderm?
o Although Lidoderm is unlikely to affect medicines taken by mouth, talk
to your doctor before using Lidoderm if you are taking digoxin (Lanoxin)
or any medicine to control irregular heartbeats. You may not be able to use
Lidoderm, or you may require a dosage adjustment or special monitoring.
o Avoid using other topical medications on the affected area without first
talking to your doctor.
o Drugs other than those listed here may also interact with Lidoderm. Talk
to your doctor and pharmacist before taking or using any other prescription or
over-the-counter medicines, including vitamins, minerals, and herbal products.
Where can I get more information?
o Your pharmacist has additional information about Lidoderm written for
health professionals that you may read.
--------------------------------------------------------------------------------
o Remember, keep this and all other medicines out of the reach of children,
never share your medicines with others, and use this medication only for the
indication prescribed.
o Every effort has been made to ensure that the information provided by
Cerner Multum, Inc. ('Multum') is accurate, up-to-date, and complete, but
no guarantee is made to that effect. Drug information contained herein may
be time sensitive. Multum information has been compiled for use by healthcare
practitioners and consumers in the United States and therefore Multum does not
warrant that uses outside of the United States are appropriate, unless specifically
indicated otherwise. Multum's drug information does not endorse drugs, diagnose
patients or recommend therapy. Multum's drug information is an informational
resource designed to assist licensed healthcare practitioners in caring for
their patients and/or to serve consumers viewing this service as a supplement
to, and not a substitute for, the expertise, skill, knowledge and judgment
of healthcare practitioners. The absence of a warning for a given drug or
drug combination in no way should be construed to indicate that the drug or
drug combination is safe, effective or appropriate for any given patient.
Multum does not assume any responsibility for any aspect of healthcare
administered with the aid of information Multum provides. The information
contained herein is not intended to cover all possible uses, directions,
precautions, warnings, drug interactions, allergic reactions, or adverse
effects. If you have questions about the drugs you are taking, check with
your doctor, nurse or pharmacist.
=============================================================================
Directions of Lidoderm within Lidocaine Patch Box:
* ENDO Pharmaceuticals
Lidoderm
(Lidocaine Patch 5%)
Rx only
Description:
LIDODERM (lidocaine patch 5%) is comprised of an adhesive material containing 5%
lidocaine, which is applied to non-woven polyester felt backing and covered with
polyethylene terephthalate (PET) film release liner. The release liner is removed
prior to application to the skin. The size of the patch is 10 cm x 14 cm.
Lidocaine is chemically designated as acetamide, 2-(diethylamino)-N-(2,2-dimethylphenyl),
has an octanol: water partition ratio 43 at pH 7.4, and has the following structure:
CH
/ 3 C H
--- / 2 5
/ \_____NH-CO-CH--N
\ / 2 \
--- C H
\ 2 5
CH
3
Each adhesive patch contains 700 mg of lidocaine (50 mg per ram adhesive) in an
aqueous base. It also contains the following inactive ingredients: dihydroxyaluminim
aminoacetate, disodium edetate, gelatin, glycerin, kaolin, methylparaben, polyacrylic
acid, polyvinyl alcohol, propylene glycol, propylparaben, sodium carboxymethylcellulose,
sodium polyacrylate, D-sorbitol, tartaric acid, and urea.
CLINAL PHARMACOLOGY
Pharmacodynamics:
Lidocaine is an amide-type local anesthetic agent and is suggested to stabilize neuronal
membranes by inhibiting the ionic fluxes required for the initiation and conduction of
impulses.
The penetration of lidocaine into intact skin after application of LIDODERM
is sufficient to produce an analgesic effect, unless than the amount necessary
to produce a complete sensory block.
Pharmacokinetics:
Absorption: The amount of lidocaine systemically absorbed from LIDODERM is directly
related to both the duration of application and the surface area over which it is
applied. In a pharmacokinetic study, three LIDODERM patches were applied over an
area of 420 cm2 of intact skin on the back of normal volunteers for 12 hours. Blood
samples were withdrawn for determination of lidocaine concentration during the
application and for 12 hours after removal of patches. The results are summarized
in Table 1.
CAUTION: This table is incorrect because certain math symbols and notations
are not available in my word processing application. Not to be used for any
medical concerns. Speak to a Doctor before doing anything with Lidocaine.
Lidoderm Application Area Dose C(max) T(max)
Patch Site (cm2) Absorbed (mg) (ug/mL) (hr)
3 patches Back 420 64 + 32 0.3 + 0.06 11 hr
(2100 mg)
When LIDODERM is used according to the recommendation dosing instructions, only
3 + 2% of the dose applied is expected to be absorbed. At least 95% (665 mg)
of lidocaine will remain in a used patch. Mean peak blood concentration of
lidocaine is about 0.13 ug/mL (about 1/10 of the therapeutic concentration
required to treat cardiac arrhythmias). Repeated application of three
patches simultaneously for 12 hours (recommended maximum daily dose), once
per day for three days, indicated that the lidocaine concentration does not
increase with daily use. The mean plasma pharmacokinetic profile for the
15 healthy volunteers are shown in Figure 1.
Figure 1
Mean lidocaine blood concentration after three consecutive daily applications
of three IDODERM patches simultaneously for 12 hours per day in healthy volunteers
(n=15).
=============================================================================
120 . .
. . . . .
100 . . .. . . .
. . . . . .
80 . . . . . .
. . . . . .
60 . . . . . .
. . . . . .
40 . .. . .. . .
. . . . ..
20 .
.
0 .
.
0 6 12 18 24 30 36 42 48 54 60 66 72
HOURS
=============================================================================
DISTRIBUTION:
When lidocaine is administered intravenously to healthy volunteers,
the volume of distribution is 0.7 to 2.7 L/kg (mean 1.5 + 0.6 SD, n=15) At
concentrations produced by application of LIDODEERM, lidocaine is approximately
70% bound to plasma proteins, primarily alpha-1-acid glycoprotein. At much
higher plasma concentrations (1 to 4 ug/mL of free base), the plasma protein
binding of lidocaine is concentration dependent. Lidocaine crosses the
placental and blood brain barriers, presumably by passive diffusion.
METABOLISM:
It is not known if lidocaine is metabolized in the skin. Lidocaine is
metabolized rapidly by the liver to a number of metabolites, including
monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have
pharmacologic activity similar to, but less potent than that of lidocaine.
A minor metabolite, 2,6-xylidine, has unknown pharmacologic activity but is
carcinogenic in rats. The blood concentration of this metabolite is
negligible following ap0plication of LIDODERM (lidocaine patch 5%). Following
intravenous administration, MEGX and GX concentrations in serum range from
11 to 36% and from 5 to 11% of lidocaine concentrations, respectively.
Excretion: Lidocaine and its metabolites are excreted by the kidneys. Less
than 10% of lidocaine is excreted unchanged. The half-life of lidocaine
elimination from the plasma following IV administration is 81 to 149 minutes
(mean 107 + 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min
(mean 0.64 + 0.18 SD, n = 15).
CLINICAL STUDIES
Single-dose treatment with LIDODERM was compared to treatment with vehicle patch
(without lidocaine), and to no treatment (observation only) in a double-blind,
crossover clinical trial with 35 post-herpetic neuralgia patients. Pain
intensity and pain relief scores were evaluated periodically for 12 hours.
LIDODERM performed statistically better than vehicle patch in terms of pain
intensity from 4 to 12 hours.
Multiple-dose, two-week treatment with LIDODERM was compared to vehicle patch
(without lidocaine) in a double-blind, crossover clinical trial of withdrawal type
design conducted in 32 patients, who were considered as responders to the open-
label use of LIDODERM prior to the study. The constant type of pain was
evaluated but not the pain induced by sensory stimuli (dysesthesia). Statistically
significant difference favoring LIDODERM were observed in terms of time to
exit from the trial (14 versus 3.8 days at p-value 0.001), daily average pain
relief, and patient's preference of treatment. About half of the patients also
took oral medications commonly used in the treatment of post-herpetic neuralgia.
The extent of use of concomitant me3dication was similar in the two treatment
groups.
INDICATION AND USAGE
LIDODERM is indicated for relief of pain associated with post-herpetic neuralgia.
It should be applied only to intact skin.
CONTRAINDICATIONS:
LIDODERM is contraindicated in patients with a known history of sensitivity to
local anesthetics of the amide type, or to any other component of the product.
WARNINGS:
Accidental Exposure to Children:
Even a used LIDODERM patch contains a large amount of lidocaine (at least 665 mg).
The potential exists for a small child or a pet to suffer serious adverse effects
from chewing or ingesting a new or used LIDODERM patch, although the risk with this
formulation has not been evaluated. It is important for patients to store and dispose
of LIDODERM out of the reach of children and pets.
Excessive Dosing:
Excessive dosing by applying LIDODERM to larger areas or for longer than the
recommended wearing time could result in increased absorption of lidocaine and
high blood concentrations, leading to serious adverse effects (see ADVERSE REACTIONS,
Systemic Reactions). Lidocaine toxicity could be expected at lidocaine blood
concentrations above 5 ug/mL. The blood application of more than the recommended
number of patches, small patients, or impaired elimination may all contribute to
increasing the blood concentration of lidocaine. With recommended dosing of LIDODERM,
the average peak blood concentration is about 0.13 ug/mL, but concentrations
higher than 0.25 ug/mL have been observed in some individuals.
PRECAUTIONS:
General
Hepatic Disease: Patients with severe hepatic disease are at greater risk of developing
toxic blood concentrations of lidocaine because of their inability to metabolize
lidocaine normally.
Allergic Reactions: Patients allergic to para-aminobenzoic acid derivatives (procaine,
tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
However, LIDODERM should be used with caution in patients with a history of drug
sensitivities, especially if the etiologic agent is uncertain.
Non-Intact Skin: Application to broken or inflamed skin, although not tested, may
result in higher blood concentration of lidocaine from increased absorption.
LIDODERM is only recommended for use on intact skin.
Eye Exposure: The contact of LIDODERM with eyes, although not studied, should be
avoided based on the findings of severe eye irritation with the use of similar
products in animals. If eye contact occurs, immediately wash out the eye with water
or saline and protect the eye until sensation returns.
There are many more precautions: Please read your Prescription label and text of
directions and usage.
Drug Interactions
Antiarrhythmic Drugs: LIDODERM should be used with caution in patients receiving
Class I antiarrhymthmic drugs (such as tocainide and mexiletine) since the toxic
effects are additive and potentially synergistic.
Local Anesthetics
When LIDODERM is used concomitantly with other products containing local anesthetic
agents, the amount absorbed from all formulations must be considered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogensis: A minor metabolite, 2.6-xylidine, has been found to be carcinogenic
in rats. The blood concentration of this metabolite is negligible following
application of LIDODERM.
Mutagenesis: Lidocaine HCI is not mutagenic in Salmonella/mammalian microsome test
nor clastogenic in chromosome aberration assay with human lymphocytes and mouse
micronucleus test.
Impairment of Fertility:
The effect of LIDODERM on fertility as not been studied.
Pregnancy
Teratogenic Effects: Pregnancy Category B.
LIDODERM (lidocaine patch 5%) has not been studied in pregnancy, Reproduction studies
with lidocaine have been performed in rats at doses up to 30 mg/kg subcutaneously
and have revealed no evidence of harm to the fetus due to lidocaine. There are,
however, no adequate and well-controlled studies in pregnant women. Because
animal reproduction studies are not always predictive of human response, LIDODERM
should be use during pregnancy only if clearly needed.
Labor and Delivery
LIDODERM has not been studied in Labor and delivery. Licocaine is not contraindicated
in labor and delivery. Should LIDODERM be used concomitantly with other products
containing lidocaine, total doses contributed by all formulations must be
considered.
Nursing Mothers:
LIDODERM has not been studied in nursing mothers. Lidocaine is excreted in human
mild, and the milk: plasma ratio of lidocaine is 0.45 Caution should be exercised
when LIDODERM is admistered to a nursing woman.
Pediatric USE
Safety and effectiveness in pediatric patients have not been established.
ADVERSE REACTIONS
Localized Reactions
During or immediately after treatment with LIDODERM (lidocaine patch 5%), the skin at
the stie of treatment may develop erythema or edema or may be the locus of abnormal
sensation. These reactions are generally mild and transient, resolving
spontaneously within a few minutes to hours. In clinical studies with LIDODERM,
there were no serious reactions reported. One out of 150 subjects in a three-
week study was discontinued from treatment because of a skin reaction
(erythema and hives).
Allergic Reactions:
Allergic and anaphylactoid reactions associated with lidocaine, although rare, can
occur. They are characterized by urticaria, angioedema, bronchospasm, and shock.
If they occur, they should be managed by conventional means. The detection of
sensitivity by skin testing is of doubtful value.
Systemic (Dose-Related) Reactions
Systemic adverse reactions following appropriate use of LIDODERM are likely, due to
the small dose absorbed (See CLINICAL PHARMACOLOGY, Pharmacokinetics), Systemic
adverse effects of lidocaine are similar in nature to those observed with other
PHARMACOLOGY, Pharmacokinetics). Systemic adverse effects oflidocaieare similar in
nature to those observed with other amide local anesthetic agents, including CNS
excitation and/or depression (light-headedness, nervousness, apprehension, twitching,
tremors, convulsions, unconsciousness, respiratory depression and arrest).
Excitatory CNS reactions may be brief or not occur at all, in which case the
first manifestation may be drowsiness merging into unconsciousness. Cardiovascular
manifestations may include bradycardia, hypotension and cardiovascular collapse
leading to arrest.
OVERDOSAGE:
Lidocaine overdose from cutaneous absorption is rare, but could occur. If there is
any suspicion of lidocaine overdose (see ADVERSE REACTIONS, Systemic Reactions), drug
blood concentration should be checked. The management of overdose includes close
monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible
value in the treatment of acute overdose with lidocaine.
In the absence of massive topical overdose or oral ingestion, evaluation of symptoms
of toxicity should include consideration of other etiologies for the clinical effects,
or over dosage from other sources of lidocaine or other local anesthetics.
The oral LD50 of lidocaine HCI is 459 (346-773) mg/kg (as the salt) in non-fasted
female rats and 214 (159-324) mg/kg (as the salt) in fasted female rats, which are
equivalent to roughly 4000 mg, respectively, in a 60 to 70 kg man based on the
equivalent surface area dosage conversion factors between species.
DOSAGE AND ADMINISTRATION:
Apply LIDODERM to intact skin to cover the most painful areas. Apply up to three
patches, only once for up to 12 hours within a 24-hour period. Patches may be cut
into smaller sizes with scissors prior to removal of the release liner. Clothing
may be worn over the area of application. Smaller areas of treatment are recommended
in a debilitated patient, or a patient with impaired elimination.
If irritated or a burning sensation occurs during application, remove the patch(es)
and do not reapply until the irritation subsides.
When LIDODERM is used concomitantly with other products containing local enesthetic
agents, the amount absorbed from all formulations must be considered.
HANDLING AND DISPOSAL:
Hands should be washed after the handling of LIDODERM, and eye contact with LIDODERM
should be avoided. The used patch should be immediately disposed of in such a way
as to prevent its access by children and pets.
HOW SUPPLIED:
LIDODERM (Lidocaine patch 5%) is available as the following:
Carton of 30 patches, packaged into individual child-resistant envelopes
Store at 25C (77 degrees) excursions permitted to 15 to 30 Celsius (59 degree to
86 degree farenheight) See USP Controlled Room Temperature).
Manufactured for:
Endo Pharmaceutical Inc. ENDO
Chadds Ford, Pennsylvania 19317
LIDODERM is a Registered Trademark of Hind Health Care, INC.
=============================================================================
A pressure point procedure found on the internet to help another patient
of piriformis problems in which the Piriformis Muscle needed to be stretched
out back to its original length -- Here is the therapy for that below:
=============================================================================
Sciatica? Piriformis? This helped me
Lidocaine Patch
The Lidoderm® patch contains lidocaine and is applied directly to intact
skin to treat the neuropathic pain associated with postherpetic neuralgia
(PHN). Learn more about postherpetic neuralgia, shingles, and instructions
=============================================================================
The Lidoderm® patch provides targeted peripheral analgesia for the neuropathic
pain associated with postherpetic neuralgia. Learn more about Lidoderm® patch
clinical studies, its site of action, postherpetic neuralgia, and our patient
education tools.
Here are the results to the new Lidoderm patch with 5% Lidocaine which I am
told is the way of the future for pain relief.
Lidoderm
lidocaine topical (LYE doe cane)
Anestacon, Bactine, Dermaflex, Ela-Max, Ela-Max 5, Ela-Max Plus, Lida Mantle,
Lidocaine Viscous, Lidoderm, Lidomar, Medi-Quik Spray, Protech First Aid Stik,
Solarcaine, Xylocaine 10% Oral, Xylocaine Jelly, Xylocaine Topical, Xylocaine
Viscous, Zilactin-L
What is the most important information I should know about Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
What is Lidoderm?
o Lidocaine causes loss of feeling (numbness) of skin and mucous membranes.
o Lidoderm is used to relieve pain associated with sunburn; insect bites;
poison ivy; poison oak; poison sumac; minor cuts; scratches; and burns; sores
in the mouth; dental procedures; hemorrhoids; and shingles (herpes infection).
o Lidoderm may also be used for purposes other than those listed here.
What should I discuss with my healthcare provider before using Lidoderm?
o Before using Lidoderm, talk to your healthcare provider if you have
· liver problems;
· other serious medical conditions; or
· broken, inflamed, or damaged skin (lidocaine patches).
o You may not be able to use Lidoderm, or you may require a dosage adjustment
or special monitoring during treatment.
o Lidoderm is in the FDA pregnancy category B. This means that it is unlikely
to be harmful to an unborn baby. Do not use Lidoderm without first talking to
your doctor if you are pregnant or could become pregnant during treatment.
o Lidoderm passes into breast milk and may affect a nursing baby. Do not use
Lidoderm without first talking to your doctor if you are breast-feeding.
How should I use Lidoderm?
o Use Lidoderm exactly as directed. If you do not understand these instructions,
ask your doctor, nurse, or pharmacist to explain them to you.
o Lidoderm is intended for external use on the skin only. Do not swallow the
medication (unless specifically directed to do so by your doctor if treating a
throat condition).
o Lidoderm may be applied using the finger tips or a cotton swab. Apply the
medication as directed by your healthcare provider.
o Lidocaine oral cavity patches are applied to the gums by a dentist or a
dental assistant before a dental procedure.
o Lidocaine solution can be swished around the mouth or gargled, and then
spat out. Use a dose-measuring spoon or cup to measure the solution. Ask your
pharmacist if you do not have one.
o Shake the oral spray well before use. Do not inhale the spray.
o Apply the lidocaine patches as directed by your doctor. Make sure the skin
does not have any open sores or rashes. You may apply up to 3 patches at one
time. Leave the patches on for only 12 hours during a 24-hour period. Patches
may be cut into smaller sizes with scissors before removing the adhesive liner.
Clothing may be worn over the patches. If irritation or burning occurs due to
the patch, remove it and do not reapply until the irritation subsides. Dispose
of used lidocaine topical patches where they cannot be reached by children or pets.
o Do not use Lidoderm more often or for longer than is directed. Talk to your
healthcare provider if your symptoms do not improve or if they worsen.
o Store Lidoderm at room temperature away from moisture and heat, out of the
reach of children and pets.
What happens if I miss a dose?
o Apply the missed dose as soon as you remember. If it is almost time for the
next dose, skip the missed dose and use the next regularly scheduled dose as
directed. Do not apply a double dose of this medication.
What happens if I overdose?
o Seek emergency medical attention if an overdose is suspected or if the
medication has been ingested.
o Symptoms of a Lidoderm overdose may include dizziness, drowsiness, confusion,
nervousness, ringing in the ears, blurred or double vision, sensation of heat
or cold, numbness, twitching, seizures, unconsciousness, decreased breathing,
and heart attack.
What should I avoid while using Lidoderm?
o Do not use Lidoderm more often or for longer than is directed. Talk to
your healthcare provider if your symptoms do not improve or if they worsen.
o Since there will be decreased sensation of the skin where Lidoderm is
applied, use caution to avoid injury of the area during treatment.
What are the possible side effects of Lidoderm?
o Stop using Lidoderm and seek emergency medical attention or contact your
doctor immediately if you experience any of the following rare but serious
side effects:
· an allergic reaction (difficulty breathing; closing of the throat;
swelling of the lips, tongue, or face; or hives);;
· chest pain or irregular heartbeats;
· dizziness or drowsiness;
· nausea or vomiting;
· trembling, shaking, or seizures (convulsions); or
· blurred or double vision.
o Other less serious side effects may be more likely to occur. Continue to
use Lidoderm and talk to your healthcare provider if you experience
· mild irritation, redness, or swelling at the application site.
o Side effects other than those listed here may also occur. Continue to use
Lidoderm and talk to your doctor about any side effect that seems unusual or
that is especially bothersome.
What other drugs will affect Lidoderm?
o Although Lidoderm is unlikely to affect medicines taken by mouth, talk
to your doctor before using Lidoderm if you are taking digoxin (Lanoxin)
or any medicine to control irregular heartbeats. You may not be able to use
Lidoderm, or you may require a dosage adjustment or special monitoring.
o Avoid using other topical medications on the affected area without first
talking to your doctor.
o Drugs other than those listed here may also interact with Lidoderm. Talk
to your doctor and pharmacist before taking or using any other prescription or
over-the-counter medicines, including vitamins, minerals, and herbal products.
Where can I get more information?
o Your pharmacist has additional information about Lidoderm written for
health professionals that you may read.
--------------------------------------------------------------------------------
o Remember, keep this and all other medicines out of the reach of children,
never share your medicines with others, and use this medication only for the
indication prescribed.
o Every effort has been made to ensure that the information provided by
Cerner Multum, Inc. ('Multum') is accurate, up-to-date, and complete, but
no guarantee is made to that effect. Drug information contained herein may
be time sensitive. Multum information has been compiled for use by healthcare
practitioners and consumers in the United States and therefore Multum does not
warrant that uses outside of the United States are appropriate, unless specifically
indicated otherwise. Multum's drug information does not endorse drugs, diagnose
patients or recommend therapy. Multum's drug information is an informational
resource designed to assist licensed healthcare practitioners in caring for
their patients and/or to serve consumers viewing this service as a supplement
to, and not a substitute for, the expertise, skill, knowledge and judgment
of healthcare practitioners. The absence of a warning for a given drug or
drug combination in no way should be construed to indicate that the drug or
drug combination is safe, effective or appropriate for any given patient.
Multum does not assume any responsibility for any aspect of healthcare
administered with the aid of information Multum provides. The information
contained herein is not intended to cover all possible uses, directions,
precautions, warnings, drug interactions, allergic reactions, or adverse
effects. If you have questions about the drugs you are taking, check with
your doctor, nurse or pharmacist.
=============================================================================
Directions of Lidoderm within Lidocaine Patch Box:
* ENDO Pharmaceuticals
Lidoderm
(Lidocaine Patch 5%)
Rx only
Description:
LIDODERM (lidocaine patch 5%) is comprised of an adhesive material containing 5%
lidocaine, which is applied to non-woven polyester felt backing and covered with
polyethylene terephthalate (PET) film release liner. The release liner is removed
prior to application to the skin. The size of the patch is 10 cm x 14 cm.
Lidocaine is chemically designated as acetamide, 2-(diethylamino)-N-(2,2-dimethylphenyl),
has an octanol: water partition ratio 43 at pH 7.4, and has the following structure:
CH
/ 3 C H
--- / 2 5
/ \_____NH-CO-CH--N
\ / 2 \
--- C H
\ 2 5
CH
3
Each adhesive patch contains 700 mg of lidocaine (50 mg per ram adhesive) in an
aqueous base. It also contains the following inactive ingredients: dihydroxyaluminim
aminoacetate, disodium edetate, gelatin, glycerin, kaolin, methylparaben, polyacrylic
acid, polyvinyl alcohol, propylene glycol, propylparaben, sodium carboxymethylcellulose,
sodium polyacrylate, D-sorbitol, tartaric acid, and urea.
CLINAL PHARMACOLOGY
Pharmacodynamics:
Lidocaine is an amide-type local anesthetic agent and is suggested to stabilize neuronal
membranes by inhibiting the ionic fluxes required for the initiation and conduction of
impulses.
The penetration of lidocaine into intact skin after application of LIDODERM
is sufficient to produce an analgesic effect, unless than the amount necessary
to produce a complete sensory block.
Pharmacokinetics:
Absorption: The amount of lidocaine systemically absorbed from LIDODERM is directly
related to both the duration of application and the surface area over which it is
applied. In a pharmacokinetic study, three LIDODERM patches were applied over an
area of 420 cm2 of intact skin on the back of normal volunteers for 12 hours. Blood
samples were withdrawn for determination of lidocaine concentration during the
application and for 12 hours after removal of patches. The results are summarized
in Table 1.
CAUTION: This table is incorrect because certain math symbols and notations
are not available in my word processing application. Not to be used for any
medical concerns. Speak to a Doctor before doing anything with Lidocaine.
Lidoderm Application Area Dose C(max) T(max)
Patch Site (cm2) Absorbed (mg) (ug/mL) (hr)
3 patches Back 420 64 + 32 0.3 + 0.06 11 hr
(2100 mg)
When LIDODERM is used according to the recommendation dosing instructions, only
3 + 2% of the dose applied is expected to be absorbed. At least 95% (665 mg)
of lidocaine will remain in a used patch. Mean peak blood concentration of
lidocaine is about 0.13 ug/mL (about 1/10 of the therapeutic concentration
required to treat cardiac arrhythmias). Repeated application of three
patches simultaneously for 12 hours (recommended maximum daily dose), once
per day for three days, indicated that the lidocaine concentration does not
increase with daily use. The mean plasma pharmacokinetic profile for the
15 healthy volunteers are shown in Figure 1.
Figure 1
Mean lidocaine blood concentration after three consecutive daily applications
of three IDODERM patches simultaneously for 12 hours per day in healthy volunteers
(n=15).
=============================================================================
120 . .
. . . . .
100 . . .. . . .
. . . . . .
80 . . . . . .
. . . . . .
60 . . . . . .
. . . . . .
40 . .. . .. . .
. . . . ..
20 .
.
0 .
.
0 6 12 18 24 30 36 42 48 54 60 66 72
HOURS
=============================================================================
DISTRIBUTION:
When lidocaine is administered intravenously to healthy volunteers,
the volume of distribution is 0.7 to 2.7 L/kg (mean 1.5 + 0.6 SD, n=15) At
concentrations produced by application of LIDODEERM, lidocaine is approximately
70% bound to plasma proteins, primarily alpha-1-acid glycoprotein. At much
higher plasma concentrations (1 to 4 ug/mL of free base), the plasma protein
binding of lidocaine is concentration dependent. Lidocaine crosses the
placental and blood brain barriers, presumably by passive diffusion.
METABOLISM:
It is not known if lidocaine is metabolized in the skin. Lidocaine is
metabolized rapidly by the liver to a number of metabolites, including
monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have
pharmacologic activity similar to, but less potent than that of lidocaine.
A minor metabolite, 2,6-xylidine, has unknown pharmacologic activity but is
carcinogenic in rats. The blood concentration of this metabolite is
negligible following ap0plication of LIDODERM (lidocaine patch 5%). Following
intravenous administration, MEGX and GX concentrations in serum range from
11 to 36% and from 5 to 11% of lidocaine concentrations, respectively.
Excretion: Lidocaine and its metabolites are excreted by the kidneys. Less
than 10% of lidocaine is excreted unchanged. The half-life of lidocaine
elimination from the plasma following IV administration is 81 to 149 minutes
(mean 107 + 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min
(mean 0.64 + 0.18 SD, n = 15).
CLINICAL STUDIES
Single-dose treatment with LIDODERM was compared to treatment with vehicle patch
(without lidocaine), and to no treatment (observation only) in a double-blind,
crossover clinical trial with 35 post-herpetic neuralgia patients. Pain
intensity and pain relief scores were evaluated periodically for 12 hours.
LIDODERM performed statistically better than vehicle patch in terms of pain
intensity from 4 to 12 hours.
Multiple-dose, two-week treatment with LIDODERM was compared to vehicle patch
(without lidocaine) in a double-blind, crossover clinical trial of withdrawal type
design conducted in 32 patients, who were considered as responders to the open-
label use of LIDODERM prior to the study. The constant type of pain was
evaluated but not the pain induced by sensory stimuli (dysesthesia). Statistically
significant difference favoring LIDODERM were observed in terms of time to
exit from the trial (14 versus 3.8 days at p-value 0.001), daily average pain
relief, and patient's preference of treatment. About half of the patients also
took oral medications commonly used in the treatment of post-herpetic neuralgia.
The extent of use of concomitant me3dication was similar in the two treatment
groups.
INDICATION AND USAGE
LIDODERM is indicated for relief of pain associated with post-herpetic neuralgia.
It should be applied only to intact skin.
CONTRAINDICATIONS:
LIDODERM is contraindicated in patients with a known history of sensitivity to
local anesthetics of the amide type, or to any other component of the product.
WARNINGS:
Accidental Exposure to Children:
Even a used LIDODERM patch contains a large amount of lidocaine (at least 665 mg).
The potential exists for a small child or a pet to suffer serious adverse effects
from chewing or ingesting a new or used LIDODERM patch, although the risk with this
formulation has not been evaluated. It is important for patients to store and dispose
of LIDODERM out of the reach of children and pets.
Excessive Dosing:
Excessive dosing by applying LIDODERM to larger areas or for longer than the
recommended wearing time could result in increased absorption of lidocaine and
high blood concentrations, leading to serious adverse effects (see ADVERSE REACTIONS,
Systemic Reactions). Lidocaine toxicity could be expected at lidocaine blood
concentrations above 5 ug/mL. The blood application of more than the recommended
number of patches, small patients, or impaired elimination may all contribute to
increasing the blood concentration of lidocaine. With recommended dosing of LIDODERM,
the average peak blood concentration is about 0.13 ug/mL, but concentrations
higher than 0.25 ug/mL have been observed in some individuals.
PRECAUTIONS:
General
Hepatic Disease: Patients with severe hepatic disease are at greater risk of developing
toxic blood concentrations of lidocaine because of their inability to metabolize
lidocaine normally.
Allergic Reactions: Patients allergic to para-aminobenzoic acid derivatives (procaine,
tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine.
However, LIDODERM should be used with caution in patients with a history of drug
sensitivities, especially if the etiologic agent is uncertain.
Non-Intact Skin: Application to broken or inflamed skin, although not tested, may
result in higher blood concentration of lidocaine from increased absorption.
LIDODERM is only recommended for use on intact skin.
Eye Exposure: The contact of LIDODERM with eyes, although not studied, should be
avoided based on the findings of severe eye irritation with the use of similar
products in animals. If eye contact occurs, immediately wash out the eye with water
or saline and protect the eye until sensation returns.
There are many more precautions: Please read your Prescription label and text of
directions and usage.
Drug Interactions
Antiarrhythmic Drugs: LIDODERM should be used with caution in patients receiving
Class I antiarrhymthmic drugs (such as tocainide and mexiletine) since the toxic
effects are additive and potentially synergistic.
Local Anesthetics
When LIDODERM is used concomitantly with other products containing local anesthetic
agents, the amount absorbed from all formulations must be considered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogensis: A minor metabolite, 2.6-xylidine, has been found to be carcinogenic
in rats. The blood concentration of this metabolite is negligible following
application of LIDODERM.
Mutagenesis: Lidocaine HCI is not mutagenic in Salmonella/mammalian microsome test
nor clastogenic in chromosome aberration assay with human lymphocytes and mouse
micronucleus test.
Impairment of Fertility:
The effect of LIDODERM on fertility as not been studied.
Pregnancy
Teratogenic Effects: Pregnancy Category B.
LIDODERM (lidocaine patch 5%) has not been studied in pregnancy, Reproduction studies
with lidocaine have been performed in rats at doses up to 30 mg/kg subcutaneously
and have revealed no evidence of harm to the fetus due to lidocaine. There are,
however, no adequate and well-controlled studies in pregnant women. Because
animal reproduction studies are not always predictive of human response, LIDODERM
should be use during pregnancy only if clearly needed.
Labor and Delivery
LIDODERM has not been studied in Labor and delivery. Licocaine is not contraindicated
in labor and delivery. Should LIDODERM be used concomitantly with other products
containing lidocaine, total doses contributed by all formulations must be
considered.
Nursing Mothers:
LIDODERM has not been studied in nursing mothers. Lidocaine is excreted in human
mild, and the milk: plasma ratio of lidocaine is 0.45 Caution should be exercised
when LIDODERM is admistered to a nursing woman.
Pediatric USE
Safety and effectiveness in pediatric patients have not been established.
ADVERSE REACTIONS
Localized Reactions
During or immediately after treatment with LIDODERM (lidocaine patch 5%), the skin at
the stie of treatment may develop erythema or edema or may be the locus of abnormal
sensation. These reactions are generally mild and transient, resolving
spontaneously within a few minutes to hours. In clinical studies with LIDODERM,
there were no serious reactions reported. One out of 150 subjects in a three-
week study was discontinued from treatment because of a skin reaction
(erythema and hives).
Allergic Reactions:
Allergic and anaphylactoid reactions associated with lidocaine, although rare, can
occur. They are characterized by urticaria, angioedema, bronchospasm, and shock.
If they occur, they should be managed by conventional means. The detection of
sensitivity by skin testing is of doubtful value.
Systemic (Dose-Related) Reactions
Systemic adverse reactions following appropriate use of LIDODERM are likely, due to
the small dose absorbed (See CLINICAL PHARMACOLOGY, Pharmacokinetics), Systemic
adverse effects of lidocaine are similar in nature to those observed with other
PHARMACOLOGY, Pharmacokinetics). Systemic adverse effects oflidocaieare similar in
nature to those observed with other amide local anesthetic agents, including CNS
excitation and/or depression (light-headedness, nervousness, apprehension, twitching,
tremors, convulsions, unconsciousness, respiratory depression and arrest).
Excitatory CNS reactions may be brief or not occur at all, in which case the
first manifestation may be drowsiness merging into unconsciousness. Cardiovascular
manifestations may include bradycardia, hypotension and cardiovascular collapse
leading to arrest.
OVERDOSAGE:
Lidocaine overdose from cutaneous absorption is rare, but could occur. If there is
any suspicion of lidocaine overdose (see ADVERSE REACTIONS, Systemic Reactions), drug
blood concentration should be checked. The management of overdose includes close
monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible
value in the treatment of acute overdose with lidocaine.
In the absence of massive topical overdose or oral ingestion, evaluation of symptoms
of toxicity should include consideration of other etiologies for the clinical effects,
or over dosage from other sources of lidocaine or other local anesthetics.
The oral LD50 of lidocaine HCI is 459 (346-773) mg/kg (as the salt) in non-fasted
female rats and 214 (159-324) mg/kg (as the salt) in fasted female rats, which are
equivalent to roughly 4000 mg, respectively, in a 60 to 70 kg man based on the
equivalent surface area dosage conversion factors between species.
DOSAGE AND ADMINISTRATION:
Apply LIDODERM to intact skin to cover the most painful areas. Apply up to three
patches, only once for up to 12 hours within a 24-hour period. Patches may be cut
into smaller sizes with scissors prior to removal of the release liner. Clothing
may be worn over the area of application. Smaller areas of treatment are recommended
in a debilitated patient, or a patient with impaired elimination.
If irritated or a burning sensation occurs during application, remove the patch(es)
and do not reapply until the irritation subsides.
When LIDODERM is used concomitantly with other products containing local enesthetic
agents, the amount absorbed from all formulations must be considered.
HANDLING AND DISPOSAL:
Hands should be washed after the handling of LIDODERM, and eye contact with LIDODERM
should be avoided. The used patch should be immediately disposed of in such a way
as to prevent its access by children and pets.
HOW SUPPLIED:
LIDODERM (Lidocaine patch 5%) is available as the following:
Carton of 30 patches, packaged into individual child-resistant envelopes
Store at 25C (77 degrees) excursions permitted to 15 to 30 Celsius (59 degree to
86 degree farenheight) See USP Controlled Room Temperature).
Manufactured for:
Endo Pharmaceutical Inc. ENDO
Chadds Ford, Pennsylvania 19317
LIDODERM is a Registered Trademark of Hind Health Care, INC.
=============================================================================
A pressure point procedure found on the internet to help another patient
of piriformis problems in which the Piriformis Muscle needed to be stretched
out back to its original length -- Here is the therapy for that below:
=============================================================================
Sciatica? Piriformis? This helped me 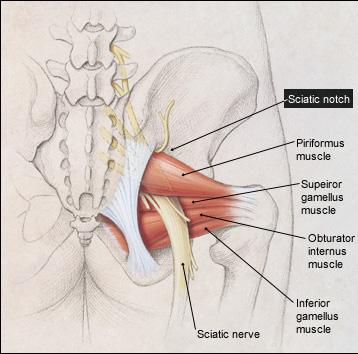
 =================================================================================
(April 8, 2005)
Email to Paul Dean from Northern California Sufferer:
hi,
I have had a neurogram and it shows that both my sciatic nerves are being pinched
at the sciatic notch. Is their any advise you could give me. I live in Northern
California and the doctors up here pretty much suck and really don't believe
piriformis syndrome exists. who did you do to and what tests did you do to determine
you had piriformis syndrome.
THANKS
==================================================================================
Piriformis Surgery Incision (Site)
Of a Patient Suffering from Left Side
Piriformis Syndrome and Sciatica
=================================================================================
(April 8, 2005)
Email to Paul Dean from Northern California Sufferer:
hi,
I have had a neurogram and it shows that both my sciatic nerves are being pinched
at the sciatic notch. Is their any advise you could give me. I live in Northern
California and the doctors up here pretty much suck and really don't believe
piriformis syndrome exists. who did you do to and what tests did you do to determine
you had piriformis syndrome.
THANKS
==================================================================================
Piriformis Surgery Incision (Site)
Of a Patient Suffering from Left Side
Piriformis Syndrome and Sciatica
 The incision is to the Buttock
(April 8, 2005)
Email Reply From Paul Dean to Northern California Sufferer:
The nerve narrowing at the sciatic notch is a different part of the body and
is near the spinal cord and structure which (IS NOT) Piriformis Syndrome, which
lies deep underneith the Buttock underneith your gluteal muscles. Your Sciatic
notch may need to be enlargened because it should not be pinching any of the
nerves. Nerves need to move freely as they are stretched in walking, etc. If
they cannot move or if they are pinched, you will be in great pain.
It is very hard to find a doctor who knows where your pain is coming from. Especially
in Piriformis Syndrome. A Orthopaedic doctor can go an entire career without
seeing more than one or two cases of Piriformis Syndrome in his career.
Call Dr. Chambi, (Neurosurgeon) (714)-973-0810 and explain your situation to him.
He is the only one who could find my problem of many, doctors who had seen me.
In my case, the Piriformis muscle had scar tissue wrapped around the sciatic nerve,
entrapping that nerve and giving me pain. That scar tissue has been removed by
Dr. Chambi and I am getting good results, but it takes time for a sciatic nerve to
get back to normal.
Good luck, I feel for all of those who have had the intense pain that I have had!
As a final comment. I chose the Doctor that the Pro Athletes prefer, because you
need the best of the best for good results.
I am a patient recovering like yourself and every situation will be different and
your exact situation sounds a little bit different than mine.
The diagnosis of Piriformis Syndrome is a situation of exclusion of any Spinal
problems. Also, if your pain lies in the middle of your buttock and comes about
when you are sitting, this is one sign that you may have Piriformis Syndrome.
You could have numbess, Sharp stabbing Pain, burning pain, or Aching Pain, along
with sciatica.
When it is found that your problem is not coming from the spine, then the surgeon
will look else where for the problem. The situation becomes confusing when the
spine has exactly the same symptoms of the Piriformis entrapment, (In my case,
sciatica down the right leg). This is when the MRI will exclude any type of
abnormal discs that may have ruptured or narrowed or had entrapped the nerve.
I am post disc surgery and post Piriformis Release surgery at this time. As
long as you have entrapment, no amount of exercise or stretches are going to
change that entrapment. It is after these failed exercises and stretches that
one may go for a release surgery.
As a last note, find the very best neurosurgeon that you can, (even if it means flying
to that doctor) who is familiar with your diagnosis and possible surgery solutions.
Different Doctors specialize in different things and they don't know much about
other conditions and they only look at what they know. A spine surgeon only
likes to give spine surgeries... etc. etc. So you really need a specialist who
deals with your type of problem all day long and I think you are on the right
track. Your age and type of fall that you might of had would also help in diagnosis
of your injury. Family history and many other questions are needed to be
answered to get to the bottom of your situation. Your body will give you
an idea of where the pain is coming from which is helpful in the diagnosis.
Hope some of the above helps you! See a good Neurosurgeon to confirm
any of the above I have mentioned. Of course I cannot prescribe or give advice
because I am not a Doctor. But I guess everybody has an opinion.
Thanks,
Paul, Recovering Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
=============================================================================
Piriformis Surgery Questions and Answers:
The incision is to the Buttock
(April 8, 2005)
Email Reply From Paul Dean to Northern California Sufferer:
The nerve narrowing at the sciatic notch is a different part of the body and
is near the spinal cord and structure which (IS NOT) Piriformis Syndrome, which
lies deep underneith the Buttock underneith your gluteal muscles. Your Sciatic
notch may need to be enlargened because it should not be pinching any of the
nerves. Nerves need to move freely as they are stretched in walking, etc. If
they cannot move or if they are pinched, you will be in great pain.
It is very hard to find a doctor who knows where your pain is coming from. Especially
in Piriformis Syndrome. A Orthopaedic doctor can go an entire career without
seeing more than one or two cases of Piriformis Syndrome in his career.
Call Dr. Chambi, (Neurosurgeon) (714)-973-0810 and explain your situation to him.
He is the only one who could find my problem of many, doctors who had seen me.
In my case, the Piriformis muscle had scar tissue wrapped around the sciatic nerve,
entrapping that nerve and giving me pain. That scar tissue has been removed by
Dr. Chambi and I am getting good results, but it takes time for a sciatic nerve to
get back to normal.
Good luck, I feel for all of those who have had the intense pain that I have had!
As a final comment. I chose the Doctor that the Pro Athletes prefer, because you
need the best of the best for good results.
I am a patient recovering like yourself and every situation will be different and
your exact situation sounds a little bit different than mine.
The diagnosis of Piriformis Syndrome is a situation of exclusion of any Spinal
problems. Also, if your pain lies in the middle of your buttock and comes about
when you are sitting, this is one sign that you may have Piriformis Syndrome.
You could have numbess, Sharp stabbing Pain, burning pain, or Aching Pain, along
with sciatica.
When it is found that your problem is not coming from the spine, then the surgeon
will look else where for the problem. The situation becomes confusing when the
spine has exactly the same symptoms of the Piriformis entrapment, (In my case,
sciatica down the right leg). This is when the MRI will exclude any type of
abnormal discs that may have ruptured or narrowed or had entrapped the nerve.
I am post disc surgery and post Piriformis Release surgery at this time. As
long as you have entrapment, no amount of exercise or stretches are going to
change that entrapment. It is after these failed exercises and stretches that
one may go for a release surgery.
As a last note, find the very best neurosurgeon that you can, (even if it means flying
to that doctor) who is familiar with your diagnosis and possible surgery solutions.
Different Doctors specialize in different things and they don't know much about
other conditions and they only look at what they know. A spine surgeon only
likes to give spine surgeries... etc. etc. So you really need a specialist who
deals with your type of problem all day long and I think you are on the right
track. Your age and type of fall that you might of had would also help in diagnosis
of your injury. Family history and many other questions are needed to be
answered to get to the bottom of your situation. Your body will give you
an idea of where the pain is coming from which is helpful in the diagnosis.
Hope some of the above helps you! See a good Neurosurgeon to confirm
any of the above I have mentioned. Of course I cannot prescribe or give advice
because I am not a Doctor. But I guess everybody has an opinion.
Thanks,
Paul, Recovering Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
=============================================================================
Piriformis Surgery Questions and Answers:
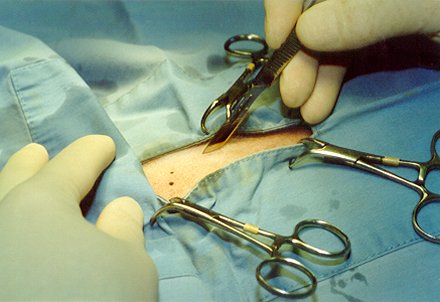 (April 8, 2005) Email Questions to Paul Dean
An Email to Paul Dean from another Person who is considering
Piriformis Release Surgery:
Hello Mr. Dean,
While researching piriformis syndrome on the internet, I ran across your account
of having release surgery done by Dr. Chambi.
My wife is having a great deal of sciatica pain and is currently seeing Dr. Chambi
for piriformis syndrome. After 2 injections with little relief of pain, Dr Chambi
has suggested that surgery might be in order.
Given what you know about this surgery, was it successful in relieving your pain
and would you have Dr Chambi perform it again?
I would be very interested in talking to you further about this subject if you
would consent.
==================================================================================
==================================================================================
Piriformis Surgery Steps:
(April 8, 2005) Email Questions to Paul Dean
An Email to Paul Dean from another Person who is considering
Piriformis Release Surgery:
Hello Mr. Dean,
While researching piriformis syndrome on the internet, I ran across your account
of having release surgery done by Dr. Chambi.
My wife is having a great deal of sciatica pain and is currently seeing Dr. Chambi
for piriformis syndrome. After 2 injections with little relief of pain, Dr Chambi
has suggested that surgery might be in order.
Given what you know about this surgery, was it successful in relieving your pain
and would you have Dr Chambi perform it again?
I would be very interested in talking to you further about this subject if you
would consent.
==================================================================================
==================================================================================
Piriformis Surgery Steps:
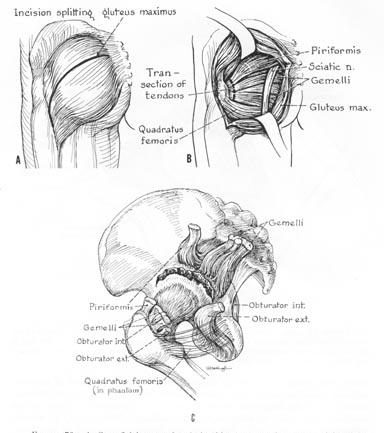 Email Answer from Paul Dean: (April 8, 2005)
Dear Sir,
Yes I did the Buttock Lidocaine shots and only the first of a series of three
helped me. I was still in a lot of pain and the only alternative at that point
was the actual Piriformis Release Surgery.
I had worn out the physical therapy option, and wasn't getting any better.
It was either have the pirifromis release surgery or always be in terrible pain.
I did not want to live the rest of my life in terrible pain so I went for the
piriformis release surgery.
Within two months after the surgery I was ALOT better. That alone helped me
very much, and my depression started to lift as well. When a person is injured
for a long time it is very hard to keep a positive frame of mind, but this
is essential in getting better.
Nerve
Email Answer from Paul Dean: (April 8, 2005)
Dear Sir,
Yes I did the Buttock Lidocaine shots and only the first of a series of three
helped me. I was still in a lot of pain and the only alternative at that point
was the actual Piriformis Release Surgery.
I had worn out the physical therapy option, and wasn't getting any better.
It was either have the pirifromis release surgery or always be in terrible pain.
I did not want to live the rest of my life in terrible pain so I went for the
piriformis release surgery.
Within two months after the surgery I was ALOT better. That alone helped me
very much, and my depression started to lift as well. When a person is injured
for a long time it is very hard to keep a positive frame of mind, but this
is essential in getting better.
Nerve
 Now 10 months later I continue to improve. I could not improve at all without the
piriformis release surgery. What happened is when I fell at work, a large amount
of scarring was attached to the piriformis muscle area and to the sciatic nerve
making it impossible for the nerve to move. If the sciatic nerve cannot move, you
will have terrible pain.
Yes, I was scared to have the release, but not as scared as when I had my
back surgery.
Would I do it again? Every day of the week, I would. Quality of life is very important
to me and I need to be able to be active as I once was and now I have the opportunity
to get back to being active.
Piriformis Syndrome is very rare and most Doctors know nothing about it. You have
a doctor, Dr. Chambi, who understands this condition, so you are very lucky to find
somebody who understands where your pain is actually coming from.
Post Op: I have lost a great deal of elasticity in the nerve so I must walk and
stretch every day to regain what I can in that sciatic nerve elasticity.
Rehab. is very important and takes a long time to get the nerve back into
shape. Stretching, Walking and Light water exercises.
Structure Of A Nerve
Now 10 months later I continue to improve. I could not improve at all without the
piriformis release surgery. What happened is when I fell at work, a large amount
of scarring was attached to the piriformis muscle area and to the sciatic nerve
making it impossible for the nerve to move. If the sciatic nerve cannot move, you
will have terrible pain.
Yes, I was scared to have the release, but not as scared as when I had my
back surgery.
Would I do it again? Every day of the week, I would. Quality of life is very important
to me and I need to be able to be active as I once was and now I have the opportunity
to get back to being active.
Piriformis Syndrome is very rare and most Doctors know nothing about it. You have
a doctor, Dr. Chambi, who understands this condition, so you are very lucky to find
somebody who understands where your pain is actually coming from.
Post Op: I have lost a great deal of elasticity in the nerve so I must walk and
stretch every day to regain what I can in that sciatic nerve elasticity.
Rehab. is very important and takes a long time to get the nerve back into
shape. Stretching, Walking and Light water exercises.
Structure Of A Nerve
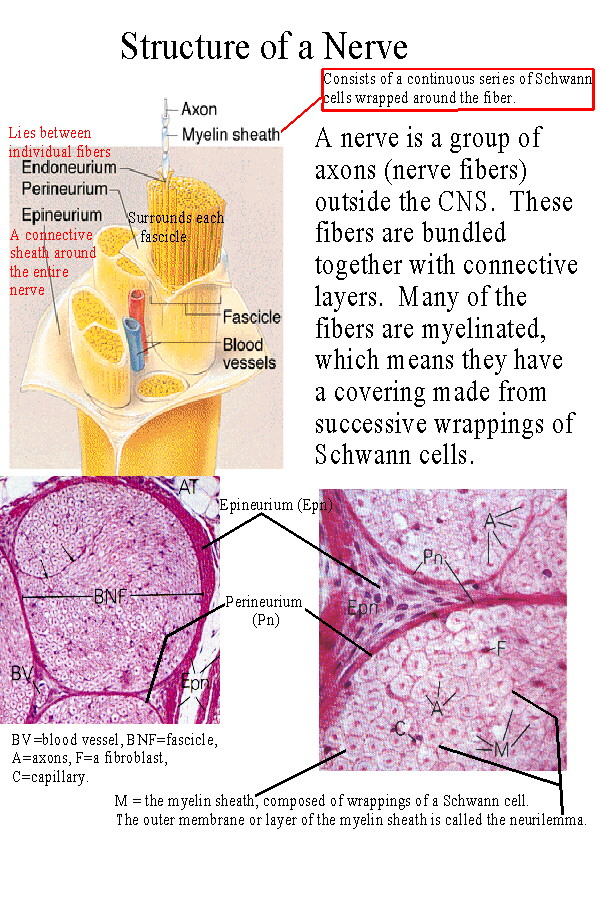 A final note:
I was at the point where I felt I had nothing to lose so I went ahead with the surgery,
and it helped a great deal. My L5 S1 Lower discectomy surgery also helped me very
much. (I had a 7mm Herniated Disk)
Good luck to you and your wife, and again, think of quality of life, and of getting
better because sometimes physical therapy will do you no good when the scarring is so
severe that your sciatic nerve cannot move.
I am up to walking an hour and the extreme edge of pain is gone!!!
Of course I am not a Doctor so I cannot give advise but only opinions as to my
unique situation, and every situation is different.
Dr. Chambi is the doctor that all the Pro Athletes choose and there must be a reason
for that.
Take care,
I hope that you recover soon!
Paul Dean, Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
==================================================================================
Side Note: July 23, 2005 - Paul Dean
I am continuing to recover at my own body's rate which seems to be a little bit
slow but you really can't recover at any pace faster than your own natural
pace of healing. Nerves take up to three years to have their full healing ability.
So do not be to impatient if the second you get off the operating table that you
are not completely healed. That just isn't how nerves work if they have been damaged
for a long time. The problem is that once your sciatic nerve in your hip has
been entrapped at the piriformis level for several years, the elasticy shrinks
and you will hurt every time you stretch until you get your nerve elasticy back.
This is the reason that you need to walk an hour or more every day to get that
elasticty back. It will hurt to walk long distances and that is why I use the
Lidocaine patch. This patch numbs the area that hurts in the back of the hip,
so you can walk further and stretch the sciatica nerve.
Rubber band Analogy:
I can imagine a rubber band that needs another inch or two in order to reach
its full potential of stretch. So every day I walk, and then I walk some more,
stretching that rubber band, which is the sciatic nerve. Once the nerve is used
to the stretch it doesn't hurt as much. Of course this is done after the
surgery because the sciatic nerve could not stretch at all when it was tethered
down from tissues wrapped around it from a fall accident I had from work. Now
that there is no entrapment of the nerve I am gently stretching that nerve
until it gets used to the stretch and stops hurting when I walk. The goal
is to have absolutely no pain no matter what I am doing and that is my eventual
goal.
Vitamins B1 and B12 and Antioxidants to build up the Immunity and Healing:
What about boosting the immunity system to have a faster healing process?
I am on a Vitamin Regiment of B1 Vitamin and B12 Vitamin in decent doses as
well as an Anti-oxidant supplement to get my system in good working order so
that I can heal as fast as possible.
I have tried to increase the rate of healing by getting toxins out of my
system by doing the following:
Do's:
Vitamin B (B1) (B12) Vitamin A,B,C,E Beta Carotene and Mineral Supplements.
Drink Six glasses of water a day
Drink as much Grapefruit juice (no Sugar) as possible
Eat as many raw fruits and vegetables as possible
Chicken and Fish
Dont's:
No Salt and No Sugar need to be eaten it is in your foods already.
No Greasy Processed Foods
No Fast-food
No Breads or rice or potatoes
Please see a Doctor before using these above techniques which I am
following as your medications may require that you do not follow
my above plan for getting your system back into shape for quicker healing.
Note: These above Do's and Don'ts can be found in the book of President Clintons
Doctor: Michael F. Roizen, MD. and Mehmet C. Oz, MD copyright 2005,
"YOU, THE OWNER'S MANUAL", The insider's guide to the body that will make
you healthier and younger. Harpercollins Publishers Inc, 10 East 53rd Street
New York, NY 10022.
I have no affiliation with any of these works and please take all information
as third party opinion and review options with your Doctors before doing
anything with your body. Thank you.
Above Updated: April 8, 2005
------------------------------------------------------------------------------
--------------------------------------------------------------------------------
New Entry: July 25, 2007 - Updated Medical Condition of Post Piriformis Syndrome
with Piriformis Release Surgery and Post Discectomy of L5 S1 Disc.
--------------------------------------------------------------------------------
Email Response to Susan:
--------------------------------------------------------------------------------
July 25, 2007
Hi Susan, (Disclaimer: I am a patient like yourself and am not a Doctor.)
Thank you for reading all of my postings, I'm sure it must have taken awhile to get
through it all. Pain is an interesting thing, in makes you want to read every single
thing you can find out about your pain hoping that you can some how stumble upon the
right information that can give you some pain relief. That is what I did and I am sure
that is also what you are seeking and I am wishing you the best of luck in advance, as
pain can control and ruin a good life that was before pain free.
Susan wrote:
The last update on your progress was quite some time ago. How is the sitting going
now?
Paul's reply:
Yes, the update was quite a while ago mostly because I have been busy back in the
Tradeshow business, which requires lifting heavy amounts of weight for a duration of
time. So, in part I have to say that I have gotten better, because it was unfathomable
before my piriformis surgery that I would be able to excel in either of my heavy lifting
jobs. Lifting in duration and for long periods of time was difficult to impossible
before my surgery. Now to answer the sitting question which is important because my
travel time to and from work is an hour and a half each way most of the time. I still
have pain, but not extreme pain and I can get out of it by putting my car on cruise
control and taking my right leg out of the stretch that is required to press down the
gas peddle. I use cruise control most of the time because my pain is elevated. So now
the next question is how much has my pain level improved since the surgery.
I would say it has gone from a 7 to 8 in pain level down to a 2 and 3 which has given
my life back to me in many ways as I enjoy physical activity with lifting and movies
which last up to 3 hours. I do have problems with movies over 2 hours and will take a
15 minute walk around the lobby during a movie in order to stop my pain. It seems that
almost instantly when the leg is no longer in a bad position of a stretch or just
sitting to long in the theater, the walking relieves the pain instantly. Where is the
pain in the first place, it seems that it is in the thigh area, but before the surgery
I had both buttock an thigh pain. Would I do the surgery over again? Definitely, yes as
my pain levels went down to a livable tolerance level. I am still cautious as to getting
back into tennis as that does a lot of thigh stretching but I will try to see if I can
slowly work back into this great sport that I have loved.
Susan wrote:
I'm at the "I need surgery" stage and am trying to find the best, most experienced
surgeon. I live in Florida and am having a difficult time finding someone in this
area who might be competent to do this specialized procedure. It seems that your
doctor and
A final note:
I was at the point where I felt I had nothing to lose so I went ahead with the surgery,
and it helped a great deal. My L5 S1 Lower discectomy surgery also helped me very
much. (I had a 7mm Herniated Disk)
Good luck to you and your wife, and again, think of quality of life, and of getting
better because sometimes physical therapy will do you no good when the scarring is so
severe that your sciatic nerve cannot move.
I am up to walking an hour and the extreme edge of pain is gone!!!
Of course I am not a Doctor so I cannot give advise but only opinions as to my
unique situation, and every situation is different.
Dr. Chambi is the doctor that all the Pro Athletes choose and there must be a reason
for that.
Take care,
I hope that you recover soon!
Paul Dean, Patient (Dr. Chambi (714)-973-0810 Santa Ana, CA )
==================================================================================
Side Note: July 23, 2005 - Paul Dean
I am continuing to recover at my own body's rate which seems to be a little bit
slow but you really can't recover at any pace faster than your own natural
pace of healing. Nerves take up to three years to have their full healing ability.
So do not be to impatient if the second you get off the operating table that you
are not completely healed. That just isn't how nerves work if they have been damaged
for a long time. The problem is that once your sciatic nerve in your hip has
been entrapped at the piriformis level for several years, the elasticy shrinks
and you will hurt every time you stretch until you get your nerve elasticy back.
This is the reason that you need to walk an hour or more every day to get that
elasticty back. It will hurt to walk long distances and that is why I use the
Lidocaine patch. This patch numbs the area that hurts in the back of the hip,
so you can walk further and stretch the sciatica nerve.
Rubber band Analogy:
I can imagine a rubber band that needs another inch or two in order to reach
its full potential of stretch. So every day I walk, and then I walk some more,
stretching that rubber band, which is the sciatic nerve. Once the nerve is used
to the stretch it doesn't hurt as much. Of course this is done after the
surgery because the sciatic nerve could not stretch at all when it was tethered
down from tissues wrapped around it from a fall accident I had from work. Now
that there is no entrapment of the nerve I am gently stretching that nerve
until it gets used to the stretch and stops hurting when I walk. The goal
is to have absolutely no pain no matter what I am doing and that is my eventual
goal.
Vitamins B1 and B12 and Antioxidants to build up the Immunity and Healing:
What about boosting the immunity system to have a faster healing process?
I am on a Vitamin Regiment of B1 Vitamin and B12 Vitamin in decent doses as
well as an Anti-oxidant supplement to get my system in good working order so
that I can heal as fast as possible.
I have tried to increase the rate of healing by getting toxins out of my
system by doing the following:
Do's:
Vitamin B (B1) (B12) Vitamin A,B,C,E Beta Carotene and Mineral Supplements.
Drink Six glasses of water a day
Drink as much Grapefruit juice (no Sugar) as possible
Eat as many raw fruits and vegetables as possible
Chicken and Fish
Dont's:
No Salt and No Sugar need to be eaten it is in your foods already.
No Greasy Processed Foods
No Fast-food
No Breads or rice or potatoes
Please see a Doctor before using these above techniques which I am
following as your medications may require that you do not follow
my above plan for getting your system back into shape for quicker healing.
Note: These above Do's and Don'ts can be found in the book of President Clintons
Doctor: Michael F. Roizen, MD. and Mehmet C. Oz, MD copyright 2005,
"YOU, THE OWNER'S MANUAL", The insider's guide to the body that will make
you healthier and younger. Harpercollins Publishers Inc, 10 East 53rd Street
New York, NY 10022.
I have no affiliation with any of these works and please take all information
as third party opinion and review options with your Doctors before doing
anything with your body. Thank you.
Above Updated: April 8, 2005
------------------------------------------------------------------------------
--------------------------------------------------------------------------------
New Entry: July 25, 2007 - Updated Medical Condition of Post Piriformis Syndrome
with Piriformis Release Surgery and Post Discectomy of L5 S1 Disc.
--------------------------------------------------------------------------------
Email Response to Susan:
--------------------------------------------------------------------------------
July 25, 2007
Hi Susan, (Disclaimer: I am a patient like yourself and am not a Doctor.)
Thank you for reading all of my postings, I'm sure it must have taken awhile to get
through it all. Pain is an interesting thing, in makes you want to read every single
thing you can find out about your pain hoping that you can some how stumble upon the
right information that can give you some pain relief. That is what I did and I am sure
that is also what you are seeking and I am wishing you the best of luck in advance, as
pain can control and ruin a good life that was before pain free.
Susan wrote:
The last update on your progress was quite some time ago. How is the sitting going
now?
Paul's reply:
Yes, the update was quite a while ago mostly because I have been busy back in the
Tradeshow business, which requires lifting heavy amounts of weight for a duration of
time. So, in part I have to say that I have gotten better, because it was unfathomable
before my piriformis surgery that I would be able to excel in either of my heavy lifting
jobs. Lifting in duration and for long periods of time was difficult to impossible
before my surgery. Now to answer the sitting question which is important because my
travel time to and from work is an hour and a half each way most of the time. I still
have pain, but not extreme pain and I can get out of it by putting my car on cruise
control and taking my right leg out of the stretch that is required to press down the
gas peddle. I use cruise control most of the time because my pain is elevated. So now
the next question is how much has my pain level improved since the surgery.
I would say it has gone from a 7 to 8 in pain level down to a 2 and 3 which has given
my life back to me in many ways as I enjoy physical activity with lifting and movies
which last up to 3 hours. I do have problems with movies over 2 hours and will take a
15 minute walk around the lobby during a movie in order to stop my pain. It seems that
almost instantly when the leg is no longer in a bad position of a stretch or just
sitting to long in the theater, the walking relieves the pain instantly. Where is the
pain in the first place, it seems that it is in the thigh area, but before the surgery
I had both buttock an thigh pain. Would I do the surgery over again? Definitely, yes as
my pain levels went down to a livable tolerance level. I am still cautious as to getting
back into tennis as that does a lot of thigh stretching but I will try to see if I can
slowly work back into this great sport that I have loved.
Susan wrote:
I'm at the "I need surgery" stage and am trying to find the best, most experienced
surgeon. I live in Florida and am having a difficult time finding someone in this
area who might be competent to do this specialized procedure. It seems that your
doctor and